It happens that in the maternity hospital or a little later, at an appointment with a pediatrician, a newborn child is given complex diagnoses regarding the state of the central nervous system (CNS). What is hidden behind the words “hypertensive-hydrocephalic syndrome” or “vegetative-visceral dysfunction syndrome” and how can these conditions affect the health and development of a child? Is it possible to treat CNS lesions? Child rehabilitation specialist Natalya Pykhtina, head of the clinic of the same name, tells the story.
The doctor receives the first information about the state of the newborn’s central nervous system in the first minutes and hours after the baby is born, still in the delivery room. Everyone has heard about the Apgar score, which evaluates a child's vitality based on five main visible signs - heartbeat, skin color, breathing, reflex excitability and muscle tone.
Why is it important to correctly assess a baby’s motor activity? Because it provides information about the state of the spinal cord and brain, their functionality, which helps to recognize in time both minor deviations and serious pathologies.
Thus, the greatest attention is paid to the degree of symmetry of the movements of the limbs: their pace and volume should be the same on both sides, that is, on the left arm and left leg and the right arm and leg, respectively. Also, the doctor conducting the initial examination of the newborn takes into account the clarity and severity of unconditioned reflexes. This is how the pediatrician receives information about the activity of the baby’s central nervous system and finds out whether it is functioning within normal limits.
Lesions of the central nervous system: at what stages of pregnancy?
Damage to the central nervous system in a child occurs in two ways - in utero or during childbirth.
If developmental abnormalities occur in the fetus during the embryonic stage of intrauterine development, they often turn into defects that are incompatible with life, or are extremely severe and cannot be treated or corrected. If a damaging effect was exerted on the fetus after the eighth week of pregnancy , this will not affect the child in the form of gross deformity, but may well cause minor deviations that will have to be treated after birth. The negative impact on the fetus in the later stages - after the twenty-eighth week of pregnancy - will not manifest itself in the form of defects at all, but can become a catalyst for the occurrence of diseases in a normally formed child.
It is very difficult to predict which specific negative factor and at what stage of pregnancy will cause irreparable damage to the fetus. Therefore, the expectant mother needs to be extremely careful and monitor her health even before the moment of conception. Preparing for pregnancy is an important stage of family planning, because the child’s health can be affected by both the bad habits of the mother and her chronic diseases, hard work and unhealthy psychological state.
How exactly he is born is also important for the child’s future life. It is at the moment of birth that there is a danger of damage in the second way - intranatally. Any incorrect intervention or, conversely, lack of timely assistance is highly likely to have a negative impact on the baby. At risk are premature birth, as well as birth at the scheduled time, but rapid or, conversely, protracted.
The main causes of central nervous system damage in newborns are oxygen starvation, which leads to hypoxia, and birth trauma. Less obvious and diagnosable causes are less common: intrauterine infections, hemolytic disease of the newborn, malformations of the brain and spinal cord, hereditary metabolic disorders or chromosomal pathology.
Doctors identify several syndromes of central nervous system pathology in newborns.
Degrees of severity and characteristic symptoms
Hypoxic-ischemic encephalopathy has 3 degrees of severity, which are characterized by their own manifestations. Using them, doctors often give a preliminary description of brain damage and an approximate prognosis.
Mild degree
With this degree the patient will have:
- the pupil is dilated and the eyelids are wide open;
- lack of concentration;
- impaired coordination of movements, wandering behavior;
- either drowsiness or hyperexcitability was detected;
- high degree of irritability;
- lack of appetite;
- cerebral circulation is impaired.
Average degree
Neurology with it will be more pronounced, since the disturbance in oxygen saturation of the brain is longer lasting:
- the baby has spontaneous cries for no reason;
- the protective and support reflex is either weakened or absent altogether;
- signs of muscle weakness;
- drooping upper eyelid;
- increased cerebrospinal fluid pressure;
- metabolic acidosis of the blood;
- neuralgic attacks;
- failure in the swallowing process.
Severe degree
The damage in such cases is more severe, which manifests itself in:
- convulsions;
- bluish skin;
- loss of consciousness;
- hypertension;
- lack of motor abilities;
- strabismus;
- coma or precoma;
- lack of pupil reaction to light;
- failure of the respiratory process with severe arrhythmia;
- tachycardia.
PEP is a type of hypoxic-ischemic encephalopathy in young children. It is diagnosed both immediately after birth and in the first year of life. PEP develops both in utero, during labor, and in the first 10 days from birth.
It can be of three degrees of severity with characteristic symptoms and occur in an acute form - up to a month, with early restoration of functions - up to 4 months, with late recovery - up to 2 years.
- Arthritis 3 degrees
Increased intracranial pressure: symptoms
Hypertensive-hydrocephalic syndrome is an excessive accumulation of cerebrospinal fluid in the ventricles and under the meninges. To identify this syndrome in an infant, an ultrasound scan of the brain is performed and data on increased intracranial pressure are recorded (according to echoencephalography - EEG).
In pronounced severe cases of this syndrome, the size of the brain part of the skull increases disproportionately. As is known, children are born with mobile bones of the skull, which fuse during development, therefore, with a unilateral pathological process of this syndrome, divergence of cranial sutures, thinning of the skin in the temporal lobe and increased venous pattern on the scalp will be observed.
If a child has increased intracranial pressure, he will be restless, irritable, easily excitable and whiny. Also, the baby will sleep poorly, roll his eyes and throw his head back. Graefe's symptom (a white stripe between the pupil and the upper eyelid) may occur. In more severe cases, there may also be a symptom of the so-called “setting sun”, in which the iris of the eye, like the sun at sunset, is half submerged under the lower eyelid. Convergent strabismus also sometimes appears.
With reduced intracranial pressure, on the contrary, the child will be inactive, lethargic and drowsy. Muscle tone in this case is unpredictable - it can be either increased or decreased. The baby may stand on tiptoes when supported, or cross his legs when trying to walk, while the baby’s support, crawling and walking reflexes will be reduced. Seizures can also often occur.
Ischemic cochleovestibular syndromes: algorithm for diagnosis and complex therapy
Ischemic cochleovestibular syndromes (ICVS) are one of the most common causes of dizziness and develop in the presence of circulatory failure in the arteries supplying the inner ear and the root of the VIII nerve, as well as the vestibular nuclei and pathways.
The article proposes an algorithm for diagnosing ischemic cochleovestibular syndromes and describes the principles of treatment of patients with ICVS. Oxidative stress plays a special role in the clinical and morphological picture of ischemia. Using Actovegin as an example, the possibilities of including drugs with neurometabolic effects that improve the survival of neurons under conditions of chronic hypoxia into ICS therapy are considered.
MRI – magnetic resonance imaging; Ultrasound – ultrasound examination; ECG – electrocardiography; EEG – electroencephalography.
Dizziness is one of the most common causes of loss of balance and complaints among patients visiting general practitioners [1]. Dizziness is very often caused by ischemic cochleovestibular syndromes (ICVS), which are a combination of vestibular disorders (dizziness, unsteadiness) with tinnitus and hearing loss. ICVS develops in the presence of circulatory failure in the arteries supplying the inner ear and the VIII nerve root [2], which is caused by increasing manifestations of general cerebral ischemia, chronic cerebral vascular insufficiency and steal syndromes [1, 3–5].
There are peripheral and central cochleovestibular syndromes. Peripheral ICVS is associated with circulatory failure in the small arteries supplying the labyrinth and the VIII nerve [6, 7]. Central cochleovestibular syndrome occurs as a result of ischemia of the vestibular nuclei located in the brain stem [8, 9]. The etiological factors for the development of dizziness in these cases are atherosclerotic damage to extra- and intracranial cerebral vessels (stenosis, occlusion), arterial hypertension, deformation of the vertebral arteries, anomalies of the arteries of the vertebral-basilar system, disorders of hemorheology and hemostasis, arterio-arterial and cardiac embolisms, thrombosis venous sinuses, disturbance of central hemodynamic parameters [10, 11].
Dizziness often occurs with brain tumors, epilepsy, degenerative diseases of the central nervous system, as well as with metabolic disorders (primarily diabetes mellitus, in which the blood circulation of the inner ear is impaired), cognitive disorders, anxiety disorders, and degenerative diseases of the cervical spine. The pathogenesis of all ischemic cochleovestibular syndromes is based on local and cerebral hemodynamic disorders, entailing various forms of functional disorders of the vestibular system. Pathogenetic factors in the development of ICVS are ischemia, disruption of the trophism of labyrinth receptors and labyrinth-dependent brain structures and metabolism as a result of cerebral vascular diseases of various origins and, as a consequence, secondary encephalopathic disorders [12, 13].
It can be assumed that in the pathogenesis of acute ICVS, an important role is played by the obstruction of venous outflow from the transverse sinus during a hypertensive crisis as a result of the opening of arteriole-venous shunts. Often in such patients, “secondary” hydrops of the labyrinth is detected, which is caused by impaired circulation of the inner ear against the background of impaired venous outflow from the cranial cavity and/or external hydrocephalus. Hemolytic fluid dynamics disorders are aggravated by an increase in the activity of lipid peroxidation, a decrease in the main indicators of the antioxidant system, changes (like hypercoagulation) in blood rheology and lipid metabolism indicators. However, an indisputable fact is that the development of cerebrovascular diseases is based on changes in the metabolism and trophism of neurons and neurotransmitter systems [5, 10, 14]. Disturbances in metabolic and protein synthetic processes in the vascular wall and neurons underlie subsequent morphological damage (atherosclerotic or neurodegenerative in nature), which is the foundation for the further development and manifestation of the disease. Equally important is the disruption of neurohumoral regulation processes, in particular neurotransmitter systems, vascular tone and adaptive capabilities of the vascular bed [3]. Depending on the nature of the vascular changes, the pathological focus can be localized both in the “periphery” (in the labyrinth) and at any level of the brain, which is clinically manifested by peripheral and central labyrinthine syndrome.
Symptoms of ICVS have age-related characteristics [15]. This is due to the fact that in old age it is difficult to single out one cause for the development of ICVS; hypercholesterolemia, bending of one or both vertebral arteries, atherosclerotic stenosis (often hemodynamically insignificant) of the internal carotid arteries, and the presence of degenerative changes in the spine can lead to ICVS [16 ]. In elderly and senile age, multiplicity and recurrence of acute ischemic strokes are often observed, especially in the vertebrobasilar system. Clinically, this is manifested by frequent attacks of dizziness, nystagmus, balance and coordination disorders. Chronic cerebral ischemia is reflected by changes in the white matter (leukoaraiosis), primarily in the deep parts of the brain. In elderly patients, a relationship has been identified between the prevalence of leukoaraiosis, especially in the anterior parts of the brain, the localization of lacunar lesions in the lenticular nucleus and the severity of walking and balance disorders [13]. In patients with cognitive disorders, it is difficult to collect a correct history and differentiate complaints, so diagnosing ICVS in this group of patients is difficult.
Diagnosing ICVS in general is challenging. On the one hand, dizziness in different diseases can occur identically, on the other hand, it can have a different clinical picture for the same disease. For example, in outpatients with dizziness, the cause of dizziness is identified only in 20% of cases [4]. In order to make the correct diagnosis and prescribe optimal treatment to the patient, the doctor must adhere to a certain diagnostic algorithm (Fig.).
Research methods for ICVS
First of all, it is necessary to carefully examine the patient, including a detailed history taking and analysis of complaints in order to determine the type of dizziness. Measure blood pressure in a supine and standing position: with a significant decrease in systolic pressure (more than 20 mm Hg) in an upright position, symptoms similar to those of vertebrobasilar insufficiency are usually caused by orthostatic hypotension. During a neurological examination, attention should be paid to the presence or absence of nystagmus, static or dynamic ataxia. Indicative tests are Romberg (the patient, standing with his eyes closed, deviates in the direction of the labyrinth lesion) and Babinsky-Weil (the patient with his eyes closed takes five steps forward and backward several times - with a unilateral vestibular lesion, his route will be shaped like a star). In elderly patients and patients with a complicated history (abuse of alcohol, toxic substances, drugs), neuropsychological testing should be performed to identify cognitive disorders.
Systemic dizziness
Systemic dizziness is the result of impaired functioning of the vestibular analyzer due to its damage [7, 17]. Proprioceptive systemic vertigo is distinguished (a feeling of passive movement of one’s own body in space or a tactile tactile sensation of support moving under the feet or hands, lifting or sinking of the body, feeling “on a wave,” swaying back and forth, left and right, up and down, “walking like a over bumps") and visual systemic vertigo (a feeling of progressive movement of objects in the field of vision). Depending on the level and depth of the lesion, systemic vertigo is classified as peripheral (damage to the vestibular ganglia, semicircular canals) or as central systemic vertigo (damage to the cerebellum, brain stem and, in particular, the vestibular nuclei or their connections with other components of the central nervous system).
Peripheral systemic vertigo is most often associated with inflammatory diseases of the inner ear, viral lesions, Meniere's disease, trauma or ischemia of the labyrinth [3, 18]. Typically, systemic vertigo is paroxysmal in nature, manifests itself more intensely than central vertigo, and is accompanied by severe vegetative symptoms (nausea, repeated vomiting not associated with food intake, pallor (hyperemia) of the face, hyperhidrosis, etc.). Peripheral systemic vertigo is always accompanied by spontaneous nystagmus - clonic, horizontal or horizontal-rotatory of varying degrees of intensity, associated with a harmonious deviation of the torso and arms towards the slow component.
During the acute onset of an attack, patients feel the apparent movement of objects towards the diseased ear, nystagmus is also directed in the same direction (stage of irritation or irritation of the labyrinth), subsequently (in the stage of inhibition of the labyrinth) - a sensation of apparent movement of objects and the direction of nystagmus towards the healthy ear. The duration of attacks can range from several minutes to several hours. There is a positive effect of turning the head (towards the slow component of nystagmus). As a rule, peripheral vestibular vertigo is caused by a unilateral pathological process and is accompanied by hearing impairment and tinnitus on the affected side [19]. In some cases, hearing impairments are not intense and are more often associated with impaired speech intelligibility. Recurrences of attacks are associated with increases or fluctuations in blood pressure, turns of the head and torso, and changes in body position.
The causes of dizziness of central origin are most often vertebrobasilar insufficiency and trauma [3, 18]. In addition, severe neurological diseases can be the cause of central vertigo [20]. In rare cases, isolated vestibular vertigo may be caused by acute cerebrovascular accident [21, 22]. This is how occlusion of the distal branch of the anterior inferior cerebellar artery manifests itself, causing ischemia of the cerebellar patch, occlusion of the median cerebellar branch of the posterior inferior cerebellar artery (when vestibular vertigo occurs without other manifestations of Wallenberg-Zakharchenko syndrome), occlusion of the labyrinthine artery. The artery of the labyrinth supplies blood not only to the peripheral vestibular apparatus, but also to the cochlea, and since the latter is less sensitive to ischemia, there may be no hearing impairment when the artery is occluded.
More than 70% of elderly patients have vertebrobasilar insufficiency [4]. More than half of all ischemic strokes in elderly patients are, to one degree or another, associated with damage to extracerebral arteries, primarily of atherosclerotic origin. In 50% of patients over 60 years of age, atherosclerosis is combined with arterial hypertension [10]. The atherosclerotic process causes changes in cerebral circulation, leading to stenosis and occlusion of the main arteries of the head, deterioration of the possibility of collateral redistribution of blood, an increase in cerebral peripheral vascular resistance, a decrease in cerebral perfusion, oxygen and energy starvation of brain tissue, contributing to the development of discirculatory disorders [4]. Changes in the vascular wall occur with an increase in its permeability, periventricular edema, secondary compression of venules, and a slowdown in venous outflow [2, 5]. A common cause of dizziness in hypertension is increased intracranial pressure: up to 60% of patients with intracranial hypertension suffer from dizziness in combination with hearing loss. Central dizziness often occurs with blood diseases (anemia, thrombocytopenia, thrombophilia, polycythemia). Polycythemia deserves special attention because the arteries of the inner ear are small in diameter. Their blood circulation depends not only on systemic hemodynamics, but also on the rheological properties of the blood. Polycythemia causes severe circulatory disorders, especially in small arteries, and dizziness can also be a leading syndrome [18].
With migraine, dizziness also often occurs in the structure of vascular paroxysms. Each paroxysm, especially a prolonged one, can worsen blood circulation in the ear area [23]. Degenerative diseases of the spine can also lead to dizziness [24]. Osteophytes formed during osteochondrosis and spondylosis deformans in the area of uncovertebral joints have the greatest compressive effect on the vertebral artery. They cause dynamic irritation of its sympathetic plexus only during certain positions or movements in the cervical spine. In addition to mechanical compression, vascular spasm may occur as a result of irritation of the periarterial nerve plexus. Displacement and compression of the vertebral arteries can also be observed as a result of subluxation of the articular processes of the vertebrae. The vertebral artery is injured by the apex of the superior articular process of the underlying vertebra due to pathological mobility between the individual segments (two vertebrae connected by a disc) of the cervical spinal column [16, 25]. Compression of the vertebral arteries is also possible by the neck muscles (scalenus, longus colli, inferior oblique capitis) when they contract in certain positions of the head.
Central vertigo is characterized by a less acute onset, dizziness can be systemic and non-systemic in nature, hearing loss (less severe) or tinnitus is often bilateral in nature, nystagmus is bilateral in nature. With central vertigo, occipital headaches appear, radiating to the neck, sometimes to the parietotemporal region and the orbit, instability is observed when walking and standing (static ataxia), less often dynamic ataxia, indicating transient ischemia of the cerebellar structures. Attacks of sudden falling without loss of consciousness (drop attacks) and syncope often develop. Progression of visual and oculomotor disorders is possible: transient diplopia, attacks of “blurred vision”, “spots” and “zigzags” in the visual field, transient hemianopia - all this indicates ischemia of the occipital lobes of the brain. In addition, memory for current events deteriorates; occasionally, attacks of transient global amnesia occur, when the patient’s working memory (memory ability) is impaired for several hours, the patient is confused and disoriented. Often, dizziness of central origin is accompanied by sleep disturbances, increased fatigue, and autonomic disorders (hyperhidrosis, pallor or cyanosis of the skin) [9]. The general practitioner should remember that a patient with systemic dizziness must be referred for consultation to an otoneurologist.
Unsystematic dizziness
Non-systemic dizziness often occurs with arterial hypotension, asthenic conditions, with chronic somatic diseases, with conditions associated with a decrease in blood volume (anemia, acute blood loss, hypoproteinemia and low plasma volume, dehydration) [9, 13]. When blood pressure drops against the background of ongoing cerebrovascular disease, ischemia often develops in the brain stem, which also manifests itself as non-systemic dizziness [21]. Deficiency of adrenergic effects and, consequently, clinical manifestations of orthostatic hypotension are manifested in the picture of Addison's disease, renal amyloidosis, in some cases of the use of pharmacological agents (ganglionic blockers, antihypertensive drugs, dopaminomimetics such as Nakoma, Madopar and some dopamine receptor agonists), with organic pathology of the heart and blood vessels (with aortic stenosis, ventricular arrhythmia, tachycardia, atrial fibrillation) [3].
The appearance of dizziness is possible with bradycardia due to an increase in the vagal reflex. In this case, there is a decrease in heart rate until loss of consciousness in the absence of any heart disease. This is probably due to the fact that stimuli capable of causing such an unusual autonomic response can come from different organs, the afferent innervation of which is vagal, trigeminal, glossopharyngeal or spinal. The prefainting state is characterized by a feeling of lightheadedness and near loss of consciousness, and there is no true sensation of rotation of the patient himself or the world around him [23]. Unsystematic dizziness is manifested by a sudden onset of general weakness, a feeling of lightheadedness, “darkening in the eyes,” ringing in the ears, a premonition of an imminent fall and loss of consciousness (fainting). In the latter case, that is, when dizziness precedes loss of consciousness (fainting), it is called a presyncope [9]. A presyncope does not necessarily lead to fainting (this depends on the speed and extent of the drop in blood pressure). These conditions can often recur, then the main complaint of the patient will be dizziness.
There are vasodepressor (vasovagal); hyperventilation fainting (syncope); syncope associated with carotid sinus hypersensitivity; cough fainting; nocturic, hypoglycemic, orthostatic and other types of fainting. In all these cases, the patient experiences a feeling of lightheadedness, complains of dizziness and a premonition of loss of consciousness [3, 14, 26]. In such cases, fainting must be differentiated from epileptic seizures using electroencephalography.
Differential diagnosis of ICVS with dizziness of other etiologies
Differential diagnosis of ICVS should be carried out taking into account the characteristic features of certain pathological conditions. Psychogenic dizziness is observed as part of anxiety and depressive disorders. This is the most difficult section of neurological diagnostics. The prevalence of psychogenic dizziness reaches 12–15% of cases. The diagnosis is established in the absence of a morphological cause or any focal damage. In addition, dizziness can be a manifestation of somatized depression - neuroses with phobic disorders, vegetative paroxysms, pathological personality changes during hysteria [27]. Physiological dizziness occurs when the vestibular apparatus is overstimulated. It is observed in the case of a sharp change in movement speed (sickness), due to prolonged rotation, when observing moving objects, being in a state of weightlessness, etc.
Sometimes they are perceived and described by patients as conditions resembling dizziness, imbalance and gait disturbances (dysbasia), associated with paretic, atactic, hyperkinetic, akinetic, apractical or postural disorders [9]. The causes of imbalance caused by changes in the efferent part of the motor act include normal pressure hydrocephalus, Parkinson's disease, chronic subdural hematoma, tumors of the frontal lobes, as well as taking a number of medications - anticonvulsants (phenytoin, phenobarbital, carbamazepine), benzodiazepines, neuroleptics (phenothiazines, haloperidol ), lithium preparations. The most pronounced disorders develop with cerebellar disorders, tumors of the cerebellopontine angle, temporal bone and posterior cranial fossa. They are characterized by a feeling of instability, difficulty walking or maintaining a certain posture, and possibly increased discomfort when performing actions that require precise coordination of movements. Characteristically, symptoms worsen in the dark. Systemic dizziness is observed much less frequently with this pathology. In the vast majority of cases, concomitant neurological symptoms are detected.
In acute traumatic brain injury, especially with a fracture of the temporal bone pyramid, dizziness is noted as the leading syndrome. Virtually every concussion has a cervical component due to ballistic changes in the head-to-spine mass ratio [8, 9]. Cervical whiplash often occurs in a car accident when there is sudden hyperextension, then sudden hyperflexion in the cervical spine. Difficulties in diagnosis are due to the fact that symptoms of dizziness do not appear in the acute period, but 1–2 weeks after the injury, and the injury occurs in the absence of visible injuries to the neck. The cause of dizziness is pathological proprioceptive pulsation associated with injury to the soft tissues of the neck and spinal joints [18]. It must be remembered that dizziness can be part of the structure of a convulsive seizure when the epileptogenic focus is localized in the temporal lobe of the brain. Dizziness can occur as the only symptom, which then ends on its own (a discharge that occurs in the form of dizziness), and can also be part of the structure of a partial seizure of secondary origin. The onset of the attack in these cases develops with dizziness followed by the development of tonic-clonic convulsions. In such cases, the patient's examination should include electroencephalography [4].
An attack of Meniere's disease resembles an attack in peripheral cochleovestibular syndrome, but is much shorter in duration, and the course of the disease is recurrent. A sudden unexpected attack of pronounced systemic dizziness appears in combination with nausea and often vomiting, decreased hearing in one ear (or noise in it), spontaneous nystagmus with a short duration (1-3 hours) and complete relief of all symptoms. Characteristically, there are no other neurological symptoms or changes in the blood vessels of the brain (during examination). Dizziness may also accompany multiple sclerosis. The disease is relapsing in nature and is typically characterized by a combination of vestibular and cerebellar disorders with other symptoms of multiple sclerosis. Magnetic resonance imaging of the brain reveals areas of white matter demyelination. For tumors of the cerebellopontine angle (neurinoma of the VIII nerve), an early sign is damage to auditory function (sharp hearing loss, usually in one ear); less commonly, vestibular dysfunction (dizziness is not pronounced), often with damage to other nearby cranial nerves; in the later stages, balance disorders are added. The diagnosis can be confirmed by magnetic resonance imaging.
Additional examination methods
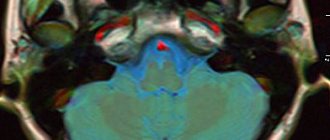
Additional examination methods include the classic and advanced otoneurological method using data from computer electronystagmography, audiometry, auditory evoked potentials, the study of central hemodynamics, determination of hemorheological parameters, ultrasound methods for studying cerebral blood flow (duplex scanning, transcranial Dopplerography), computer and magnetic resonance imaging brain, magnetic resonance angiography and radioisotope angioscintigraphy of the brain. If a spondylogenic effect on the vertebral artery is suspected, radiography or magnetic resonance imaging of the cervical spine is performed.
Choice of ICS therapy
The main principles of ICS therapy are preventing the onset or progression of the pathological process, improving cognitive functions and taking general therapeutic measures [6, 10, 26]. ICVS therapy should be comprehensive and include drugs with multidirectional mechanisms of action. In order to prevent secondary ischemic disorders, it is necessary to prescribe antiplatelet agents (acetylsalicylic acid, ticlopidine, dipyridamole), and in case of increasing symptoms, anticoagulants [24]. Treatment of systemic dizziness is largely determined by its cause; in addition, symptomatic therapy plays an important role [4]. A clear distinction should be made between so-called “emergency” therapy and long-term therapy [12]. Early and long-term use of vestibulolytic drugs is necessary. An example of such drugs is betahistine dihydrochloride, which has an effect on histamine H₁ and H₃ receptors and improves microcirculation in the labyrinth and neurotransmission in the area of the vestibular nuclei of the central nervous system [6]. The use of this drug does not provide a quick clinical effect, but requires compliance with the dosage regimen (daily dose 48 mg) and long-term use (at least 1 month).
“First aid” therapy for ICVS should be carried out with drugs that have vasoactive, neuroprotective and metabolic properties (Vasobral, Cavinton). It is extremely important that this therapy is aimed at correcting local pathophysiological mechanisms - impaired tone of cerebral arteries and veins, metabolic processes in the brain, hemorheology and microcirculation [12]. The clinical effect of these drugs is usually achieved within 10–14 days. The duration of the course of treatment and the choice of drug are determined by the doctor individually. Due to a decrease in the tone of the cerebral veins and disturbances of venous outflow, venotonics are successfully used. Due to the fact that oxidative stress plays a special role in the clinical and morphological picture of ischemia, drugs with neurometabolic effects are used that improve the survival of neurons under conditions of chronic hypoxia (Actovegin).
Actovegin is a deproteinized hemoderivative from the blood of calves, containing low molecular weight peptides and nucleic acid derivatives [28]. It should be noted the activating effect of Actovegin on the energy metabolism of cells of various organs [11, 19, 22]. This is due, first of all, to the ability of the drug to increase the uptake and utilization of glucose and oxygen, leading to an improvement in aerobic energy production in the cell and oxygenation in the microcirculatory system. At the same time, anaerobic energy exchange in the vascular endothelium improves, accompanied by the release of endogenous substances with powerful vasodilating properties - prostacyclin and nitric oxide. As a result, organ perfusion improves and peripheral resistance decreases [18]. Activation of oxygen energy exchange in almost all organs that are in a state of metabolic insufficiency contributes to increased metabolism of high-energy phosphates in the cell, activation of oxidative phosphorylation enzymes and acceleration of the synthesis of carbohydrates and proteins and the breakdown of anaerobic glycolysis products [20]. An increase in oxygen consumption by various tissues under the influence of hemodialysate has been demonstrated in in vitro experiments, in animal models and in humans [5, 8, 9, 12, 14, 16, 22, 25]. Studies on healthy volunteers have shown that under conditions of hypoxia, the drug not only increases oxygen consumption, but also promotes its accumulation, that is, the maximum effect of the drug is manifested precisely in conditions of oxygen deficiency.
Actovegin has an insulin-like effect, which increases the effectiveness of its use in patients with ICVS due to diabetes mellitus. It stimulates the transport of glucose into the cell without affecting insulin receptors [19]. It is assumed that Actovegin takes part in the final stage of activation of glucose carriers present in the membrane [20]. In terms of activity in relation to intracellular glucose transport, the drug is only two times inferior to insulin. In addition, Actovegin stimulates (up to 5 times) lipid biosynthesis. This effect is also insulin-independent and is not affected by insulin antibodies. The drug has a pronounced inhibitory effect on the lipolytic effect caused by stimulation of the adrenergic system. Actovegin has a positive effect on impaired cerebral metabolism during ischemia, providing noticeable changes in the accumulation of glucose, adenosine triphosphate and lactate under the influence of the main substrates of the drug [17]. In addition to cases of general cerebral ischemia, hemodialysate has been successfully used to improve the energy status of cells in lesions of the hippocampus.
Actovegin has both a central effect, stimulating cerebral metabolic processes, and a fairly pronounced effect in peripheral arterial disorders. This mechanism ensures stabilization of the functional metabolism of tissues under conditions of temporarily induced stress and hypoxia during peripheral ICVS [8]. Actovegin is most effective when used in high doses – from 800 mg to 4 g [15, 22]. In patients with ICVS, the drug is prescribed in doses of 800–1200 mg/day intravenously for 10 days, followed by switching to oral administration at 200 mg 3 times/day for 1–3 months. The advantages of Actovegin include its low toxicity and good tolerability. The only contraindication to the use of the drug is hypersensitivity. In most studies, drug tolerability was assessed as “very good” and “good” [17, 20, 22]. In rare cases, hypersensitivity reactions have developed. Discontinuation of the drug due to poor tolerability was extremely rare in clinical studies.
Understanding the mechanism of action of drugs expands the range of possibilities for drug therapy for ischemic cochleovestibular syndromes [26]. The final conclusion about the effectiveness of the chosen treatment and the need for its correction can be made in the absence of a therapeutic effect after 2-3 courses lasting at least 3 months. You should not refuse the chosen drug unless its dose has been increased to an individual maximum and well tolerated. In case of insufficient effectiveness, but good tolerability of the drug substance, another drug from a different class can be added to the selected drug. However, despite the fact that new opportunities have appeared in the arsenal of doctors, many unresolved questions remain. Apparently, it is necessary to radically reconsider approaches to the study of this topic, to define strict criteria for the prescription, combination and dosage of drugs.
Conclusion
Thus, the prevalence of dizziness in patients with cerebral ischemia and the complexity of drug correction of its negative consequences is one of the most complex and pressing problems of modern medicine. Research in this area is of great importance for clinical practice. The use of the proposed algorithm will allow us to systematize knowledge about the causes, types and possibilities of drug correction of ICVS.
Muscle tone disorders
Movement disorder syndrome - a pathology of motor activity - is diagnosed in almost all children with intrauterine abnormalities in the development of the central nervous system. Only the severity and level of damage varies.
When making a diagnosis, the pediatrician must understand what the zone and location of the lesion is, whether there is a problem in the functioning of the brain or spinal cord. This is a fundamentally important question, since treatment methods differ radically depending on the identified pathology. Also of great importance for making a diagnosis is a correct assessment of the tone of various muscle groups.
Impaired tone in various muscle groups leads to a delay in the appearance of motor skills in the baby: for example, the child later begins to grasp objects with the whole hand, finger movements are formed slowly and require additional training, the child gets up on his feet later, and the cross of the lower extremities prevents the formation of correct walking.
Fortunately, this syndrome is treatable - in most children, thanks to proper treatment, there is a decrease in muscle tone in the legs, and the child begins to walk well. Only a high arch of the foot may remain as a memory of the disease. This does not interfere with normal life, and the only difficulty remains choosing comfortable and well-fitting shoes.
Diagnostics
Perinatal ischemia syndrome due to cerebral hypoxia begins to be diagnosed by performing a visual examination of the child. It's the same with adults. Despite all the advances in medicine, a unique test that can accurately identify DIE has not yet been invented. All laboratory techniques are aimed at identifying how badly the brain is damaged and the current state of the whole organism.
What kind of research will be done depends on the symptoms and how they developed. To decipher the tests, there are special biomarkers that give a complete picture of the degree of HIE. The patient's blood is needed for the study.
Neuroimaging is carried out using:
- neurosonography and/or MRI, a tomograph showing internal brain damage and changes in it;
- Doppler ultrasound, recording the functioning of cerebral blood flow;
- electroneuromyograph to determine the sensitivity of fibers of the periphery of the nervous system.
Additional can be used:
- electroencephalograph to detect developmental delay at an early stage and whether there is epilepsy;
- video monitoring to study the motor activity of children.
If necessary, the victim is examined by an ophthalmologist to determine the condition of the optic nerves and fundus of the eye, as well as the presence of genetic diseases in this area.
Where does regurgitation and tendency to constipation come from?
Autonomic-visceral dysfunction syndrome is characterized by impaired thermoregulation in a child (body temperature rises or falls for no apparent reason), exceptional whiteness of the skin associated with vascular dysfunction, and gastrointestinal disorders (regurgitation, vomiting, a tendency to constipation, insufficient weight gain compared with indicators accepted as the norm).
All these symptoms are most often combined with hypertensive-hydrocephalic syndrome and are directly related to disturbances in the blood supply to the posterior parts of the brain, where all the main centers of the autonomic nervous system are located, which controls the life-supporting systems of the body - digestive, thermoregulatory and cardiovascular.
Advertising
Convulsive syndrome
The tendency to have seizures in the first months of a child’s life is due to immaturity of the brain. Convulsions occur only in cases where the spread or development of a disease process in the cerebral cortex occurs, and have many different causes.
In each specific case, the cause of the convulsive syndrome must be identified by a doctor. Effective assessment often requires a number of studies and manipulations: instrumental studies of brain function (EEG), brain circulation (Dopplerography) and anatomical structures (brain ultrasound, computed tomography, NMR, NSG), as well as biochemical blood tests.
From the point of view of localization, cramps are not the same - they can be generalized, that is, covering the entire body, and localized, which are associated with individual muscle groups.
Convulsions are also different in nature: tonic, when the child seems to stretch out and freeze for a short time in a certain fixed position, and clonic, in which twitching of the limbs and sometimes the entire body occurs.
Parents should carefully monitor their child in the first months of life, because... convulsions in children can become the onset of epilepsy if you do not immediately contact a specialist and do not carry out proper treatment. Careful observation and a detailed description of emerging seizures on the part of the parents will greatly facilitate the doctor’s diagnosis and speed up the selection of treatment.
Treatment of a child with central nervous system damage
Accurate diagnosis and timely correct treatment of CNS pathology is extremely important. The child’s body is very susceptible to external influences at the initial stage of development, and timely procedures can radically change the future life of the child and his parents, allowing at the earliest stages to get rid of problems with relative ease that can become very significant at a later age.
As a rule, children with early age pathologies are prescribed drug therapy in combination with physical rehabilitation. Therapeutic exercise (physical therapy) is one of the most effective non-drug methods of rehabilitation of children with central nervous system lesions. A properly selected course of exercise therapy helps restore the child’s motor functions, using the adaptive and compensatory capabilities of the child’s body.