Subcortical (extrapyramidal) dysarthria is a pathological condition of the brain that is accompanied by speech dysfunction. Impaired sound pronunciation in extrapyramidal dysarthria is caused by damage to the subcortical ganglia. As a result, a person experiences difficulties in pronouncing words, intonation, and controlling the expressiveness of speech. This disease requires elimination of the cause that caused the speech defect and regular speech therapy sessions. At the Yusupov Hospital, patients with subcortical dysarthria are provided with the necessary assistance to correct this condition. Here you can undergo high-quality diagnostics to identify the true cause of the pathology.
Subcortical dysarthria: characteristics
Subcortical dysarthria implies a disorder of sound pronunciation as a result of impaired muscle tone and insufficient innervation. The condition accompanies hyperkinesis, when involuntary movements of the speech apparatus occur (more often this manifests itself during the speech act, but can also be observed at rest).
Pathology occurs as a result of dysfunction of subcortical structures that are located outside the main motor pathways, that is, in the extrapyramidal system. The subcortical nodes, damage to which causes dysarthria, include some nuclei and ganglia:
- Caudate nucleus;
- Subthalamic nucleus;
- Red core;
- Shell;
- Substantia nigra;
- Pale ball.
The extrapyramidal system is responsible for muscle tone and involuntary movements. With its dysfunction, speech disorders are observed as a result of disruption of the motor sphere of subcortical structures. The extrapyramidal system is interconnected with the cerebellum through peripheral pathways of the central nervous system. The cerebellum controls motor coordination, balance, and muscle tone. Therefore, when the components of these structures are pathological, a distorted nerve impulse enters the cells of peripheral motor neurons and the spinal cord, which is reflected in dysarthria.
LECTURES ON NEUROPSYCHOLOGY: Lecture No. 11. 5/5 (3)
Lecture 11. Neuropsychological syndromes of damage to deep subcortical brain structures
- General position of the problem 2. syndromes of damage to the median nonspecific structures of the brain. 3. syndromes of damage to the median commissures of the brain 4. syndromes of damage to deep hemispheric subcortical structures
The problem of neuropsychological syndromes associated with damage to the deep subcortical structures of the cerebral hemispheres arose in neuropsychology relatively recently, primarily in connection with the success of neurosurgery in the treatment of subcortical formations. Under the influence of facts obtained in the process of research, new views on the cerebral organization of higher mental functions began to take shape, in which an increasing role began to be assigned to the principle of vertical (cortical-subcortical) cerebral organization of mental functions.
Ideas began to emerge about a certain specific role of subcortical structures in the brain mechanisms of mental processes. Currently, the accumulation of material in this area of science is proceeding in two directions. 1. More and more new data are emerging on the results of destruction (or irritation) of subcortical formations during stereotactic operations on patients suffering from parkinsonism, muscular dystrophy and other diseases.
The study of neurological symptoms arising from stereotactic influences gave rise to a new direction in neurology, called stereotactic neurology by its founder V. M. Smirnov (1976).
- traditional, clinical research. This is a study of patients with organic brain lesions (tumors, vascular lesions, etc.), localized in subcortical structures and having relatively little effect on the cerebral cortex.
However, the available diagnostic methods did not allow us to determine with great accuracy whether the lesion was localized only in the subcortical structures (and where exactly) or whether it also extended to the cerebral cortex. Currently, the introduction of new methods of technical diagnostics (and above all computed tomography) makes it possible to answer these questions quite accurately.
The problem of neuropsychological syndromes that arise with deep subcortical lesions is associated with the solution of a new theoretical question about the nature of the factors that underlie these syndromes, i.e., about the nature of the “interference” that a lesion of a particular subcortical structure introduces into the work of functional systems , providing the brain organization of higher mental functions.
Three types of neuropsychological syndromes associated with damage to deep brain structures can be distinguished. The first type is syndromes of damage to the median nonspecific structures of the brain. These syndromes occur when nonspecific structures of different levels are affected, ranging from the lower parts of the brain stem to the mediobasal parts of the cortex of the frontal and temporal lobes. Damage to these structures causes a disruption in the functioning of modality-nonspecific factors.
In nonspecific “deep” syndromes, three main groups of symptoms can be distinguished: the first group is neurodynamic disorders (or disorders of the dynamic aspect) of all higher mental functions in the form of a decrease in their speed, productivity, uneven efficiency in completing tasks, etc.
Also modal-nonspecific disturbances of attention in the form of general absent-mindedness, difficulty concentrating, easy distractibility, etc. The second group is selective disturbances of memory and emotional processes. The patients do not have obvious defects in other cognitive processes. Memory impairments are modally nonspecific, that is, they do not depend on the modality of the material being remembered.
Short-term memory is predominantly affected, while long-term (for example, professional) memory is relatively preserved. Emotional disturbances can manifest themselves in the form of emotional excitability, increased reactivity or affective paroxysms, outbursts of negativism, and anger.
The general structure of the emotional-personal sphere is disrupted in different ways. In some cases, it is relatively intact, and the patient adequately evaluates himself and those around him. In other cases, emotional-personal relationships reach the stage of a gross defect; the third group of symptoms are changes in the state of consciousness, which manifest themselves in the acute stages of the disease in the form of blackouts.
Syndromes of damage to nonspecific brain formations are specific depending on the level of damage. Level of the lower parts of the brain stem. Damage to this level of the nonspecific system in the acute stage of the disease is accompanied by loss of consciousness (its duration depends on the severity of the disease) followed by amnesia for the events preceding the injury. In the future, patients usually experience: • disturbances in the sleep-wake cycle, reduced level of wakefulness; • exhaustibility; severe fatigue, intolerance of patients; • fairly clear orientation in the environment (place, time); • preservation of personal reactions in general. Patients are adequate in their complaints and critical of their condition.
Against this background, the central symptoms are: • modal-nonspecific mnestic disorders with primary short-term memory disorders; • reduction in the volume of memorization (down to three or four words); • increased inhibition of traces by extraneous stimuli.
At the same time, increased motivation gives a clear compensatory effect, which indicates the preservation of the general structure of mental functions.
Level of diencephalic parts of the brain. (hypothalamic-pituitary system) Hypothalamic-diencephalic syndrome includes autonomic disorders, pathological visual symptoms, hormonal, metabolic disorders, etc. The neuropsychological picture of their disease consists of symptoms similar to those observed with damage to the lower parts of the trunk. These patients also have disturbances in the sleep-wake cycle and a decrease in overall functional state. They also have disturbances in the emotional and personal sphere in the following form: • increased emotional reactivity; • instability of emotional reactions; • changes in emotional states (depression or mild euphoria).
The difference between these patients and those described above is that they have more severe memory impairments (of a modality-nonspecific type), which are associated primarily with increased trace inhibition.
With massive lesions in these areas of the brain, severe mental changes occur, similar to the “frontal” syndrome, including severe disturbances in emotional states and personal reactions.
Limbic system level. The central formation of this level is the cingulate gyrus. Characterized by severe impairments of short-term memory for current events (of a modality-nonspecific type), occurring in the form of Korsakov's syndrome. Damage to this level of the nonspecific system is also associated with disturbances of consciousness and changes in the emotional sphere.
Neuropsychological syndromes of damage to the cingulate gyrus consist of the following: • modally nonspecific memory impairments, which may be similar to mnestic defects in “frontal” patients; • violations of trace selectivity; • attention disorders; • violations of the emotional and personal sphere (in the form of uncriticality, inadequacy of emotional reactions, etc.); • contamination; (false reproduction of information, characterized by the unification in the image of a concept - parts belonging to different events) • in severe cases - persistent disturbances of consciousness.
The level of the mediobasal cortex of the frontal and temporal lobes of the brain. The mediobasal frontal and temporal cortex are closely connected with nonspecific formations of the brainstem and limbic structures and can be considered as cortical sections of a nonspecific system.
Damage to these structures leads to the appearance of a number of similar neuropsychological symptoms, disturbances: • consciousness (some confusion, confabulation, disturbance of orientation in place, more often in time); • mnestic processes (modality-nonspecific violations of short-term memory); • attention (modality-nonspecific disorders); • emotional sphere (efficiency, temper, etc.).
There are differences between the syndromes due to the level of damage to nonspecific structures. The greatest differences are observed between syndromes associated with damage to the level of the mediobasal cortex of the frontal and temporal lobes and subcortical levels.
The second type is syndromes of damage to the median commissures of the brain. The main median commissure of the brain is the corpus callosum, which connects the right and left hemispheres with many fibers.
The corpus callosum unites the anterior (frontal), middle (temporal, parietal) and posterior (occipital) sections of the cerebral hemispheres and is divided into anterior, middle and posterior sections. For a long time, the symptoms of damage to the median commissures of the brain were unknown.
Since the 60s of the 20th century, commissurotomy surgery has been used in a number of countries to treat epilepsy. Studies of patients who underwent surgery to transect the corpus callosum (full or, more often, partial) (1964) showed that after such an operation a whole complex of new, previously unknown symptoms appeared, which were designated as “split brain” syndrome. Deterioration or cessation of normal interaction of the cerebral hemispheres can be regarded as an independent factor (or factors). Split brain syndrome consists of a range of symptoms. These symptoms vary at different stages of the postoperative condition.
At the first stage (immediately after surgery), patients experience severe memory impairment and sometimes confusion, but later these symptoms disappear
At the second stage, there are clearly defined violations of coordination movements in which both limbs are involved (for example, typing, riding a bicycle, etc.). At the same time, these movements are not disturbed if the patient performs them with one hand. Speech symptoms: difficulty naming objects presented to the left halves of the visual fields (when visual information enters the right hemisphere). Experiments have shown that patients recognize the objects shown, but cannot name them. This symptom was called "anomia". Patients cannot read the word “illiterate” presented to the right hemisphere, although they understand its general meaning.
A special group of symptoms is “discopia-dysgraphia”: they cannot write and draw with the right and left hands, as a healthy person does (although it is better with the dominant hand): with one hand they can only draw, and with the other - only write. All these symptoms can be explained by a violation of the mechanisms of interaction of the cerebral hemispheres in the visual and motor systems. With partial transection of the corpus callosum, three independent variants of the “split brain” syndrome can be distinguished, associated with the site of transection.
Option 1: when cutting the anterior sections of the corpus callosum, disturbances in the interaction of the hemispheres manifested themselves mainly in the motor sphere; Option 2: when cutting the middle sections, disturbances in interaction manifested themselves mainly in the tactile sphere; Option 3: during transection of the posterior sections, disturbances in interaction manifested themselves mainly in the visual system. A feature of syndromes of partial disruption of the interaction of the cerebral hemispheres is their dynamism. The symptoms that arise from partial transection of the corpus callosum are unstable and disappear fairly quickly.
Thus, a neuropsychological study of HMF disorders following damage to different parts of the corpus callosum has made it possible to establish that it is not a single organ, but a differentiated system, individual sections of which provide various aspects of interhemispheric interaction. The specialization of the corpus callosum is built on the principle of modal specificity, however, in addition to clearly modal relationships, there are also more generalized ones, which explains the simultaneous disruption of interaction in different systems when it is damaged.
A study of children with lesions of the corpus callosum showed a significant difference between “child” and “adult” syndromes. In children aged 5-15 years, symptoms of impaired interaction between the hemispheres were weakly expressed or completely absent, which indicates a late functional formation of the corpus callosum in ontogenesis.
The third type is syndromes of damage to deep hemispheric subcortical structures. The main subcortical structures located deep in the cerebral hemispheres are the basal ganglia. • caudate nucleus (corpus caudatus), • globus pallidus (globus pallidum), • shell (putamen) • fence (claustrum).
In addition to the basal nuclei, other structures also belong to the deep hemispheric subcortical formations (Fig. 60, A, B). The study of the role of these structures in the implementation of HMF is carried out primarily in connection with stereotactic effects on subcortical formations (destruction or irritation) for therapeutic purposes.
The targets of stereotactic influences are different subcortical structures. These include various nuclei of the thalamus (anterior, reticular, ventrolateral, posterior ventral, dorsomedial, midline center, cushion), hypothalamus (posterior, gray tubercle), as well as the hippocampus, amygdala, caudate nucleus, globus pallidus, substantia nigra, Cajal nucleus , cerebellum, etc. Indications for stereotactic effects are mainly hyperkinesis (with parkinsonism and muscular dystrophy) and epileptic conditions.
The most detailed and necessary information about changes in mental processes for neuropsychological analysis was obtained during stereotactic operations on patients with movement disorders (parkinsonism, muscular dystrophy). In this case, the ventrolateral nucleus of the thalamus is affected.
In patients with muscular dystrophy and parkinsonism before surgery, against the background of a relatively intact emotional-personal sphere, visual-spatial gnosis, visual memory, there are disturbances in dynamic praxis, difficulties in carrying out mnestic-intellectual activity associated with disturbances in programming and control. At the same time, they have difficulties in solving visual-figurative problems that require spatial analysis and synthesis. The nature of the syndrome varies depending on the side of the brain lesion: ♦ with left-sided damage to the extrapyramidal system, great difficulties are observed in verbal mnestic-intellectual functions; ♦ with right-sided - difficulties are observed mainly in visual-figurative functions.
Thus, in the subcortical syndromes described above, a violation of three types of factors can be distinguished: 1) a “dynamic” factor associated with the work of the anterior parts of the cerebral hemispheres; 2) “spatial” factor, reflecting the work of the posterior parieto-occipital regions of the brain; 3) “hemispheric” factor, ensuring the functioning of the hemisphere as a whole.
Neuropsychological analysis of lesions of the caudate nucleus established that the nature of the symptoms depends on the localization of the pathological focus: with lesions of the head of the caudate nucleus, distinct motor perseverations were observed; to a lesser extent they were observed in patients with damage to the body of the caudate nucleus. There were also lateral differences in symptoms: a) left-sided lesions caused auditory-speech symptoms (symptoms of alienation of the meaning of words, etc.), disturbances in the assessment of rhythms; b) right-sided - violations of spatial functions and drawing.
Neuropsychological analysis of HMF disorders with damage to deep brain structures showed that in these cases, short-term memory impairments (auditory-verbal or visual-figurative) are common.
They are observed with damage to various subcortical structures: the caudate nucleus, thalamus, cingulate gyrus, hippocampus, and corpus callosum. However, with different lesions they have a different character (in severity, relation to speech or visual-figurative traces, a combination of short-term and long-term memory disorders, the nature of the syndrome as a whole). Other disorders (motor, spatial, emotional, etc.) are less common. Conclusion
The development of the problem of subcortical neuropsychological syndromes from the standpoint of syndromic analysis in domestic neuropsychology is just beginning. Despite certain successes in this area, the creation of a neuropsychological syndromology of damage to subcortical structures is a matter of the future. However, existing data indicate significant differences between subcortical syndromes associated with damage to deep hemispheric structures of the brain and cortical syndromes arising from local lesions of the cerebral cortex: their greater diffuseness, multifactorial nature, a wider “spectrum” of disorders, and different dynamics of recovery.
Rice. Deep structures of the brain (diagram): A - diagram of the frontal section of the brain: 1 - caudate nucleus, 2 - putamen, 3 - globus pallidus, 4 - basal ganglia, 5 - thalamus optic, 6 - superior colliculus, 7 - inferior colliculus , 8 - hypothalamus, 9 - pons, 10 - medulla oblongata, 11 - spinal cord, 12 - reticular formation, 13 - cerebellum, 14 - neocortex; B - diagram of the sagittal size of the brain: 1 - corpus callosum, 2 - fornix, 3 - caudate nucleus, 4 - third ventricle, 5 - internal capsule, 6 - external capsule, 7 - extrema capsule, 8 - optic tract, 9 - base of the pons , 10 - red nucleus, 11 - substantia nigra, 12 - hippocampus, 13 - putamen and globus pallidus, 14 - insula, 15 - optic thalamus, 16 - lateral ventricle (according to V. M. Smirnov et al., 1978)
Stereotaxis is a minimally invasive surgical method, most often used in neurosurgery of the brain. Stereotaxis makes it possible to penetrate into the deep structures of the brain precisely to the designated target through a small burr hole (15mm). The path of movement of the instrument is calculated using a three-dimensional coordinate system in such a way as to eliminate the risk of damage to vital brain structures.
Stereotaxis is used to treat both organic brain lesions: hematomas, tumors, removal of foreign bodies, and functional disorders: Parkinson's disease, epilepsy, indomitable pain and many other diseases. Modern stereotactic systems have a computer planning station capable of determining the coordinates of the brain area that is planned to be affected with an accuracy of 0.6 mm. Such high accuracy is ensured by combining images of the patient’s brain obtained as a result of CT, MRI, EET, radioisotope studies, and comparison with an electronic atlas of the brain. The guides for combining images are markers determined using a stereotactic frame rigidly attached to the patient’s head. After calculating the coordinates of the target, computer programs determine the safest trajectory to reach it.
Stereotactic intervention is performed under local anesthesia, with constant monitoring of the patient’s speech and reactions. A stereotaxic frame attached to the patient's head serves to reference the three-dimensional coordinates of the target, calculated using the planning station. After achieving the goal, it is affected depending on the pathology: for functional disorders, thermal destruction, etc. is used, radioactive sources are introduced into the tumors, hematomas are sucked out, etc. Stereotaxis allows brain surgery to be performed in the least traumatic way, with minimal risk of complications. The need for stereotactic operations in our country is very high; a huge field of activity opens up for neurosurgical departments with a stereotactic system. Stereotaxis is widely used in world medicine; the widespread introduction of this method in our country will bring the level of our healthcare closer to world standards.
Hyperkinesis is automatic violent movements due to involuntary contractions that occur with organic and functional disorders of the nervous system. Hyperkinesis includes athetosis, chorea, shaking paralysis, myoclonus (short muscle flinch with a rapid rate of contraction), etc.
Praxis is the ability to perform a series of learned movements in a certain sequence. Korsakov syndrome is a psychopathological syndrome first described by S.S. Korsakov in 1887. It is characterized by disorders of remembering current events with relative preservation of memories of ancient events and acquired skills. In this case, memory gaps can be filled with events that happened before or could happen. It is observed in Korsakoff psychosis and brain tumors.
Subcortical dysarthria: causes of development
The pathology is often acquired, but dysfunctions caused by congenital pathologies also occur. The prevalence of the disease is the same for men and women and can be found at any age.
The following are the main causes of damage to the extrapyramidal system:
- Injury. With concussions, open craniocerebral injuries, and surgical interventions, damage to subcortical structures can occur, causing dysarthria. In infants, the cause of pathology can be a difficult birth.
- Vascular pathologies. Cerebrovascular accidents have a negative effect on all structures of the brain. With chronic ischemia, there is a gradual deterioration in the functioning of the extrapyramidal system, and with acute ischemic stroke, neurons in the affected area begin to die, which has a direct impact on various structures. As a result of a hemorrhagic stroke, a hematoma is formed, which compresses neighboring tissues.
- Inflammatory diseases (meningitis, encephalitis). Various infectious agents that cause inflammation in the brain provoke changes in the nuclei, basal ganglia and brain tissue. The effects of some diseases, such as measles and rubella, can take several years to appear.
- Neoplasms. Malignant tumors destroy various structures of the brain as they grow. Benign nodes have a negative compressive effect on neighboring tissues.
- Toxic poisoning. Alcohol abuse, overdose of certain medications (antipsychotics, psychoactive substances), carbon monoxide poisoning, and constant exposure to chemicals at work cause dysfunction of brain structures due to toxic poisoning.
- Stress. Chronic stress and psychological tension, mental disorders provoke functional disorders of various brain systems, including the extrapyramidal one.
Material and methods
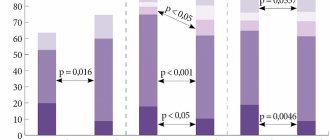
66 patients were examined. Group 1 consisted of 36 men with chronic mercury intoxication (average age - 50.8±6.0 years), with an average work experience in contact with mercury of 14.7±1.05 years. Group 2 included 30 men with chronic alcoholism (average age - 47.5±6.6 years), average duration of alcoholism - 16.7±2.1 years. The control group consisted of 30 apparently healthy men of representative age (average - 47.2±4.7 years) and total work experience (14.2±1.2 years), who had no contact with toxic substances and did not abuse alcohol.
In order to identify the characteristics of CI, a neuropsychological study was used, including a complex of the neuropsychological system according to A.R. Luria; the state of memory was assessed (tests “four is odd”, “broken window”, “performing triple counting”, “performing simple counting operations”, “selection of opposites”, “10 words”, “memorizing groups of pictures when reproduced three times”), praxis ( tests “fist-rib-palm”, Head, Ozeretsky), gnosis (recognition of crossed out, superimposed images, non-speech noises and familiar melodies, showing a given finger according to the pattern and name) and speech (tests for understanding logical-grammatical constructions, ordinal counting from 1 to 10, listing days of the week, months, completing well-known proverbs, repeating sounds, series of sounds, words and phrases) [9]. To diagnose moderately severe cognitive impairment, damage to the frontal lobes or subcortical cerebral structures, the MMSE and FAB tests were used.
The severity of emotional disorders was studied using Zung scales for assessing the asthenic state, personal and reactive anxiety, the level of neuro- and psychopathization, and depression.
Computer electroencephalography (EEG) was performed with the determination of cognitive EPs according to standard methods on a computer multifunctional complex for studying EEG and EPs Neuron-Spectrum-4 (Neurosoft LLC, Russia).
For statistical processing of the study results, an integrated system for complex statistical analysis and data processing, Statistica 6.0, was used. The normality of distribution of quantitative indicators was checked using the Shapiro-Wilk test. To compare quantitative characteristics, the Mann-Whitney test was used; differences were considered statistically significant at p
<0.05. Results were presented as median and interquartile range (25th and 75th percentiles).
In accordance with the requirements of the Committee on Biomedical Ethics, approved by the Declaration of Helsinki of the World Medical Association (2000) and the order of the Ministry of Health of the Russian Federation. No. 266 of June 19, 2003, the examination was carried out with the written informed consent of the patients. The work did not infringe the rights or jeopardize the well-being of the research subjects.
Symptoms of pathology
With subcortical dysarthria, the following main changes occur:
- Violation of muscle tone;
- Distortion of tonic activity (control is lost when the muscles of various oral zones are tense);
- The collapse of friendly movements.
The pathology is characterized by speech disorders such as:
- Difficulty pronouncing words;
- Loss of control over the rate of speech (involuntary speeding up or slowing down);
- Sudden interruption of speech;
- Repetition of certain words or syllables;
- Voice change;
- Loss of control over sound level;
- Slurred articulation;
- Difficulties with intonation;
- Inferiority of phonemic segmentation of words and syllables;
- Hearing loss (in some cases).
Extrapyramidal dysarthria: treatment and prognosis
In the treatment of speech dysfunctions, an important element is eliminating the root cause of the condition. To do this, the patient may be prescribed various studies to visualize brain structures (CT, MRI, EEG). Depending on the underlying cause, appropriate therapy will be formulated if the changes caused by the pathology are reversible. The patient may be prescribed:
- Antibacterial or antiviral treatment in the presence of penetration of an infectious agent;
- Surgery to remove a tumor or eliminate a hematoma;
- Neuroleptics, anti-dementia drugs and other medications to improve the condition of brain tissue and restore blood circulation;
- If drugs are intolerant or there is no expected therapeutic effect from their use, electrical stimulation is an alternative treatment.
An important component of the treatment of dysarthria is speech therapy. Correction of speech dysfunction will normalize articulatory and facial movements, speech breathing, and synchronize facial and respiratory processes.
The prognosis of the disease will depend on the severity and nature of the underlying pathology. With effective implementation of complex treatment and regular sessions with a speech therapist, it is possible to significantly reduce the severity of manifestations of dysarthria. Speech dysfunction is most difficult to treat in cases of malignant neoplasms and progressive dementia.
3. Diagnosis and treatment of gliomas
Until the 70s of the last century, accurate diagnosis of gliomas of the subcortical ganglia and thalamus was practically unattainable, which entailed a high mortality rate of attempts at surgical intervention. Surgeries to remove tumors often led to serious complications and subsequent disability of the patient, and their mortality rate was almost 50% of the number of removals performed. This explains the fact that radiation therapy remained the main method of treatment for a long time.
With the advent of precise neuroimaging techniques - magnetic resonance imaging (MRI) and computed tomography (CT)
Diagnosis of neoplasms has ceased to be particularly difficult, due to which the practice of surgical removal of tumors has significantly expanded.
In addition, this was also facilitated by the emergence of innovative microsurgical techniques
, providing low-traumatic access to the surgical site, as well as improving intensive care (resuscitation) techniques. Today, it is quite possible to remove, for example, nodular tumors of the optic thalamus and thalamic tumors with a low percentage of complications and unfavorable outcomes.
About our clinic Chistye Prudy metro station Medintercom page!
Treatment in Moscow
Successful elimination of subcortical dysarthria is performed by neurologists at the Yusupov Hospital. Doctors use in their work the most effective methods for correcting speech dysfunction while eliminating the root cause of the pathological condition. Neurologists at the Yusupov Hospital have extensive experience in treating neurological diseases and are constantly improving their level of qualifications by studying the latest research in this area and exchanging experience with foreign and domestic colleagues.
The Yusupov Hospital is equipped with the latest technology, which allows it to perform diagnostics of varying complexity to make the most accurate diagnosis. This is an important condition for developing the most adequate and effective therapy.
In addition to neurologists and speech therapists, patients at the Yusupov Hospital can use the services of a psychologist. This will help you get rid of the psychological discomfort and depression that often arise as a result of dysarthria, as well as gain additional motivation to overcome the disease.
To make an appointment at the Yusupov Hospital, you can call by phone.