Vegetative-vascular dystonia and osteochondrosis of the cervical spine very often have similar symptoms. Therefore, only a qualified specialist can make a correct diagnosis.
At the Yusupov Hospital, high-level specialists diagnose and treat VSD and cervical osteochondrosis, which is the key to successful rehabilitation.
The relationship between VSD and cervical osteochondrosis
Relationship between VSD and cervical osteochondrosis
Cervical osteochondrosis is destruction of the spinal column in the cervical region and deformation of the intervertebral discs. In the presence of this disease, the vertebral discs are deformed and destroyed. Nerve endings and blood vessels are compressed, causing poor circulation in the brain. As a result, vegetative-vascular dystonia develops.
Physical health gradually deteriorates, headaches, dizziness, surges in blood pressure, increased heart rate, causeless fear and panic attacks appear. There are enough provoking factors causing the appearance of the disorder. However, to treat VSD, you will need to find the underlying cause of the pathology.
Cervical osteochondrosis occurs due to deformation of the vertebral discs. The discs collapse and become mobile. As a result, any movement leads to irritation of nerve endings and blood vessels, which cause pain in the cervical spine. Correctly selected treatment will help prevent the development of intervertebral hernia. Otherwise, the blood supply to the brain will be disrupted, and pain will appear in the thoracic and cervical spine. Discomfort leads to headaches, rapid heartbeat with signs of tachycardia, and dizziness, which are similar to the symptoms of vegetative-vascular dystonia.
Osteochondrosis, VSD. Should you worry so much about symptoms and diagnostic results?
Maxim, St. Petersburg
1353 views
May 14, 2017
Good afternoon. I am 31 years old. Since childhood, I have been periodically (1-3 times a year, usually spring-autumn or winter or after an illness or stress) tormented by the following symptoms: foggy head, fatigue, quiet whistling in the ears, loss of appetite, depressed and very suspicious mood, reluctance something to do, slight dizziness, weakness in the arms and legs, I don’t sleep well. In my head at this moment I only think about illnesses, this only makes it worse and I work myself up to the point of fainting. Thoughts that this is some very serious disease or that doctors are missing something just itch in my head, I start reading a lot about diseases and symptoms and it gets even worse, fear of either dying or becoming a “vegetable” or going crazy. At peak moments, the pressure rises to 140-150 by 90-100, throws you into a fever and then into a cold sweat, and after 5 minutes everything rolls back and only the above symptoms remain. This condition can last from several days to several weeks. Sometimes the temperature reaches 37.3 during the day, in the morning and evening it is about 36.8-36.9. And indigestion, the stool becomes soft as if underdigested. Among chronic diseases - Gilbert's syndrome and VSD was diagnosed in childhood. Did various blood and urine tests. Clinical analysis is normal. Sugar and cholesterol are normal. Thyroid hormones and ultrasound are normal. Urine is normal. Now I have this condition again - it started 1.5 weeks ago with a sore throat (I have chronic tonsillitis), then I became hypothermic for several hours in the cold and wind, the sore throat quickly went away, but then everything that I described above began, plus the pressure was 120 /60-65 happens (is it worth panicking because of such a big difference?), measured in a lying position. And the temperature rises to 37.3 again. As a child, it seemed to me that it was somehow easier to bear, maybe I just had a simpler attitude towards it. Now I have done an X-ray of the cervical region, an EEG, and duplex scanning of blood vessels. X-ray shows initial signs of osteochondrosis c4-c6 and spondyloarthrosis c4-c7. EEG is a picture of mild changes in BEA of a combined nature, indirect signs of dyscirculatory disorders. The functional state of the regulatory structures of the trunk is unstable. Duplex scanning revealed no stenosis, pathological tortuosity, or atherosclerotic changes in the carotid arteries. In the subclavian - the main blood flow. PA without significant asymmetry in diameter and blood flow. The tortuous course of the VA in the bone canal. During rotation tests, the decrease in BFV in the right and left VA was more than 30%. Signs of distinct extravasal (vertebrogenic) influences on the blood flow of the left and more of the right VA. VBB blood flow in the subcompensation stage. Venous congestion of the 1st degree in the suboccipital venous plexus. A clinical blood test showed only: segmented - 45% when the norm is 47-72%. And LYMPH (lymphocytes) - 46% when the norm is 19-37%, is this for a sore throat and hypothermia? Is all this wealth related to osteochondrosis? And how will all this affect your future life? I would like to minimize these attacks or have less severe symptoms. Is it really possible to cope with this? Should I worry that much about this? It makes it very difficult to work, intellectual work, at the computer. In the intervals between exacerbations, my mood and other things are in complete order, nothing bothers me, I enjoy life. Thank you. Best regards, Maxim.
The question is closed
VSD
osteochondrosis
Symptoms of VSD in cervical osteochondrosis
Symptoms of VSD in cervical osteochondrosis are characterized by the following features:
- Disturbance in the functioning of the heart and blood vessels (arrhythmia with the manifestation of tachycardia is observed).
- Hot flash or chills.
- Coldness in upper and lower extremities.
- Blood pressure surges.
- Paleness of the skin.
- Increased heart rate.
- Headache, dizziness, shortness of breath, difficulty breathing.
- Heaviness in the chest.
- Gastrointestinal disorders (attacks of nausea, heartburn, increased gas formation or diarrhea).
Increased sweating, panic attacks, fear, anxiety, irritability, and insomnia are observed. Regular fatigue, pain in the neck, and tinnitus appear.
Treatment and prevention of symptoms of cervical osteochondrosis
Treatment of symptoms of cervical osteochondrosis of the spine should be carried out comprehensively. In each case it is necessary to find an individual approach. Medicines, physical therapy, massages and some folk remedies can help cope with the disease.
If osteochondrosis is in an acute stage, then its treatment will be aimed at improving blood circulation and eliminating spasms and pinching. The doctor can prescribe medications to the patient that will improve blood flow, as well as relieve inflammation and reduce pain.
Medicines for the treatment of cervical osteochondrosis
Clinical studies have shown that during exacerbation of cervical osteochondrosis, analgesics and non-steroidal anti-inflammatory drugs work well. In addition to them, the doctor prescribes chondroprotectors, antispasmodics and drugs that stimulate blood circulation in the tissues.
For complex therapy in the treatment of cervical osteochondrosis, the following are used:
- Analgesics. Eliminate pain. Some of them can have an anti-inflammatory effect. Most often, analgesics are prescribed for lumbar osteochondrosis, which has a wide localization of pain;
- Antispasmodics. They have an analgesic and antispasmodic effect. Eliminate muscle spasms, block the sensitivity of nerve endings;
- Anti-inflammatory drugs. Relieve pain, reduce inflammation;
- Vasodilators. Necessary for improving blood circulation. Reduces the recovery time of the body after osteochondrosis;
- Chondroprotectors. Necessary for tissue restoration in damaged cartilage. One of the most effective drugs today is Artadol. It contains chondroitin sulfate, which actively fights the degradation of articular cartilage. The drug stimulates the production of proteoglycans. Improves metabolic processes in cartilage and bone tissue.
Regardless of the stage of the disease and the degree of pain, doctors strongly recommend refraining from self-medication. Only after examination by a specialist, analyzes and tests can the doctor prescribe adequate and effective treatment for cervical osteochondrosis.
Massage for cervical osteochondrosis
Massage is necessary to relieve pain and improve muscle tone. Different techniques are used, which depend on the stage of the disease. In the treatment of cervical osteochondrosis, the following are effective:
- stroking;
- squeezing;
- rubbing;
- kneading.
If pain is observed only on one side of the neck, then the massage begins with a healthy part of the body, gradually moving to the sick one. It can be performed at home or in a specialized institution. But you should be extremely careful, since incorrect movements and influences can only aggravate the situation.
Therapeutic exercises for symptoms of cervical osteochondrosis
Therapeutic gymnastics is used in complex therapy in the treatment of cervical osteochondrosis and gives excellent results. Unlike medications, it has no contraindications or side effects. Exercise therapy aims to improve blood flow to damaged parts of the body. It is important that the patient does not feel pain when performing certain exercises.
Therapeutic gymnastics is designed to strengthen the muscles in the neck area, and also serves as an excellent prevention of osteochondrosis.
Causes of pathology
A malfunction of the nervous system provokes the development of vegetative-vascular dystonia. Diagnosis of VSD is carried out in conjunction with an examination of the cervical spine. Different pathologies have similar signs and symptoms. To make a correct diagnosis, you will need to undergo a comprehensive examination. The main causes of cervical osteochondrosis that provoke the appearance of VSD include:
- Poor posture and curvature of the spine (scoliosis).
- Heredity.
- Serious injuries to the musculoskeletal system that caused circulatory problems.
- Stable physical activity associated with lifting heavy objects.
- Sedentary lifestyle.
As a result, muscle tissue becomes weak and intervertebral discs become mobile. This condition disrupts the functioning of the nervous system and causes the development of VSD.
Clinical picture
Vegetative-vascular dystonia is characterized by a variety of clinical manifestations. Their large number is due to the disorder of all basic vegetative functions - breathing, blood supply, sweating, urination, digestion, peristalsis. In most cases, symptoms of VSD occur with cervical osteochondrosis of grade 2, 3, when changes in the vertebrae and discs have become irreversible. Often, complications of the disease—protrusions, hernial protrusions, discogenic myelopathy—lead to functional disorders.
Cardiac symptoms
Most often, VSD is clinically manifested by tachycardia - an arrhythmia characterized by a heart rate of more than 90 beats per minute. There are sensations of interruptions in the functioning of the heart, its freezing, vascular pulsation not only in the back of the neck, but also in the legs and arms.
One of the leading symptoms of VSD is pain in the cardiac region. It can be acute, but more often it is dull, aching, pressing. Diadynamic functional disorders are also noted. Blood pressure increases or decreases, blood and lymph circulation is disrupted.
Pain in the heart area.
Respiratory system
Vegetative-vascular dystonia is characterized by respiratory symptoms that occur against the background of dysregulation of the respiratory system. Tachypnea (rapid breathing), sensations of lack of air, heaviness, congestion in the chest, and severe shortness of breath, which resembles an attack of bronchial asthma, are observed. A patient with cervical osteochondrosis has difficulty in fully inhaling and exhaling.
Nervous system
The psychoneurological symptoms of VSD are so pronounced that they often lead to panic attacks - sudden attacks of unmotivated fear, increased anxiety, and restlessness. In severe cases, patients are diagnosed with depression. Vegetative-vascular dystonia is manifested by lethargy, weakness, and rapid fatigue with minor exertion.
Patients become irritable, tearful, and mental and physical performance decreases against the background of psycho-emotional instability. Gradually, they develop weather dependence, often experience headaches, and experience a disorder in the change of phases of sleep - it becomes superficial and restless.
Panic attacks, irritability, tearfulness are symptoms of pathology.
Other symptoms
A disorder of the autonomic system makes undesirable adjustments to the functioning of almost all human life systems. Symptoms of VSD rarely appear in isolation. More often they are combined with each other, which significantly worsens the patient’s well-being and complicates diagnosis.
| Autonomic disorders | Characteristic signs |
| Thermoregulation disorders | Body temperature is labile - it rises during the day to 38 °C, and then decreases to 35 °C. The patient feels chilly, and then suffers from fever and excessive sweating. Thermoregulatory disturbances may occur from time to time or become permanent |
| Digestive and peristaltic disorders | They manifest themselves as dyspeptic, dyspeptic disorders - attacks of nausea and vomiting, belching, pain in the epigastric region, increased gas formation. Constipation or diarrhea is common |
| Genitourinary disorders | Sexual desire persists against the background of anorgasmia. In the absence of any pathologies of the urinary tract, the urge to empty the bladder becomes more frequent and urination becomes painful |
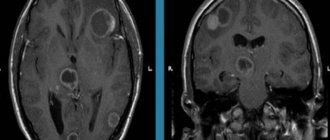
Diagnosis of VSD in cervical osteochondrosis
Signs of VSD and cervical osteochondrosis have similar symptoms to diseases of the brain and internal organs. In the absence of a complete diagnosis, self-medication is prohibited. To establish an accurate diagnosis, you will need to undergo a special examination of the body:
- ECG (electrocardiography)
- Ultrasound.
- Fluorography.
- X-ray.
- MRI of the cervical spine and brain.
- Ultrasound of blood vessels in the cervical spine.
- CT scan.
A comprehensive examination will help confirm or refute the presence of cervical osteochondrosis of the spine. In the absence of serious disorders with the manifestation of symptomatic disorders, vegetative-vascular dystonia is diagnosed.
The diagnosis of cervical osteochondrosis is a myth.
Competent doctors know that the diagnosis of cervical osteochondrosis is one of the most persistent myths in medicine. And those who are less knowledgeable blame a great many problems on osteochondrosis, including panic attacks and symptoms of VSD.
Scientists have long discovered that osteochondrosis is a natural process of aging of the body. Even teenagers have signs of osteochondrosis on x-rays!
We inherited osteochondrosis from our ancient ancestors homo erectus (homo erectus), this is a natural consequence of the evolution of our species and the acquired ability to walk upright.
In fact, osteochondrosis itself does not contribute to the development of VSD and panic attacks and does not give rise to any pronounced clinical complaints. Even neck pain is not a sign of osteochondrosis! Not to mention other symptoms that are attributed to the diagnosis of cervical chondrosis.
What causes panic attacks, neck pain, and other symptoms that are so often attributed to cervical osteochondrosis?
Causes of osteochondrosis
The causes of osteochondrosis are quite varied.
Firstly, with age, the elasticity of the intervertebral discs is gradually lost.
This means that our back requires special attention. Prolonged stay in a position that causes spinal misalignment can cause irreversible changes. You should avoid sitting in an asymmetrical position, fight the habit of lying on only one side, and carrying a load (for example, a bag) in only one hand.
A sedentary lifestyle has a detrimental effect on the health of the spine. It is necessary to move, but physical activity should be moderate. The spine should be given the opportunity to recover after stress, and it is also advisable to avoid injuries that also lead to the development of spinal pathologies.
The second group of reasons is associated with metabolic disorders
and
poor nutrition
. Food rich in carbohydrates and fats saturates the body with calories, which we, in our sedentary city life, often simply have nowhere to spend; As a result, energy is stored as fat tissue, creating excess weight. Obesity is an increased load on the spine, which leads to the development of osteochondrosis. In addition, such a diet usually contains insufficient amounts of microelements (calcium, potassium, phosphorus, magnesium, manganese and others), which are so necessary to strengthen bone tissue. Endocrine diseases are often the cause of excess weight. At the same time, a violation of energy, water or mineral metabolism can also negatively affect the tissues involved in the structure of the spine.
Factors contributing to the development of osteochondrosis may be:
- flat feet;
- hormonal changes;
- infectious diseases;
- local circulation disorders,
as well as some other factors.
What is osteochondrosis?
Osteochondrosis: parts of the spine
Osteochondrosis affects various parts of the spine. Depending on which department suffered the most, there are:
- lumbar osteochondrosis – most common;
- cervical – ranks second in “popularity”;
- sacral;
- chest;
- widespread osteochondrosis, which affects several parts of the spine at once;
- cross pathologies (lumbosacral or cervicothoracic).