The spread of vascular diseases of the brain in recent years has, unfortunately, an increasing trend.
Among them is the most dangerous manifestation of cerebral vascular insufficiency - cerebral stroke (Latin “insultus” - “attack”).
Stroke is the disease of the century. The frequency of its primary cases during the year ranges in economically developed countries from 1.27 to 7.4 per 1000 population. There is also some rejuvenation of the patient population. In Russia, ischemic stroke ranks second in the structure of overall mortality after coronary heart disease. Mortality rates for men and women are 184.6 and 137.3 per 100,000 population, respectively. Only 13% of patients who have suffered an ischemic stroke return to their previous work activity.
Risk factors for ischemic stroke
Stroke in an elderly person is characterized by a severe course, which entails various disorders of neurological and cognitive functions. The main cause of stroke is blockage of blood vessels in the brain by a blood clot. In medicine, there are several types of stroke:
- lacunar;
- atherothromboembolic;
- cardioembolic.
In addition, there are strokes caused by such reasons as a migraine attack, dissection of the arterial wall, and hereditary vascular diseases.
Risk factors contributing to the occurrence of pathology:
- arterial hypertension;
- diabetes;
- excess body weight (obesity);
- diseases of the cardiovascular system, accompanied by arrhythmias of various etiologies;
- age over 55 years;
- bad habits (alcohol abuse, smoking).
In most cases, stroke in older people begins suddenly. According to statistics, the peak of hypertensive crises and strokes occurs at night or early in the morning.
What is a stroke and how does it develop?
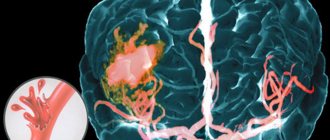
Acute cerebrovascular accident (ACVA, stroke, apoplexy) is an acute disease of the brain caused by blockage (ischemia) or rupture (bleeding - hemorrhage) of a vessel supplying part of the brain, or bleeding into the membranes of the brain.
If you tightly tighten the thigh with a tourniquet (as is sometimes necessary to do when a large vessel is injured in order to stop bleeding), necrosis of the muscles of the lower limb begins in about an hour. The brain is much more sensitive to interruptions in blood flow. Those parts of it that are suddenly deprived of the flow of oxygen and nutrients, and this is the essence of a stroke, can die within a few minutes.
There are two types of strokes: hemorrhagic type (vessel rupture and hemorrhage) and ischemic type (vessel blockage). Most often, stroke, both hemorrhagic and ischemic, develops against the background of hypertension, heart disease (atrial fibrillation, defects, paroxysmal tachycardia), heart failure, and cerebral atherosclerosis. Ischemic brain lesions predominate; the ratio of ischemic and hemorrhagic strokes is on average 5:1.
In
ischemic stroke, the cause of blockage is most often pieces that break off from atherosclerotic plaques in large vessels of the neck or thrombotic deposits on the heart valves;
blood clots that form on large plaques in areas of vasoconstriction, vascular spasms for a long time. In a hemorrhagic stroke, a vessel ruptures when there is high blood pressure, since the artery wall is unevenly thinned due to atherosclerosis. High-pressure blood pushes brain tissue apart and fills the resulting cavity, causing a blood tumor or intracerebral hematoma . Or hemorrhage occurs when a saccular formation on the wall of a vessel ruptures, which is called an aneurysm; such hemorrhage most often occurs in the lining of the brain and is called subarachnoid . Subarachnoid hemorrhage most often occurs before the age of 40 years. A disaster most often occurs after physical exertion (lifting weights, trying to break a stick over the knee), nervous stress, accompanied by a short-term rise in blood pressure.
Symptoms
Stroke in older women and men is manifested by the following symptoms:
- loss of visual fields;
- high blood pressure, dizziness;
- paresis of a limb or half of the body;
- dysarthria (unintelligible and incoherent speech);
- distorted face;
- confusion;
- loss of coordination of movements (partial, complete).
As a rule, when a stroke occurs, a combination of these symptoms occurs, and to make sure that a person is developing this particular disease, you need to do a simple test before doctors arrive:
- ask to repeat any phrase. If speech is unintelligible, it is a stroke;
- ask to smile. If the patient has a stroke, the smile will be asymmetrical;
- ask to raise your arms, bending them at an angle of 45 degrees, and hold in this position for several seconds. If one arm does not lower, then it is a stroke.
Important! If even one of these signs appears, you should immediately call an ambulance. It is strictly forbidden to give a person any medications, as this can only worsen the situation!
Before the ambulance arrives, you need to lay the patient down, raising his head slightly. Provide him with a flow of air: open the window, unfasten his collar, free him from his belt and tie. If vomiting begins or the victim loses consciousness, carefully turn his head to the side and remove his tongue from the mouth so that it does not fall back.
Causes
If the focus of impaired blood circulation is located in the hypothalamus and/or brain stem, then hyperthermia will be a mandatory symptom of a stroke.
The hypothalamus is responsible for thermoregulation of the body; damage to this part of the brain leads to pathological changes in heat exchange rates.
There is another reason for high temperature during a stroke. Sometimes a brain stroke occurs against the background of acute inflammatory processes in the body, for example, influenza, pneumonia, etc. Hyperthermia in such cases is caused by the body’s fight against an infectious pathogen.
Consequences of a stroke
The transferred disease has consequences that, depending on the type and course of the pathology, can remain for many years, or may disappear after a certain period of time.
Manifestations of the disease are divided into several groups:
- speech disorders. A stroke affects different parts of the brain, so the patient may experience changes in articulation or speech production;
- motor disorders. An elderly person may have impaired mobility of the limbs or mobility of the face;
- cognitive disorders. They are characterized by absent-minded attention, decreased intelligence, memory loss;
- emotional-volitional disorders. A person with such manifestations after a stroke becomes “tearful”, as a result of which he can plunge into a prolonged depressive state.
These consequences arise only after the end of the acute period of pathology. In the first weeks after a stroke, the patient has symptoms such as speech impairment, frequent headaches, unstable blood pressure, and arrhythmia. In some cases, high body temperature, tremors, and convulsions are noted.
The bleeding is extremely severe. In 50–90% of cases, death is observed.
The severity of symptoms is determined by the formation of secondary brainstem symptoms - swelling of the brainstem, displacement, herniation.
The spilled blood triggers a whole cascade of biochemical reactions, leading, in the first 2 days, to the development of vasogenic cerebral edema (acute period). On the third day, delayed vasospasm develops, which leads to the development of necrotizing angiopathy and calcium cell death.
It is possible for hemorrhage to develop through diapedetic bleeding - due to prolonged spasm of the vessel, slowing down the blood flow in it, and its subsequent persistent expansion. In this case, disruption of the functioning of the endothelium occurs, the permeability of the vessel wall increases, and plasma and blood elements leak out of it into the surrounding tissues. Small hemorrhages merge to form hemorrhagic foci of various sizes.
You should be especially careful about headaches. It may be a harbinger of a brain catastrophe.
The development of stroke is acute (apoplexy), sudden with a rapid increase in neurological symptoms.
Rapidly growing headache - especially severe, with nausea and vomiting, “hot flashes and pulsations” in the head, pain in the eyes when looking at bright light and when rotating the eyes to the sides, red circles before the eyes, breathing problems, palpitations, hemiplegia or hemiparesis ( paralysis of the limbs of the same name - right-sided or left-sided), impaired consciousness of varying degrees of severity - stunning, stupor or coma. Here is a scenario for the development of a hemorrhagic stroke.
A sudden onset of the disease with the development of an epileptic attack is possible. Against the background of complete health on the beach, during strong emotions at work, during an injury, a person falls with a cry, throws back his head, convulses, breathes hoarsely, foam comes out of the mouth (possibly with blood due to biting the tongue).
The gaze is turned towards the hemorrhage, the patient seems to be looking at the affected side of the brain, on the side of the hemorrhage there is a wide pupil (mydriasis), possibly divergent strabismus, the eyeballs make “floating” movements, the gaze is not fixed; on the side opposite to the hemorrhage, atony (drooping) of the upper eyelid develops, the corner of the mouth droops, and the cheek does not hold air when breathing (the “sail” symptom).
Meningeal symptoms appear - it is impossible to tilt your head forward and touch your chin to the chest, it is impossible to lie on your back and bend your leg at the hip joint to straighten it at the knee.
The course of extensive hemorrhages in the cerebral hemisphere can be complicated by secondary stem syndrome. Disturbances in breathing, cardiac activity, and consciousness increase, muscle tone changes in the form of periodic tonic spasms with a sharp increase in tone in the extremities (hormetonia) and increased tone of the extensor (extensor) muscles and relative relaxation of the flexor muscles (decerebrate rigidity), the development of alternating syndromes is possible ( syndromes that combine damage to the cranial nerves on the side of the hemorrhage with disorders of movement and sensitivity on the opposite side).
43-73% of hemorrhages end with a breakthrough of blood into the ventricles of the brain. When blood breaks through into the ventricles, the patient’s condition sharply worsens - a coma develops, bilateral pathological signs, protective reflexes appear, hemiplegia is combined with motor restlessness in non-paralyzed limbs (violent movements seem conscious (patients pull the blanket over themselves, as if they want to cover themselves with a blanket), hormetonia, symptoms of damage to the autonomic nervous system deepen (chills, cold sweats, a significant increase in temperature) The appearance of these symptoms is prognostically unfavorable.
At the first symptoms of a stroke, immediate help is required - you need to call an ambulance and hospitalize the patient.
Treatment
The main goal of emergency physicians is to stabilize the victim’s condition and support the functioning of brain cells before hospitalization. For this purpose, basic therapy is carried out, which includes activities such as:
- control and/or correction of blood pressure;
- temperature control;
- relief of seizures;
- control of heart rate and glucose levels;
- maintaining water-salt balance.
Specific treatment in a hospital setting includes thrombolytic therapy, antiplatelet agents, mechanical thrombus extraction, and elimination of cerebral edema.
Thrombolytic therapy
Indications for such therapy: age from 18 to 80 years and no more than 4.5 hours from the onset of the stroke. The victim is administered an effective drug - tissue-type plasminogen activator, which dissolves blood clots.
Contraindications:
- Blood pressure is higher than 185/110;
- sensitivity to drugs of this type;
- erosion, gastrointestinal ulcer in the last 6 months;
- various brain pathologies;
- recent brain surgery;
- taking anticoagulants, etc.
Taking into account the extensive list of contraindications, thrombolytic therapy is performed in no more than 10% of patients.
Antiplatelet agents
These drugs are prescribed to patients on the second day after thrombolytic therapy. If it is not carried out, then on the first day. Aspirin is prescribed as a preventive measure against recurrent stroke, and its use significantly reduces mortality.
Mechanical thrombus extraction
This technique is the most effective. As a result of its use, blood supply to the brain is restored in the shortest possible period. The principle of mechanical thrombus extraction is the mechanical removal of blood clots using a special high-precision instrument. A stand is immersed in the artery and advanced to the site of blockage, after which it is removed with a catheter. All manipulations are carried out under radiographic control.
One of the main advantages of mechanical thrombus extraction is the ability to perform it within 6–8 hours after the onset of an ischemic stroke and a small number of contraindications. However, the use of this method is not possible in all clinics. This is due to the need to have in the arsenal of a medical institution the most modern equipment and a staff of vascular surgeons capable of performing this manipulation.
Elimination of cerebral edema
In some cases, stroke patients develop brain swelling. Its elimination is carried out with the help of diuretic drugs. The duration of treatment depends on the severity of the patient's condition.
Why is hyperthermia dangerous?
Hyperthermia during a stroke is a dangerous phenomenon that worsens the course of the disease and reduces the chances of restoring health after a brain stroke.
In the cells of brain tissue during hyperthermia, metabolism and tissue respiration accelerate. These processes require an increased flow of oxygen, but with the disease the opposite phenomenon occurs - oxygen starvation.
Hyperthermia during a stroke leads to faster death of brain cells and significantly increases the focus of ischemic damage.
An increase in temperature contributes to the development of inflammatory processes, necrosis, disorders of cerebral regulation, damage and changes in the brain matter. In severe cases, high fever can be fatal.
Patient care
In most cases, mortality in the first days after the onset of a stroke is caused by impaired blood circulation in the brain. In the subsequent period, patients die from various complications caused by prolonged immobility:
- pneumonia;
- bedsores and/or their infection;
- thromboembolism;
- thrombophlebitis.
That is why patient care must be thorough and regular. It is important to turn the elderly person from one side to the other every 2-3 hours, and also to ensure that the bedding does not bunch up.
Daily care for a person after a stroke includes important elements of rehabilitation, which are recommended to begin immediately after his life is out of danger. Early recovery from this pathology has a beneficial effect on the patient’s condition and contributes to his speedy recovery.
Massage
Passive gymnastics and massage are mandatory activities aimed at preventing the development of bedsores. In addition, these procedures help prevent contracture (limited mobility in the joints) caused by the patient's immobility.
At the initial stage, the patient's muscles are stretched, joints are extended and flexed. Such manipulations should only be carried out by a specially trained person. The time and number of sessions are individual and determined by the attending physician.
Important! The massage must be performed by a specially trained person. The number and time of sessions is determined by the doctor.
If the elderly person is conscious, passive stimulation of the muscle frame and speech gymnastics are prescribed.
The right diet
Caring for an elderly person after an ischemic stroke includes a special diet containing foods rich in potassium. This trace element is found in large quantities in bananas, legumes, fish, seafood, spinach, dried fruits, kefir, and low-fat yogurt. It is recommended to include vegetable salads with vegetable or olive oil and light vegetable soups in the menu.
Coffee, strong tea (all varieties), and alcoholic beverages should be excluded from the diet.
In addition, you should limit your use of:
- red meat dishes (no more than 150 g per day);
- smoked products;
- spicy, salty dishes;
- baking.
Food must be boiled, stewed or baked.
Leisure after a stroke
The patient's time after an ischemic stroke should be devoted to improving mood and returning to an active life.
To improve motor skills and cognitive disorders, it is recommended:
- collect puzzles;
- draw, sew, knit;
- listen to the radio, read books, communicate with people.
Such hobbies promote recovery and significantly increase the chance of returning to a full life.
Doctors are unanimous that a nursing home after a stroke is an excellent opportunity to return to normal life as quickly as possible. The patient is surrounded by care, and qualified staff guarantees proper care, adequate nutrition and round-the-clock supervision.
What are the temperature readings for different types of stroke?
Doctors determine the condition of a person who has a stroke, as well as the degree of damage to brain tissue, based, among other things, on temperature readings.
Hyperthermia is not observed immediately after a stroke occurs. Initially, primary symptoms characteristic of a hemorrhagic or ischemic form of stroke appear, but the temperature may change somewhat later, if by the time the doctor arrives it does not exceed 38 degrees, the patient’s condition is considered normal. Although the best option is a temperature of up to 37.2 0 C.
If, with an ischemic stroke, the thermometer shows 36 0 C, there is hope for a favorable outcome for the patient. This condition is characterized by a decrease in temperature.
Hemorrhagic stroke is always characterized by hyperthermia.
Thermometer readings above 37.5 0 C indicate serious disorders in the patient’s body. The higher the temperature, the more dangerous the situation and the less favorable the forecasts.
A person does not always survive a stroke. It is not at all possible to fully recover after a brain stroke, and at elevated temperatures the area of hemorrhage and hematoma expand, thus putting more pressure on the brain.
The sooner from the onset of the attack the temperature drops to normal readings, the less likely it is to die. Knowing this, doctors, to be on the safe side, inject the patient with medications that lower the temperature, as well as anticoagulants.
First steps in case of attack
If symptoms of a stroke are severe, accompanied by hyperthermia, the patient’s household should call a doctor. Before his arrival, the victim of an ischemic form of pathology can be given Ibuprofen, Paracetamol and Analgin.
When providing primary first aid, it is unacceptable to use strong analgesics, as well as antibacterial and steroid drugs.
In case of hemorrhagic cerebral stroke, the use of any medications before the arrival of an ambulance is prohibited.
Relatives should check the patient for reflexes and consciousness. Upon arrival of the ambulance, the patient is immediately taken to the clinic.
It is difficult to reduce the temperature during a stroke using medications. Hyperthermia is fought with other methods.
- Invasive methods. Intravenous injection of cooled saline solution.
- Catheter monitoring of temperature.
At elevated temperatures, brain cells are not properly oxygenated. This provokes the development of hypoxia, subsequent tissue necrosis and disruptions in cerebral regulation. To avoid such complications, patients have their temperature periodically measured during the first 12 hours after hospitalization.
Drugs for the treatment of post-stroke hyperthermia are prescribed depending on the specific cause that provoked the increase in temperature.
Development and risk groups
The development of a stroke is caused by a sharp increase in blood pressure, physical activity, and emotional stress. In such situations, a vessel ruptures followed by hemorrhage or spasm with ischemia. Predisposing factors are diabetes mellitus, high cholesterol, heart, vascular and blood diseases, and excess weight. In these diseases, blood vessels lose their elasticity and their walls stretch. People who or their close relatives have had a stroke or heart attack should be especially careful.
There are scales that determine the degree of risk of developing a stroke: the Framingham scale for assessing individual risk of developing stroke, the London School of Hygiene questionnaire on cardiovascular diseases by J. Rose.
By undergoing such testing, you can identify the degree of risk, undergo an examination and undergo a course of treatment in a timely manner before your health is affected.
Risk groups are identified:
- by age and gender - the likelihood of a stroke increases after 30 years. Ischemic stroke occurs more often in men aged 50-69 years. The incidence of hemorrhagic stroke up to 60 years of age is the same in men and women, then higher in women;
- in terms of lifestyle - unfavorable factors include inactivity, bad habits, stress, heavy physical labor. These factors worsen health and provoke chronic heart and vascular diseases.
Clinical picture as a whole
In addition to hyperthermia, doctors include general cerebral and focal symptoms in the clinical picture of a stroke.
General cerebral symptoms
Includes the following features:
- dizziness and headache;
- noise in ears;
- urge to vomit;
- disturbances in consciousness - from slight disorientation in space and time to partial or complete loss of consciousness and immersion in a coma;
- convulsions.
Focal signs
Damage to the right hemisphere is accompanied by the following symptoms:
- paresis of the left half of the body;
- speech problems;
- conduct disorder;
- lethargy;
- memory problems.
If there is a violation in the left hemisphere, the following signs are observed:
- paresis of the right half of the body;
- problems with spatial perception;
- hot temper and aggression;
- behavioral disorders.