What causes intracranial hypertension in children?
In order to understand this issue, let's turn to anatomy. The brain in the skull is located movably. Blood and cerebrospinal fluid are in constant motion, bathing the brain, supplying it with nutrients and oxygen. From the spinal canal, the cerebrospinal fluid enters the ventricles of the brain and then returns through the venous sinuses. The speed of movement of cerebrospinal fluid and blood may vary depending on a person’s physical activity. In this case, there is an increase in intracranial pressure , but this is a variant of the norm, it is physiological. About 85% of the skull is occupied by the brain, 8% by blood, and 7% by cerebrospinal fluid. Standard values of intracranial pressure are achieved by maintaining these proportions. If the volume of the brain increases, cerebrospinal fluid accumulates, which causes impaired blood circulation and increased intracranial pressure. And this is a very serious pathology.
Intracranial hypertension: diagnosis
Types of pathology diagnostics include:
- measuring intracranial pressure by inserting a needle into the fluid cavities of the skull or spinal canal with a pressure gauge attached to it.
- tracking the degree of blood filling and dilation of the veins of the eyeball. If the patient has red eyes, that is, the eye veins are abundantly filled with blood and are clearly visible, we can talk about increased intracranial pressure;
- ultrasound examination of cerebral vessels;
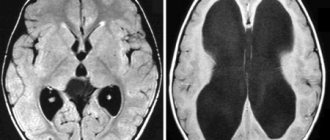
- magnetic resonance and computed tomography: the expansion of the fluid cavities of the brain is examined, as well as the degree of rarefaction of the edges of the ventricle;
- conducting an encephalogram.
Causes of intracranial hypertension in a child
Intracranial pressure also increases in completely healthy children with any physical activity. But this increase is short-term and returns to normal in a calm state. You should be concerned when intracranial pressure is constantly elevated. What are the reasons?
The root cause of intracranial hypertension is a pathological increase in the volume of cerebrospinal fluid, blood or brain tissue, and this occurs due to the following pathologies:
- Hydrocephalus - a violation of the outflow of cerebrospinal fluid and, as a result, its accumulation in the ventricles of the brain, is often a congenital disease.
- Tumors.
- Traumatic brain injury can lead to the formation of a hematoma and cerebral edema, which, in turn, leads to an increase in intracranial pressure due to an increase in brain volume.
- Rapid fusion of the sutures of the skull and fontanel.
- Meningitis and encephalitis due to inflammation of the membranes of the brain lead to its enlargement.
What is the essence of increased intracranial pressure?
The brain is washed externally and internally by cerebrospinal fluid (CSF). It nourishes, washes and protects brain structures from mechanical influences, maintains optimal intracranial pressure, and also regulates metabolic processes between blood and brain.
Liquor constantly circulates in the ventricles of the brain, inside the skull and other spaces of the spinal cord and brain. In certain areas, liquid accumulates, flows out and, having been distributed over other spaces, is absorbed back. There is a certain balance between the absorption and release of cerebrospinal fluid. If more fluid is released than is absorbed or less is absorbed than is released, or there are obstacles to the outflow of cerebrospinal fluid, the fluid begins to accumulate in a certain place, which causes intracranial pressure.
Since the brain is located in a closed cavity of the skull, the accumulated fluid begins to compress the brain, causing an increase in pressure. In this case, the child may experience episodic attacks of headaches.
Intracranial hypertension is not a rare case in infants. The cause of hypertension in a child from birth can be an intrauterine infection or hypoxia, neuroinfection, birth trauma, congenital defects or prematurity. Such children grow up with elevated levels of hypertension from an early age and get used to them, so they do not complain of headaches. The child may experience excessive excitability, lack of concentration and slow formation of certain mental functions (speech, walking, memory, writing, counting, logic, phonemic hearing). Therefore, if any disturbances in the functioning of the nervous system are detected, you should consult a doctor and undergo the necessary examinations.
Prolonged exposure of the brain to cerebrospinal fluid leads to its reduction. At the same time, the number of liquid cavities increases. This condition is called hydrocephalus. It is accompanied by partial replacement of brain matter with cerebrospinal fluid. In severe clinical cases, newborns experience a disruption in the development of nervous system functions and develop cerebral palsy (cerebral palsy). Severe hydrocephalus is treated with a brain shunt. In most cases, using osteopathic techniques, it is possible to get rid of this disease without surgery.
Signs of increased intracranial pressure in older children
In a child of an older age category, arterial hypertension is manifested by the following symptoms:
- Nausea, vomiting. Occurs against the background of irritation of the membranes of the medulla oblongata. The difference between vomiting in hypertension and vomiting in poisoning is that it does not bring relief.
- Pain behind the eyeballs. They are formed due to the effect of cerebrospinal fluid on the orbital area.
- The appearance of ribbons, flashes, double vision. This occurs as a result of irritation of the optic nerves.
- Attacks of headaches that get worse in the evening and at night.
- Restless sleep, irritability, tearfulness.
Why is unstable intracranial pressure dangerous?
The lack of appropriate treatment for hypertension can provoke the appearance of epileptic seizures and the death of certain parts of the brain due to oxygen deficiency. Chronic increased intracranial pressure, even with minor fluctuations from the norm, negatively affects the activity of the central nervous system. At the same time, signs of nervous exhaustion develop quite quickly, such as sleep disturbance, irritability, fatigue, as well as a decrease in intellectual and physical activity.
The greatest danger with unstable pressure is congestion in the optic discs, which can cause atrophy of nerve tissue, a sharp drop in vision and even complete uncorrectable blindness.
High blood pressure in young children: symptoms of the disease
Increased intracranial pressure can be manifested by the following pathological disorders and symptoms:
- Severe crying, restlessness. A distinctive feature of unstable intracranial pressure is that throughout the day the child may feel well and be relatively calm. In the evening and at night the baby begins to cry and becomes restless. This is due to the anatomy of the cerebrospinal fluid and venous systems. The baby lies down more at night and in the evening. As a result, venous outflow slows down, and the veins of the skull and brain become congested. As a result, the volume of cerebrospinal fluid increases, which provokes the development of arterial hypertension.
- Difficulty falling asleep, frequent waking up, sleep disturbance. The listed symptoms are also due to the structure of the venous and cerebrospinal fluid systems.
- Nausea, attacks of vomiting, profuse, frequent regurgitation. These clinical manifestations are reflex. High intracranial exposure provokes irritation of the membranes of the medulla oblongata, which is responsible for nausea and vomiting. It should be borne in mind that frequent regurgitation in a child can be caused by swallowing air during feeding and overfeeding. Therefore, it is not recommended to draw conclusions about intracranial hypertension based on symptoms alone. However, this pathology cannot be excluded either.
- Increase in head volume. The accumulation of cerebrospinal fluid in the cerebrospinal spaces can lead to divergence of the sutures of the cranial bones, enlargement of the frontal part of the skull, enlargement of the fontanelles and disproportionate size of the head.
- The appearance of a venous network under the scalp. With hypertension, excessive filling and stagnation of blood occurs in the venous network. This provokes expansion of the saphenous veins, which makes them visually noticeable.
- Graefe's symptom. It manifests itself as a dysfunction of the oculomotor nerves, which occurs against the background of birth trauma or high blood pressure. The eyeballs periodically begin to deviate downward, and the sclera becomes visible between the upper eyelid and the edge of the iris.
- Refusal to feed. In infants, intracranial pressure physiologically increases, which leads to increased pain. The result of refusal to feed a child is a lack of weight gain.
Disturbances in psycho-emotional and physical development. This can be caused by insufficient feeding and the presence of damaging factors on the brain.
Treatment of increased intracranial pressure with osteopathy
Living with hypertension for a child is unpleasant and harmful to health.
Under the influence of increased compression, brain structures cannot function normally. This causes atrophy of the white brain fluid, followed by a decrease in intellectual abilities and dysregulation of internal organs. To avoid the above complications, treatment of hypertension should begin as early as possible. To alleviate the child’s condition and normalize intracranial pressure, it is important to restore the balance between the absorption and production of cerebrospinal fluid. Traditional medicine uses diuretics for this. Osteopathy treats arterial hypertension in children using safe manual techniques that normalize the level of cerebrospinal fluid without surgery or drug therapy. Osteopathic techniques are aimed at unloading the venous bed of the head and eliminating pinching of blood vessels by the vertebrae.
Symptoms
The development of this pathology can be suspected even in the prenatal period if there are severe infections in the mother, fetal hypoxia, birth asphyxia, prematurity, or birth injuries.
The main signs of intracranial hypertension in newborns and infants include:
- bulging and pulsation of the fontanel;
- excessive growth of the head with disproportionate size;
- divergence of the sutures of the skull;
- convulsions;
- well-defined venous pattern on the skin – “marbling”;
- chin tremor;
- copious and frequent regurgitation, vomiting, resulting in poor weight gain;
- restlessness, crying, sleep disturbance;
- delay in psychomotor development.
Symptoms
In young children, intracranial hypertension can remain compensated for quite a long time due to the softness of the bones and the presence of elastic sutures between them, this explains the long-term subclinical course of the disease. Signs of pathology in infants may include restless behavior, screaming, refusal to eat, vomiting, bulging fontanel and suture dehiscence. With chronic hypertension, children lag behind in neuropsychic development.
In older patients, the clinical picture is typical; its severity depends on the form of the disease. In the acute course of intracranial hypertension, the symptoms in adults will be striking:
- severe headache of a bursting nature throughout the skull, especially in the symmetrical frontal and parietal areas, most often disturbing in the morning after getting out of bed, increasing when bending the head and coughing;
- feeling of pressure on the eyes;
- nausea, sometimes sudden vomiting without preliminary nausea, especially in the morning;
- transient visual disturbances in the form of fog or “floaters” before the eyes, double vision, loss of visual fields;
- noises in the head, dizziness;
- neurological picture - the appearance of focal symptoms from different pairs of cranial nerves.
With a sharp increase in ICP, for example, with acute cranial hypertension, there are often disturbances of consciousness up to and including falling into a coma.
The chronic form of ICH usually proceeds more calmly. The headache can be constant, of moderate intensity with periods of intensification. The deterioration of the patient's general condition occurs gradually: insomnia, irritability, weather sensitivity, chronic fatigue. Sometimes crises may occur with increased blood pressure, headache, vomiting, respiratory distress and short-term impairment of consciousness.
Benign intracranial hypertension in most cases is manifested by transient visual disturbances, which often precede the appearance of headaches of varying intensity; focal symptoms include bilateral damage to the abducens pair of cranial nerves, which innervate the eye muscles and are responsible for turning the eye outward. Mild ICH may not produce pronounced symptoms for a long time, moderate intracranial hypertension manifests itself more strongly when atmospheric pressure decreases, making people especially sensitive to weather conditions. The severe form is life-threatening.
Treatment of intracranial pressure
Treatment requires an integrated approach and depends on the cause that caused it.
- Drug therapy. Treatment is prescribed by a neurologist, using drugs that improve blood supply to the brain and diuretics.
- Surgery is inevitable for hydrocephalus, some traumatic brain injuries, and malignant tumors.
- Physiotherapy and massage.
- Osteopathic techniques. With their help, an osteopathic doctor removes obstacles that cause disturbances in the circulation of cerebrospinal fluid and blood.
It is worth noting that solving this problem requires an integrated approach. If you suspect that a child has increased intracranial pressure, you should contact an experienced neurologist or osteopath as soon as possible. The sooner measures are taken, the greater the likelihood of a positive treatment result.
Indirect signs of increased ICP
In adults and older children, indirect clinical signs of increased intracranial pressure include:
- Headaches of a bursting-pressing nature. They are usually accompanied by a feeling of pressure in the bridge of the nose or from the inside on the eyeballs, often intensifying in the early morning hours when lying down. This is the most common and characteristic sign of increased intracranial pressure. Simple analgesics and NSAIDs are ineffective, and lowering the general (systemic) blood pressure level does not help either.
- Increased meteosensitivity with deterioration of health when atmospheric pressure changes.
- Functional disorders: mood instability with increased irritability, often with a tendency to tearfulness, increased fatigue, not always sufficient concentration, sleep disturbances.
- Autonomic disorders: increased sweating, increased vascular pattern with periodic appearance of skin marbling and acrocyanosis.
- Recurrent nosebleeds, spontaneous and often difficult to stop. Their appearance is associated with the activation of an emergency compensatory mechanism for regulating intracranial and blood pressure. But they are not observed in all cases; people with extensive and closely spaced venous plexuses in the walls of the nasal cavity are predisposed to them.
- Dizziness. It is unstable, non-systemic, and usually disturbs when weather conditions change, neuro-emotional stress, or increased blood pressure.
- Vomiting that does not have a clear connection with food intake and is not explained by any intoxication or pathology of the gastrointestinal tract. Moreover, it is not always accompanied by clearly defined nausea, does not lead to its relief and does not alleviate the condition.
- Double vision, blurred vision. Such disorders are optional and transient; they occur during acute decompensation of intracranial hypertension.
- Epileptiform seizures (convulsive and non-convulsive), and abortive forms are possible. They are uncommon and usually do not progress to status epilepticus.
- Transient mental disorders. They appear only in a small number of people with intracranial hypertension and are usually associated with decompensation of liquor-dynamic disorders. These may be disturbances of perception (from illusory disturbances to true hallucinosis), disturbances of consciousness (confusion, stunnedness), asthenodepressive syndrome, dysphoria.
The presence of intracranial hypertension can be suspected based on the results of some studies. For example, dilated and congested veins in the fundus of the eye testify in favor of this pathology, especially in combination with a picture of papilledema.
And the EEG with increased intracranial pressure often reveals diffuse changes with signs of increased convulsive readiness of the cerebral cortex without specific focal epileptic activity. Moreover, such deviations are possible even in the absence of any history of attacks.
Intracranial hypertension: treatment, drugs
Increased intracranial pressure can lead to a decrease in the patient’s intellectual abilities and disruptions in the normal functioning of internal organs. Therefore, this pathology requires immediate initiation of treatment aimed at reducing intracranial pressure.
Treatment can only be carried out if the causes of the pathology are correctly diagnosed. For example, if intracranial hypertension occurs due to the development of a tumor or hematoma of the brain, then surgical intervention is required. Removal of a hematoma or neoplasm leads to normalization of intracranial pressure.
When increased intracranial pressure is a consequence of inflammatory processes in the body (meningitis, encephalitis, etc.), then the only effective method of treatment is massive antibiotic therapy. In this case, antibacterial drugs can be injected into the subarachnoid space in combination with the extraction of part of the cerebrospinal fluid.
Therapy is aimed at reducing the release of cerebrospinal fluid while simultaneously increasing its absorption. For this purpose, patients are prescribed diuretics.
Quite often, treatment does not require taking any medications. A set of gymnastic exercises is developed for the patient, the implementation of which leads to a decrease in intracranial pressure. Adjustments are also made to the diet and a drinking regime is developed individually. Light manual therapy, acupuncture and physiotherapy have a beneficial effect. The effectiveness of non-drug treatment is observed within the first week from the start of therapy.
In case of postoperative, congenital cerebrospinal fluid block or other severe cases, surgical treatment is indicated. The most common type of surgical intervention is bypass surgery, that is, the insertion of a special tube with one end into the abdominal cavity or heart cavity, and the other into the cerebrospinal fluid space of the brain. Thus, excess cerebrospinal fluid is constantly removed from the skull, leading to a decrease in pressure.
When intracranial pressure increases at a very high rate and the patient’s life is threatened, urgent measures are required to save the patient. In this case, the patient is injected intravenously with a hyperosmolar solution, artificial ventilation is performed, the patient is put into a medically induced coma, and excess cerebrospinal fluid is removed by puncture.
The most aggressive treatment measure, which is resorted to in the most difficult cases, is decompressive craniotomy. At the time of the operation, a skull defect is created on one or both sides so that the brain does not rest against the bones of the skull.
Intracranial hypertension can be completely eliminated if the causes that caused it (tumor, poor blood flow, etc.) are eliminated.