- Jaw muscle spasm
- Development of the disease
- Symptoms of TMJ problems
- Diagnostics
- Prevention of hypertonicity of the TMJ muscles
- Prevention of hypertonicity of the TMJ muscles
Spasm of the jaw muscles is called trismus, and can be single or multiple.
The jaw muscles are always toned (in background activity, ready for action). Muscle hypertonicity represents increased activity and tension, with decreased ability to stretch. With mild hypertonicity, a person experiences slight discomfort. In the case of moderate or severe hypertonicity, muscle spasm occurs, accompanied by pain. In difficult cases, the jaw cramps so that the person cannot open the jaw. Muscle spasm under the jaw
there is one-sided and two-sided
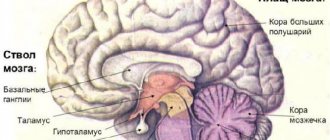
There are several causes of jaw muscle spasm. Common causes may be internal diseases of an infectious or neurological nature:
- Neoplasms in the brain of benign and malignant nature.
- Intracranial hemorrhage.
- Meningitis.
- Diseases of the nervous system (stress, depression).
- Tetanus, rabies.
- Anatomical tissue defects.
Local causes are diseases of the maxillofacial area and injuries:
- Inflammatory process of bone tissue (osteomyelitis).
- Cellulitis and abscess.
- Inflammatory process in the soft tissues around wisdom teeth.
- Inflammation of the periosteum.
- Unsuccessful anesthesia during dental surgery on the lower jaw.
- Dislocation, fracture or crack in the lower jaw.
- Arthrosis or arthritis of the TMJ.
- Inflammatory process in the trigeminal nerve.
- Hypothermia or overload of the lower jaw.
- Periodontitis or pulpitis in an advanced stage.
- Incorrect installation of the bracket system or poor-quality prosthetics.
- Sports injuries (common in boxers who use mouthguards, weightlifters who clench their teeth while lifting weights, scuba divers who use an oxygen tank mouthpiece for long periods of time).
It is important to consult a dentist so that he can diagnose such a multifaceted disease as spasm of the jaw muscles.
The dentist will be able to find out the reasons after examination, history taking, and diagnostics.
Development of the disease
A provoking factor appears that causes a single muscle tension. Constant hypertonicity gradually develops into spasm. Pain weakens the muscle over time as the person tends to use the muscle less. The result is a decrease in muscle tone
. Against this background, compensatory tension of the muscle located on the opposite side of the jaw develops.
With muscle pain syndrome, the patient experiences constant pain in the area of the masticatory muscles, which intensifies with movement of the lower jaw. When closing and opening the jaws, a clicking sound is heard in the TMJ. Visually, zigzag deviations of the jaw to the side or forward are observed. Bruxism develops
. Sometimes pain syndrome manifests itself in the upper jaw, sinuses, superciliary arches, and ringing or noise in the ears develops.
How to prevent trismus
There are 4 main ways to prevent trismus:
- massage your jaw muscles;
- train your jaw muscles;
- maintain good posture;
- Maintain proper oral hygiene.
This should be done even if there are no symptoms of trismus to prevent it. Follow the directions in the section below. If you have had surgery, ask your healthcare provider if it is safe before you have surgery.
You may need a timer or watch to help you hold the stretching position for the required amount of time. Breathe normally and do not hold your breath. If you feel pain, numbness, or tingling, stop immediately and call your healthcare provider.
Massage your jaw muscles
Press your index and middle fingers against your cheekbone. Use your fingers to massage the masseter muscle, which is attached to the lower jaw (see Figure 3). As you move your fingers, look for areas that are tender or tight. Massage these areas with circular movements of your fingers for 30 seconds. Do this 2-3 times a day.
Try not to clench your jaw when you are stressed or out of habit. This will help relax your jaw muscles.
Figure 3. Massage the jaw muscles
Train your jaw muscles
Perform these exercises 3 times every day. You can do them standing or sitting. Use a mirror to help you do the exercises correctly.
These exercises will help stretch the muscles well, but should not cause pain. If an exercise causes pain or discomfort, try doing it with less effort. If pain or discomfort persists, contact your healthcare provider.
Range of motion and stretching exercises
Your head should remain in one position while performing these exercises. Repeat these steps 5 times.
- Open your mouth as wide as possible until you feel a good stretch but no pain (see Figure 4).
Hold this position for 10 seconds. Figure 4. Opening your mouth as wide as possible - Move your lower jaw to the left (see Figure 5). Hold this position for 3 seconds.
- Move your lower jaw to the right (see Figure 6). Hold this position for 3 seconds.
Figure 5. Jaw shift to the leftFigure 6. Jaw shift to the right
- Make circular movements with your lower jaw to the left.
- Make circular movements with your lower jaw to the right.
Passive stretching exercise
Figure 7. Press your thumb and index finger against your teeth.
Repeat these steps 5 times.
- Press your thumb against your upper teeth in the middle of your jaw.
- Press the index finger of your other hand against your lower teeth in the middle of your jaw (see Figure 7).
- Open your mouth as wide as possible. Place additional emphasis with your fingers so that your mouth does not close. You should feel a slight stretch, but not pain. Hold this position for ______ seconds.
Maintain proper posture
Correct posture means sitting and standing with your ears, shoulders, hips, knees and ankles aligned horizontally (see Figure 8). To have correct posture, it is necessary to maintain good tone and stretch in the muscles of the neck and shoulders. The following exercises will help you with this.
Figure 8. Correct posture
Do them 2 times every day. You can do them standing or sitting with your arms at your side.
Neck stretch
Repeat these steps 5 times. Hold each stretch for 30 seconds.
- Tilt your head forward (see Figure 9).
- Tilt your head back (see Figure 10).
Figure 9. Head tilt forwardFigure 10. Head tilt back
- Turn your head to the right (see Figure 11).
- Turn your head to the left (see Figure 12).
Figure 11. Turning the head to the rightFigure 12. Turning the head to the left
- Tilt your head, trying to bring your left ear closer to your left shoulder (see Figure 13).
- Tilt your head, trying to bring your right ear closer to your right shoulder (see Figure 14).
Figure 13. Head tilt to the leftFigure 14. Head tilt to the right
Chin retraction
Figure 15. Retraction of the chin when pulling the head back.
Repeat these steps 5 times.
- Looking forward, tuck your chin.
- Pull your head back so that your ears are level with your shoulders (see Figure 15). Stay in this position for 3 seconds.
Scapula compression
Repeat these steps 5 times.
- Tuck your chin in as described in the exercise above.
- Squeeze and squeeze your shoulder blades together as hard as possible (see Figure 16).
- Stay in this position for 3 seconds.
Figure 16. Squeezing the shoulder blades together
Maintain proper oral hygiene
- Brush your teeth and tongue in the morning after sleep, after every meal and before bed.
- If you have removable dentures, remove and clean them every time you brush your teeth. Don't go to bed with dentures in your mouth.
- Floss your teeth once a day before bed.
to come back to the beginning
Symptoms of TMJ problems
The disease manifests itself with the following symptoms:
- Painful sensations occur on palpation.
- When opening the mouth, the patient feels a sharp pain.
- Due to pain, a person experiences difficulty eating and communicating.
- Breathing through the mouth is difficult.
- To the touch, the chewing muscles are compacted and slightly increased in volume.
- Facial asymmetry with unilateral spasm.
- Low-grade fever.
- Headache.
The gnathologist
carries out differential diagnosis with a fracture or dislocation of the jaw, as well as with an infectious lesion.
There are three degrees of disease progression: mild (the patient is able to open his mouth four centimeters), moderate (the mouth opens two centimeters), severe (the patient cannot open his mouth more than one centimeter).
How long does it take to cure trismus?
Typically, full muscle recovery can take one to three weeks, depending on the cause of the trismus. More time will be needed for fractures of the jaw, which must heal properly and subsequently develop.
To prevent trismus of the masticatory muscle, you must:
- do not cause diseases of teeth and gums;
- get vaccinated against rabies and tetanus (rabies and, as a result, lockjaw can be fatal);
- In case of blows or damage to the jaw, seek emergency help from dentistry;
- avoid stressful situations, nervous tension;
- when engaging in contact sports, wear special helmets and mouthguards for protection;
- undergo regular preventive examinations with a trusted dentist. These are the doctors who work in the 32 Dent network of clinics, where you will be happy to see you at any time. Contact us!
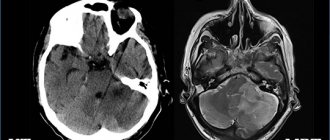
Diagnostics
The patient experiences pain from jaw movement. In this situation, it is necessary to consult a doctor as soon as possible to begin treatment. It is necessary to find out how to relieve jaw muscle spasm in order to restore health.
During the examination and history taking, the doctor observes the patient, paying attention to his posture and head tilt, neck movements, facial expressions, and facial expressions. The state of the muscles during speaking and swallowing is determined. The presence of the corneal reflex is checked, and the amplitude of movements of the lower jaw is determined. The doctor finds out whether there are problems with the spine.
The patient is examined using diagnostic equipment, an occlusiogram is prescribed to determine the type of bite, and its dynamics and statics are measured. If necessary, an X-ray of the TMJ and an orthopantomogram of the jaws are prescribed, and an electromyographic study is performed.
In case of spasm of the masticatory muscles when opening the mouth
The sooner you begin treatment for spasms of the masticatory muscles, the easier it will be to resume normal jaw function. If you experience tension in your jaw, call your healthcare provider immediately. He or she may refer you to a specialist, as described below.
- See a speech and swallowing specialist, a physical therapist, or both. They will help you maintain your ability to open your mouth and regain any lost abilities. These professionals use a variety of techniques, such as exercise, stretching and massage. They may also recommend that you use special devices to help open your mouth.
- See a rehabilitation doctor. He will evaluate how well you can open your mouth. He or she may prescribe medications for pain or spasms (sudden, strong muscle contractions), suggest other treatments, or recommend medical devices to help you.
Your healthcare provider will discuss with you which specialist referral would be most beneficial for you.
to come back to the beginning
Prevention of hypertonicity of the TMJ muscles
Preventive measures against hypertonicity of the lower jaw muscles will help prevent the disease with an integrated approach. It is much easier to follow the general recommendations of doctors than to face a painful spasm of the TMJ. Prevention includes the following activities:
- Preventive visits to the doctor every six months.
- Careful systematic oral hygiene.
- Treatment of caries at its first symptoms.
- Orthodontic treatment for malocclusion pathologies.
- Disinfection of food products.
- Antitetanus therapy for animal bites.
- A set of necessary vaccinations.
- Do not open your mouth wide (jaw dislocations often occur when trying to bite off a large fruit).
- Do not overuse solid foods and do not chew nuts with your teeth.
- Avoid stressful situations, react less to stress.
Causes of jaw clenching during trismus
- inflammation of the masticatory muscles;
- inflammation of the gums;
- caries;
- abscess;
- inflammation of the periosteum of the lower jaw;
- jaw injuries (cracks, fractures, dislocations);
- dousing with cold water;
- animal or insect bites.
Trismus can also be a consequence of the following diseases:
- osteomyelitis of the jaw;
- periostitis;
- neurosis;
- epilepsy;
- meningitis;
- hysteria;
- arthrosis of the jaw joint;
- cancerous tumors;
- convulsions;
- rabies;
- tetany;
- paralysis;
- tetanus;
- pulpitis in the acute stage, etc.
Consequences of jaw spasm
Trismus is unpleasant for a person not only due to pain. When opening and closing the mouth is painful, the normal process of eating is disrupted and the gastrointestinal tract suffers. When the jaw spasms, breathing is impaired, which leads to constant oxygen starvation of the brain and headaches. This affects the composition of the blood and the functioning of the cardiovascular system.
Trismus caused by infections or tumors causes serious health problems. In this case, long-term serious treatment is required. In the initial stages, pain is completely relieved. For systemic diseases, when trismus is a secondary symptom, complex therapy is necessary.
Hypertonicity of the masticatory muscles and its correction with BTA for aesthetic problems of the lower half of the face
Soykher M.I., Orlova O.R., Mingazova L.R., Soykher M.G.
The aesthetic appearance of the lower half of the face reflects the morphology of the dental system and the function of the masticatory muscles. In aesthetic medicine, the problems of correction of the lower third of the face remain relevant, despite the accumulated many years of experience. The functional state of the masticatory muscle is associated with the configuration of the lower third of the face and possible asymmetry, which hides a combination of dental and neurological problems that require a detailed examination and adequate treatment of the patient. Some diseases, such as bruxism and oromandibular dystonia, are accompanied by hypertrophy of the masticatory muscles, which occurs as a result of their forced contraction, and the massive lower third of the face becomes an aesthetic manifestation here.
Keywords:
Facial disproportion; hypertrophy of the masticatory muscles; bruxism; oromandibular dystonia; myofascial pain syndrome; botulinum toxin type A
Soykher Marina Ivanovna, candidate of medical sciences, dentist, head. Doctor of the Center for Interdisciplinary Dentistry E-mail
Orlova Olga Ratmirovna, Doctor of Medical Sciences, Professor of the Department of Nervous Diseases of the Faculty of Faculty of Physics, First Moscow State Medical University named after. I. M. Sechenova, President of the MoESBT E-mail
Mingazova Leniza Rifkatovna, candidate of medical sciences, neurologist, employee of the department of nervous diseases of the State Educational Institution of Higher Professional Education MMA named after. I. M. Sechenova E-mail
Soykher Mikhail Grigorievich, candidate of medical sciences, dentist, leading specialist of the Center for Interdisciplinary Dentistry E-mail
INTRODUCTION
“Everything in a person should be beautiful.” Today, more and more people are striving to implement this principle in their own lives <2>. Almost every person pays attention to his appearance, and attaches special importance to how his face looks <3, 4>. Dissatisfaction in this case can become quite a serious problem and affect both the psychosomatic state (causing depression, uncertainty, neuroses...), and professional status, family and personal relationships.
In aesthetic medicine, the problems of correction of the lower third of the face remain relevant, despite the accumulated many years of experience. According to a survey of patients, the main complaint they present is facial disproportion, in particular the “square face” problem. What is meant by the expression “square” (or “trapezoidal”) face?
In domestic and foreign medicine, for a brief answer to this question, they use such characteristics as protruding angles of the lower jaw, hypertrophy of the masticatory muscles themselves, prominent contours of the lower zone of the face, angular contours of the face (prominent mandibular angle, hypertrophy of the masseter, lower facial contour). The contours and shape of the lower half of the face are determined by the relative position of the upper and lower jaws (occlusal relationship), the size and shape of the lower jaw, as well as the condition of the masticatory muscles.
The lower jaw is suspended in space to the fixed bones of the skull with the help of muscles and ligaments. The only support for it is the chewing teeth. It is the teeth that fix the position of the jaw in three mutually perpendicular planes. When the position of the teeth and, accordingly, the dentition changes or their loss, the position of the jaw in space also changes. In most cases, there is a decrease in the lower third of the face, distalization of the bite, with characteristic facial manifestations. There are disturbances in the coordination of the masticatory muscles and temporomandibular joints. The dentition, the geometry of which is normally designed to compensate for the complex biomechanics of the chewing function of the cranial-maxillary system, simultaneously serves as support for the soft tissues of the face, which must be taken into account during the aesthetic rehabilitation of patients.
The four chewing muscles on each side are interconnected genetically (they originate from one branchial arch - the mandibular), morphologically (they are all attached to the lower jaw, which they move during their contractions) and functionally (they perform chewing movements of the lower jaw, which determines their location) .
M. masseter is a chewing muscle that starts from the lower edge of the zygomatic bone and zygomatic arch and is attached to the tuberositas masseterica and to the outer side of the ramus of the lower jaw. It has the shape of an irregular rectangle and consists of a superficial part and a deep part. The strongest muscle in the human body in terms of force generated - on molars it develops a force of up to 72 kg.
M. temporalis is the temporal muscle, with its wide origin it occupies the entire space of the temporal fossa of the skull, reaching at the top to the linea temporalis. The muscle bundles converge in a fan-shaped manner and form a strong tendon, which fits under the zygomatic arch and is attached to the processus coronoideus of the lower jaw.
M. pterygoideus lateralis - lateral pterygoid muscle, starts from the lower surface of the greater wing of the sphenoid bone and from the pterygoid process and is attached to the neck of the condylar process of the mandible, as well as to the capsule and to the discus articularis of the temporomandibular joint.
M. pterygoideus medidlis - medial pterygoid muscle, originates in the fossa pterygoidea of the pterygoid process and is attached to the medial surface of the angle of the mandible, symmetrically m. masseter, to the tuberosity of the same name..
M. masseter, m. temporalis and m. pterygoideus medialis, with the mouth open, pull the lower jaw towards the upper, in other words, they close the mouth.
With the simultaneous contraction of both muscles of the pterygoidei laterales, the lower jaw moves forward. The reverse movement is produced by the most posterior fibers of m. temporalis, running almost horizontally from back to front. If m. pterygoideus lateralis contracts only on one side, then the lower jaw moves to the side, in the direction opposite to the contracting muscle. M. temporalis gives a certain position to the lower jaw during speech, thereby ensuring the articulation of the latter.
The masticatory muscle, in addition to chewing movements, takes part, together with the facial muscles, in the articulation of speech sounds, facial expressions, yawning, and swallowing. We can say that this muscle is in a state of “chronic fitness”. Excessive prolonged activity of the masticatory muscles leads to their hypertrophy, which is characterized by an increase in strength and muscle mass (Fig. 5).
The functional state of the masticatory muscle is associated with the configuration of the lower third of the face and possible asymmetry, which hides a combination of dental and neurological problems that require a detailed examination and adequate treatment of the patient. Some diseases, for example, bruxism and oromandibular dystonia, are accompanied by hypertrophy of the masticatory muscles, which occurs as a result of their forced contraction, and their aesthetic manifestation is a massive lower third of the face <6–10>.
The purpose of the study is to study the relationship between the condition of the masticatory muscles and the aesthetic appearance of the lower half of the face; to evaluate the effectiveness of using the botulinum toxin type A drug "Lantox" in order to reduce hypertonicity and correct hypertrophy of the masticatory muscles under the control of surface electromyography.
MATERIALS AND METHODS
40 patients were examined. The average age is 35 years. In order to understand whether problems of an aesthetic nature are caused by pathological processes in the dental system, we conducted a dental and neurological study, which included:
analysis of anamnestic data; clinical study of the masticatory muscles, muscles of the neck and upper shoulder girdle, and the area of the temporomandibular joint (TMJ);
- occlusiogram, analysis of the static and dynamic organization of occlusion;
- orthopantomogram;
- TMJ tomogram;
- teleradiography (TRG) of the lateral surface of the head with markers;
- photoanalysis (portrait and intraoral photographs);
- axiography;
- functional analysis of jaw models in an articulator;
- diagnostics of parafunctions using brookscheckers;
- electromyography (EMG) of the masticatory and neck muscles.
When examining the patient, attention was paid to the following clinical signs: head position, range of active movements in the cervical spine; facial expression, state of the facial muscles when speaking, swallowing, signs of blepharospasm, oromandibular dystonia, facial asymmetry; corneal reflex and reflex from the nasal mucosa, the state of the muscle ridges at rest and when clenching the teeth; volume of active movements of the lower jaw - the distance between the incisors (in cm) when opening the mouth, the trajectory of movement of the lower jaw; mandibular reflex; volume of active movements of facial muscles, brow and orbicular reflexes; Chvostek's sign; sensitivity on the face, oral mucosa and tongue.
Myograph "Synapsis" dental
Electroneuromyograph for maxillofacial studies and monitoring the effectiveness of therapeutic measures.
More details
The study of the state of the musculoskeletal system included: identification of biomechanical static disorders - scoliosis, asymmetry of the shoulders, shoulder blades and other deformities; identification of the “short leg”.
During palpation examination, we used a 3-point scale for assessing muscle tension and soreness:
0 points - no tension and no pain;
1 point - slight muscle tension, no pain on palpation;
2 points - moderate muscle tension and pain on palpation;
3 points - severe muscle tension and sharp pain on palpation, the presence of painful muscle tightness and/or trigger points.
EMG indicators were recorded using an electromyograph “Synapsis” (NMF “Neurotech”, Taganrog), supplemented with special software. Injections of botulinum toxin into the masticatory muscles were carried out under the control of electromyography; for this purpose we used the Mist device (NMF Neurotech, Taganrog).
During the clinical study, 2 groups of participants were identified:
Group 1 - 30 patients who suffered from bruxism: 25 women, 5 men;
Group 2 - 10 patients with signs of focal muscular dystonia (the leading syndrome of oromandibular dystonia): 8 women, 2 (two) men.
"MIST" professional
Myographic control of injections, biofeedback training, anesthesia regimen.
More details
Clinical features
1st group. In dental practice, bruxism is defined as parafunctional activity of the masticatory muscles. The following parafunctions of the masticatory muscles have been described (arranged in descending order of frequency): clenching the teeth, moving the lower jaw forward or to any side, inserting the tongue between the teeth, biting the tongue and lips, grinding the teeth, rhythmic movements of the tongue and submandibular muscles <12–13> . Only 10 patients from group 1 noted grinding and grinding of teeth at night. The rest had the habit of clenching their teeth tightly during the day in response to even minor emotional stress. A hereditary factor (bruxism in close relatives) was determined in all patients in this group. The history also included episodic pain in the face of muscular origin (myofascial pain syndrome of the face), frequent headaches caused by tension in the pericranial muscles. All patients complained of fatigue of the masticatory muscles in the morning. When studying the aesthetic appearance of the face, a massive lower third was determined due to hypertrophy of the masticatory muscles, which caused considerable concern, especially in women.
Dental status in patients of group 1: violation of the integrity of the dentition (absence of one or more teeth), pathological abrasion of teeth, the presence of wedge-shaped defects in the cervical area.
Clinical examination of the masticatory muscles revealed signs of hypertrophy; the muscles are dense, tense, with the presence of painful muscle compactions (myofascial trigger points). When palpating the masticatory muscle itself, in 20 patients the pain radiated to the upper and lower jaws, upper and lower molars, ear, frontal region, TMJ, and neck. In 22 patients, palpation in the area of the tubercle of the upper jaw was sharply painful.
Tenderness or discomfort in the medial pterygoid and digastric muscles was also noted. All patients had muscle tension in the floor of the mouth and limited mobility of the hyoid bone; in 10 patients there was tension and slight hypertrophy of the sternocleidomastoid muscle. Palpation of the muscles on the opposite side was painless or moderately painful.
In 40% of patients, pain occurred on palpation of the lateral pole of the joint head during rotation on both sides, and the temporomandibular ligament on both sides. Discomfort when palpating the lateral pole of the joint head in static conditions on both sides.
In 25% of patients, there was a restriction in mouth opening due to pain to 1.5±2.2 cm between the incisors (normally from 4.6 to 5.6 cm). Further lowering of the lower jaw due to the appearance of sharp pain became almost impossible. There was also a restriction in the movement of the lower jaw forward and to the side.
Only 20% of patients experienced a clicking or crunching sound when opening their mouths. Pain sensitivity of the facial skin and oral mucosa was not changed.
When conducting surface electromyography of the masticatory muscles and neck muscles, the following results were obtained: asymmetry in the work of the temporal, masticatory muscles, high rates of the total biopotential of the muscles under study.
When analyzing a chewing test, a violation of the symmetry of chewing, frequency, amplitude, phase and total biopotential of chewing is noted.
2nd group. Oromandibular dystonia (OMD) is hyperkinesis involving the muscles of the perioral region and masticatory muscles. In patients of group 2, the following clinical forms of OMD were determined: spasm of the muscles that close the mouth and compress the jaw (dystonic trismus) - in 6 people; constant trismus with lateral jerking movements of the lower jaw, bruxism and hypertrophy of the masticatory muscles - in 4 people. Subjectively, all patients of the 2nd group complained of unpleasant sensations, which were described as “periodic movement of the lower jaw”, “the jaw moves to the side”, “it is impossible to find a comfortable position of the jaw”, “forcible clenching of the teeth”, “teeth chattering against each other” friend."
Clinical examination of the masticatory muscles revealed signs of hypertrophy; muscles are dense, tense, with the presence of painful muscle thickening (myofascial trigger points). As a rule, the masticatory muscle itself undergoes pronounced changes, while the temporal and pterygoid muscles undergo smaller changes. Three patients had asymmetric dystonia. Visually, this phenomenon was manifested by asymmetry of the lower half of the face (the volume of the hypertrophied masseter muscle on one side is more pronounced than on the other).
Also, in all patients of group 2, subcompensated signs of dystonic phenomena in other areas were determined: blepharospasm, mild and moderate forms of cervical dystonia, dystonic tremor of the head and upper extremities, writer's cramp.
Dental status: in patients of the 2nd group, there was a violation of the integrity of the dentition (the absence of one or more teeth), pathological abrasion of teeth, and the presence of wedge-shaped defects in the cervical region. When conducting surface electromyography of the masticatory muscles and neck muscles, the following results were obtained: asymmetry in the work of the temporal, masticatory, and neck muscles, torsional twisting of the lower jaw, an increase in the functional activity of the neck muscles and the total biopotential of the muscles under study. When analyzing the chewing sample, a violation of the symmetry of chewing, frequency, amplitude, phase and total biopotential of chewing was noted.
For therapeutic and aesthetic purposes, all patients received injections of botulinum toxin type A (BTA) “Lantox” (Lanzhou Institute, China). It was injected into the masseter proper, temporalis, medial and lateral pterygoid muscles. Large doses were injected into the masticatory muscle itself from the outside (5–10 units at one point). For a more uniform distribution of the drug throughout the muscle, it is injected into several points (from 4 to 8), 1-2 injections are carried out from the oral cavity. In patients with an asymmetric form of dystonia, large doses of the drug were also administered on the side of the larger muscle. The average total dose of BTA (Lantox) was 100 units per procedure.
RESULTS
Analysis of clinical data showed that in patients of group 10 suffering from bruxism, on days 2–10 after injections, the feeling of fatigue in the masticatory muscles in the morning disappeared and headaches stopped. By days 14–21, a decrease in the massiveness of the lower half of the face became noticeable. Against this background, the necessary dental procedures were successfully carried out.
"Hummingbird" dental
Express assessment of the level of bruxism, study of facial muscle tone, wireless technologies.
More details
Due to the weakening of the masticatory muscles, the phenomena of bruxism and the phenomenon of clenched jaws ceased for some time. During this time, patients were advised to fix their attention on the facial muscles, consciously relax the lower jaw, open the dentition and try to form a new motor stereotype of the masticatory muscles (based on the principle of biofeedback). For this purpose, disconnecting splints were used on the lower jaw.
In patients of group 2 (OMD), the signs of hyperkinesis were also leveled out already on days 10–12 after injections due to weakening of the activity of the masticatory muscles, which significantly improved the quality of life of patients. Unpleasant subjective sensations disappeared, and the opportunity for dental treatment appeared. In patients with asymmetric dystonia, the symmetry of the lower half of the face was restored.
The study demonstrated the positive effect of BTA (Lantox) on the functional and morphological state of the masticatory muscles, and a good clinical effect alleviated the condition of patients and made it possible not to use any medications.
CONCLUSIONS
The aesthetic appearance of the lower half of the face reflects the morphology of the dental system and the function of the masticatory muscles. In aesthetic practice, it is necessary to conduct a detailed clinical analysis of the condition of the masticatory muscles, especially in patients with a massive lower half of the face. Patients with increased tooth wear and failing dentures require a detailed neurological examination to exclude bruxism and oromandibular dystonia. Injections of botulinum toxin into the masticatory muscles are the method of choice for this group of patients. The drug botulinum toxin type A (Lantox) at a dose of 100 units per procedure is effective and safe for the treatment of hyperactivity of the masticatory muscles in neurological, dental and aesthetic practice.
LITERATURE
1. Budylina S.M., Degtyareva V.P. Physiology of the maxillofacial region. - M: Medicine, 2001. - P. 87–156.
2. Goldstein R. Aesthetic dentistry. Volume 1. - M.: Stbook. - 2005. - P. 10–14.
3. Kalyuzhny D.V. Physiological mechanisms of regulation of pain sensitivity. - M.: Medicine, 1984. - P. 102–114.
4.Karlov V.A. Neurology of the face. - M.: Medicine, 1991. - 284 p.
5. Kupriyanov V., Stovichek G. Human face. - M.: Medicine, 1988. - 272 p.
6. Mingazova L.R. Pathogenesis and treatment of myofascial pain syndrome of the face // Clinical materials. conference of young scientists FPPO MMA named after. I.M. Sechenov “Current issues of clinical medicine.” - M., 2002. — pp. 54–58.
7. Mingazova L.R. Clinical and physiological analysis and treatment of myofascial pain syndrome of the face. Abstract of thesis. dis…. Ph.D. honey. Sci. - M., 2005. - 25 p.
8.Orlova O.R. Focal dystonia: clinical picture, pathogenesis, treatment using botulinum toxin // Diss.... Dr. med. Sci. - M., 2000. - P. 13–29.
9.Orlova O.R., Mingazova L.R., Vein A.M. Facial pain of a muscular nature: clinical and physiological characteristics and treatment with botulinum toxin type A (dysport) // Abstracts of the Russian scientific and practical conference “Clinical and theoretical aspects of acute and chronic pain”. - Nizhny Novgorod, 2003. - pp. 113–115.
10.Orlova O.R. Focal dystonia: clinical picture, pathogenesis, treatment using botulinum toxin. Dissertation for the degree of Doctor of Medical Sciences. - Moscow, 2000. - pp. 13–29.
11.Orlova O.R., Yakhno N.N. The use of Botox (botulism toxin type A) in clinical practice. - M., 2001. - P. 143–147, 161–163.
12. Orlova O.R., Mingazova L.R., Vein A.M. Myofascial pain syndrome of the face: new aspects of the clinic, pathogenesis and treatment // New in dentistry. - 2003. - No. 1. — pp. 25–29.
13.Petrov E.A. Electrophysiological characteristics of pain syndrome of temporomandibular joint dysfunction // Ross. dental magazine. - 2002. - No. 6. - P. 34–35.
14.Petrosov Yu.A., Skorikova L.A. Prevention of TMJ dysfunctions by eliminating parafunctions of the masticatory muscles // Abstracts of the V All-Russian. Congress of Dentistry: Prevention of dental diseases. - Novosibirsk - M., 1988. - P. 156–157.
15.Al-Ahmad HT, Al-Qudah MA. The treatment of masseter hypertrophy with botulinum toxin type. — A. Saudi Med. J. - 2006. - 27. R. 397–400.
16.Gurney CE Chronic bilateral benign hypertrophy of the masseter muscle //Am. Surg. - 1947. - No. 73. - P. 137.
17.Moore AP, Wood GD The medical management of masseteric hypertrophy with botulinum toxin type A // Br. J. Oral Maxillofac Surg. - 1994. - No. 32. - P. 26–28.
18. Sannomiya E., Goncalves M., Masseter muscle hypertrophy // Bras. Dent. J. - 2009. - No. 17 (4). — R. 347–350.
19. Slavicek R. The masticatory organ: Function and Dysfunction.
— Kloster neuburg: Gamma Med. — wiss. Fortbildungs - GmbH, 2006. - R. 59–90. toxin type A // Saudi Med. J. - 2006. - No. 27. - P. 397–400. come back