Mechanical damage to the human skull along with its contents, which is manifested by established neurological symptoms, is called traumatic brain injury. Timely first aid for traumatic brain injuries helps save the life and many functions of the victim’s body, so it is extremely important to know all the basics of behavior in such a situation.
Main causes and types of injuries in the skull area
The pathologies under study can arise as a result of many factors, for example, during road traffic accidents, human falls from a height, at work and at home, during active sports.
Content:
- Main causes and types of injuries in the skull area
- Clinical course of the pathology
- First aid
The main types of traumatic brain injuries include closed, open and penetrating injuries to the head. The closed type of such injuries include those in which the aponeurosis remains without damage, but there are injuries or bruises to the head in the soft tissue section. Open craniocerebral injuries are characterized by damage to the aponeurosis and integrity of the skin on the head. Experts consider penetrating injuries to be those that result in disruption of the integrity of the dura mater of the brain.
Brain contusion
Compared to a concussion, a brain contusion is a more serious injury that requires urgent treatment. With this type of TBI, small vessels of the brain are affected, hemorrhage occurs, and cerebrospinal fluid (cerebrospinal fluid) may leak.
The injury may be accompanied by compression of soft tissues or occur without it. The method of treating a brain contusion depends on this.
The main symptoms of a brain contusion without compression :
- loss of consciousness (or coma);
- frequent vomiting;
- tachycardia and arrhythmia;
- decreased muscle function in the arms and legs (paresis) and loss of coordination;
- high blood pressure;
- the appearance of blood in the cerebrospinal fluid;
- prolonged severe headaches;
- vestibular dysfunction;
- loss of memory for immediate events.
Compression of the brain may occur during the head injury itself or some time later as a result of the occurrence of an intracranial hematoma.
Hematomas can be acute, subacute and chronic. If in the first case the patient’s condition begins to rapidly deteriorate, then with subacute and chronic hematoma the inflammatory process can last for months.
When the brain is compressed by a hematoma, the following clinical signs :
- convulsions;
- increased intracranial pressure;
- the appearance of delusions and hallucinations;
- weakening of abdominal and tendon reflexes;
- paresis or paralysis of the limbs;
- damage to the optic nerves.
Clinical course of the pathology
More often than others, with traumatic brain injuries, a concussion occurs without macrostructural lesions. Brain damage at the cellular level is reversible and treatable. The main symptoms of a concussion are loss of consciousness for a short time, nausea and vomiting, dizziness, headaches, double vision, sweating, memory loss. From a neurological point of view, there is a violation of symmetry in tendon reflexes, small-scale nystagmus, which under normal conditions disappears a week after the injury. If the victim undergoes a computer or magnetic resonance imaging scan, they will not reveal any pathologies.
With traumatic brain injuries, brain contusion can occur. This pathology leads to hemorrhages and destruction (gross macrostructural disorders) in the brain, accompanied by subarachnoid hemorrhage. Often a brain contusion is accompanied by a fracture of the skull bones. All this together can lead to swelling of the brain.
Manifestations of brain contusion by severity:
- Mild degree - the patient’s loss of consciousness can last up to 20 minutes, after which dizziness, vomiting and nausea, headaches, anterograde or retrograde amnesia occur. Vital functions remain unchanged; cardiovascular changes in the form of hypertension or bradycardia may occur. Neurological symptoms include pyramidal insufficiency, clonic nystagmus, and slight anisocoria.
- In the middle stage, the patient’s unconscious state lasts for several hours, after which severe memory loss occurs, repeated vomiting occurs, and mental health is impaired. Vital functions are impaired, persistent bradycardia, tachypnea with preservation of airway patency, hypertension. From a neurological point of view, nystagmus, imbalance in tendon reflexes and muscle tone, and various meningeal signs are observed. Focal manifestations in the form of ocular and pupillary disorders, changes in speech, and paresis of the limbs are also obvious.
- In severe cases, the patient falls into a coma, which, if not fatal, can last several weeks. Severe violations of vital functions pose a threat to life. The movements of the eyeballs are floating, the rhythm and frequency of breathing are disturbed, bilateral miosis or mydriasis, and convulsions occur. With such traumatic brain injuries, there are fractures of the skull bones in combination with massive subarachnoid hemorrhage.
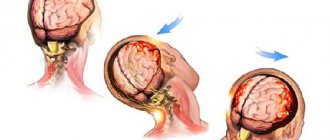
Compression of the brain substance may occur due to intracranial hematomas that form above or below the soft membrane.
Clinically, compression can manifest itself in the same way as a bruise, but it has a very dangerous consequence. After the victim returns to consciousness, he usually feels better, but this does not last long, until the intracranial hematoma grows in size and begins to compress the brain. After this, the person falls into a coma again, and the prognosis for this state is rarely satisfactory. The functioning of the respiratory and vascular centers is disrupted.
According to severity they are distinguished:
- Mild TBI: characterized by a concussion and mild brain contusion;
- Moderate TBI: characterized by moderate brain contusion; In this case, the following are possible: fracture of the vault and base of the skull, traumatic subarachnoid hemorrhage, epileptic seizures;
- Severe TBI: characterized by severe brain contusion, brain compression, severe axonal damage to the brain; Possible fractures of the vault and base of the skull, epileptic seizures, severe brainstem and diencephalic disorders.
There are several main types of interrelated pathological processes:
- direct damage to the brain substance at the time of injury;
- cerebrovascular accident;
- violation of liquor dynamics;
- disorders of neurodynamic processes;
- formation of scar-adhesive processes;
- autoneurosensitization processes.
The basis of the pathological picture of isolated brain injuries is primary traumatic dystrophies and necrosis; circulatory disorders and organization of tissue defect. Concussions are characterized by a complex of interconnected destructive, reactive and compensatory-adaptive processes occurring at the ultrastructural level in the synaptic apparatus, neurons, and cells.
Brain contusion is an injury characterized by the presence in the substance of the brain and in its membranes of macroscopically visible foci of destruction and hemorrhage, in some cases accompanied by damage to the bones of the vault and base of the skull. Direct damage to the hypothalamic-pituitary, brainstem structures and their neurotransmitter systems during TBI determines the uniqueness of the stress response. Impaired metabolism of neurotransmitters is the most important feature of the pathogenesis of TBI. Cerebral circulation is highly sensitive to mechanical influences.
The main changes that develop in the vascular system are expressed by spasm or dilation of blood vessels, as well as increased permeability of the vascular wall. Directly related to the vascular factor is another pathogenetic mechanism for the formation of the consequences of TBI—a violation of liquor dynamics. Changes in the production of cerebrospinal fluid and its resorption as a result of TBI are associated with damage to the endothelium of the choroid plexuses of the ventricles, secondary disorders of the microvasculature of the brain, fibrosis of the meninges, and in some cases, liquorrhea. These disorders lead to the development of liquor hypertension, and less commonly, hypotension.
In TBI, hypoxic and dysmetabolic disorders play a significant role in the pathogenesis of morphological disorders, along with direct damage to nerve elements. TBI, especially severe, causes respiratory and circulatory disorders, which aggravates existing cerebral dyscirculatory disorders and collectively leads to more pronounced brain hypoxia.
Currently (L. B. Likhterman, 1990) there are three basic periods during traumatic brain disease: acute, intermediate, and remote.
The acute period is determined by the interaction of the traumatic substrate, damage reactions and defense reactions, and is the period of time from the moment of the damaging effects of mechanical energy until the stabilization at one or another level of impaired cerebral and general body functions or the death of the victim. Its duration ranges from 2 to 10 weeks, depending on the clinical form of TBI.
The intermediate period is characterized by the resorption and organization of areas of damage, and the development of compensatory and adaptive processes until complete or partial restoration or stable compensation of impaired functions. The length of the intermediate period for non-severe TBI is up to 6 months, for severe TBI – up to a year.
The long-term period is the completion or coexistence of degenerative and reparative processes. The length of the period for clinical recovery is up to 2–3 years, for a progressive course it is not limited.
Complications
Violations of vital functions - a disorder of the basic life support functions (external respiration and gas exchange, systemic and regional circulation). In the acute period of TBI, the causes of acute respiratory failure (ARF) are dominated by pulmonary ventilation disorders associated with impaired airway patency caused by the accumulation of secretions and vomit in the nasopharynx with their subsequent aspiration into the trachea and bronchi, and retraction of the tongue in comatose patients.
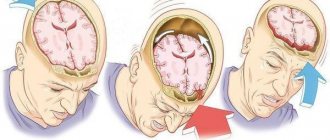
Dislocation process: temporotentorial inclusion, representing a displacement of the mediobasal sections of the temporal lobe (hippocampus) into the fissure of the tentorium of the cerebellum and herniation of the cerebellar tonsils into the foramen magnum, characterized by compression of the bulbar sections of the trunk.
Purulent-inflammatory complications are divided into intracranial (meningitis, encephalitis and brain abscess) and extracranial (pneumonia). Hemorrhagic - intracranial hematomas, cerebral infarctions.
There are five gradations of the condition of patients with TBI
Satisfactory condition. Criteria:
- clear consciousness;
- absence of violations of vital functions;
- absence of secondary (dislocation) neurological symptoms; absence or mild severity of primary focal symptoms.
There is no threat to life (with adequate treatment); the prognosis for recovery is usually good.
Moderate condition. Criteria:
- state of consciousness - clear or moderate stupor;
- vital functions are not impaired (only bradycardia is possible);
- focal symptoms - one or another hemispheric and craniobasal symptoms may be expressed, often appearing selectively.
The threat to life (with adequate treatment) is insignificant. The prognosis for restoration of working capacity is often favorable.
Serious condition. Criteria:
- state of consciousness - deep stupor or stupor;
- vital functions are impaired, mostly moderately according to 1–2 indicators;
- focal symptoms:
- stem - moderately expressed (anisocoria, decreased pupillary reactions, limited upward gaze, homolateral pyramidal insufficiency, dissociation of meningeal symptoms along the body axis, etc.);
- hemispheric and craniobasal - clearly expressed both in the form of symptoms of irritation (epileptic seizures) and loss (motor disorders can reach the degree of plegia).
The threat to life is significant and largely depends on the duration of the serious condition. The prognosis for restoration of working capacity is sometimes unfavorable.
Extremely serious condition. Criteria:
- state of consciousness - coma;
- vital functions - gross violations in several parameters;
- focal symptoms: stem - expressed roughly (plegia of upward gaze, severe anisocoria, divergence of the eyes along the vertical or horizontal axis, a sharp weakening of the pupils' reactions to light, bilateral pathological signs, hormetonia, etc.); hemispheric and craniobasal - pronounced.
The threat to life is maximum and largely depends on the duration of the extremely serious condition. The prognosis for restoration of working capacity is often unfavorable.
Terminal state. Criteria:
- state of consciousness - terminal coma;
- vital functions - critical impairment;
- focal symptoms:
- stem - bilateral fixed mydriasis, absence of pupillary and corneal reflexes;
- hemispheric and craniobasal - blocked by general cerebral and brainstem disorders.
Survival is usually impossible.