Pain localized in the back and lower back is a fairly common unpleasant symptom that accompanies a person. Sometimes such pains tend to echo, as if in adjacent areas of the body - primarily the legs. Pain radiating to the leg is radiating (false) pain, which does not arise due to a true injury to the leg, but because the impulses coming from the receptors to the brain are mixed. Thus, radiating pain is transmitted to that part of the body that has a single nerve supply system with the truly affected organ.
Pain radiating to the leg can be associated with both classic problems such as excessive physical exertion or prolonged stay in one position, and with more serious ones - pinched nerves, circulatory disorders, diseases of internal organs. It is also difficult to understand the true cause of pain because its nature and localization are not unambiguous - the pain can be more pronounced both in the leg and in the lower back, sometimes weak, sometimes growing, aching, shooting or sharp.
Contacting a qualified doctor is the first step after the appearance of any unpleasant painful sensations in the leg. It is impossible to independently determine the cause of pain, which means it is unacceptable to choose methods for getting rid of it yourself. The main task is to cure the root cause that causes pain radiating to the leg. Only a specialist can solve it by making the correct diagnosis based on professional diagnostic methods.
Possible causes of pain radiating to the leg
Most often, the cause of radiating pain in the leg is orthopedic diseases or neurological disorders. The first group includes:
- osteochondrosis;
- hernia;
- spondylosis;
- osteoporosis;
- osteomyelitis;
- prolapse;
- spinal column deformity (scoliosis).
To the second:
- damage to the lumbar roots;
- pinching;
- benign neoplasms;
- inflammation of the sciatic nerve.
- Other causes of pain radiating to the leg include:
- nagging or shooting pain down to the toes;
- diseases of internal organs;
- spinal and lumbar injuries.
Treatment methods
If the cause of paresthesia is a certain disease, then it can only be eliminated simultaneously with the elimination of the cause of this disease. The course of treatment is prescribed by a specialist only after an examination. Recommendations may include physiotherapy procedures, medications and even traditional medicine.
Physiotherapeutic procedures include the following: electrophoresis, massage, paraffin baths, physical therapy, magnetic therapy and electrical stimulation.
During treatment, special drug therapy is used to restore damaged blood flow.
If there is a hernia or varicose veins, special surgical treatment is used. Also, to improve the passage of nerve impulses, it is recommended to take multivitamin preparations of group B.
Special contrast baths also help relieve muscle tension. To do this, first dip your feet in cold water, and then in hot water. You can do this every day, holding your feet under water for 30 seconds.
Related symptoms
The pain can affect either one lower limb or both. Often a person experiences the following symptoms associated with this pain:
- heaviness in the legs;
- lower back pain;
- feeling of a “lumbago” in the back, lower back or legs;
- inability to bend the leg;
- irritability, unusual mood swings, increased fatigue, insomnia. This may be directly related to discomfort from pain, or it may be a signal of problems with neurology.
Symptoms
If the legs go numb infrequently and this condition goes away quickly, then such patients do not need to worry about anything. However, there are people who experience long-term effects of paresthesia symptoms. This causes them great discomfort in everyday life and forces them to seek medical help. Such cases always require a special examination, which will accurately help identify the cause of such a pathological condition. A person should pay close attention to their condition if they have the following symptoms:
- blue skin around the numb finger;
- pain with prolonged loss of sensation;
- spread of numbness to the entire leg;
- feeling of numbness in the leg throughout the day;
- swelling and redness in the damaged area;
- significant changes in the nature of gait.
An integrated approach to the diagnosis of pain in medical
Pain radiating to the leg is an alarming condition that requires the supervision of an experienced medical professional. In our clinic, doctors approach the issue of diagnosis comprehensively and comprehensively. A number of different diagnostic tests and procedures are involved:
- radiography of the lumbosacral spine;
- MRI of the lumbosacral spine;
- USAS of the veins of the lower extremities;
- Ultrasound of the abdominal organs;
- bone scan (densitometry);
- general blood and urine tests.
All studies are carried out using high-precision equipment from leading medical brands. A competent diagnosis is the key to finding the true cause of the pain radiating to the leg. Based on the results of checking the condition of the body, the doctor will make a diagnosis and prescribe appropriate treatment.
If you are concerned about pain in your legs and any restrictions in your body mobility, make an appointment with us without expecting the condition to worsen. The sooner you start treating the underlying disease, the less likely it is to relapse and develop complications.
Preventive actions
If the patient complains of numbness in the fingers, the doctor can recommend effective preventive measures.
Usually, numbness itself is not a very dangerous symptom, but if you do not find out the cause of its occurrence in time, then serious difficulties may arise in the future. To prevent this from happening you should:
Only a complete examination can give the doctor a picture of what is happening with the patient and allow him to prescribe quality treatment. This treatment will be aimed not only at relieving symptoms, but also at eliminating the root cause of the disease.
Thus, there are many reasons for the symptoms of numbness in the big toes. Among them there are both conditionally harmless ones and those that can signal the onset of serious health problems. The second type requires mandatory medical intervention. That is why, when they appear, you should not put off going to the doctor for too long.
Peripheral nervous system injury
Traumatic injuries to peripheral nerves, plexuses, spinal nerves, nodes and roots can occur due to mechanical impact on nerve structures, which especially often occurs in domestic, industrial and transport injuries. In this case, concussion, bruise, sprain, compression, crushing, and rupture of the structures of the peripheral nervous system may occur.
- Classification
In accordance with the classification of the World Health Organization (WHO, 1982), PNS injuries are divided according to the following criteria:
- According to the form of damage:
- Break
- Defrosting
- Compression
- Compression with rupture
- According to the state of the macroscopic (external) picture:
- Complete interruption of the peripheral nerve
- Partial interruption of the peripheral nerve
- Intrastem neuroma
- Swelling at the level of the nerve without interruption
- Nerve damage without visual changes in the nerve trunk
- According to the microscopic picture
- Neuropraxia - the continuity of the nerve fibers is preserved, but their function is impaired. The prognosis is favorable
- Axonotmesis - there is a break in the axons with subsequent Wallerian degeneration of fibers distal to the site of their damage, while the connective tissue structures of the nerve (sheaths) are preserved. It manifests itself as motor, sensory and autonomic disorders in the area innervated by the damaged nerve. Regeneration is possible.
- Neurotmesis is a rupture of a nerve. It manifests itself as peripheral paralysis, anesthesia, and severe vegetative-trophic disorders. It is possible for a nerve neuroma to form at the site of the break, which makes independent restoration of the nerve structure impossible. A neuroma is a tangle of motor nerve processes that regenerate from a segment of nerve above the break point. Restoration of nerve function in this case is long and not always complete.
- Clinical picture:
The following periods of PNS injury are distinguished:
- Acute period (3 weeks), it is often difficult to reliably assess the degree of nerve dysfunction and prognosis
- Early period (3 weeks -3 months), during this period it is possible to fully assess the true extent of the lesion and the prognosis;
- Subacute period (3-6 months)
- Late period – slow nerve regeneration;
- Remote period
In the acute period of nerve injury, the main symptoms are:
- Pain syndrome at the site of innervation of the affected nerve.
- Lack of sensitivity or discomfort (paresthesia) at the site of innervation of the affected nerve.
- Weakness (paresis) of the muscles supplied by the affected nerve.
- Autonomic disorders in the area of innervation of the affected nerve (swelling, cyanosis, marbling of the skin, excessive sweating or dry skin).
After some time has passed after the injury, the following symptoms may develop:
- in the presence of motor disturbances in the limb, its immobility - joint contractures;
- worsening of autonomic disorders, atrophy of the skin and subcutaneous tissue, the appearance of trophic ulcers.
- Causalgia is a painful, burning, difficult-to-localize pain, which is partly explained by the fact that first the thin, soft nerve fibers that are responsible for conducting pain impulses are restored.
- Phantom pain, phantom sensations are a false sensation of the presence of an amputated limb, which may indicate the formation of a neuroma and the need for surgical treatment.
- Required examination:
To assess the nature and extent of peripheral nerve damage, the patient must:
General examination + examination by a neurologist;
ENMG (electroneuromyographic study) to determine nerve function;
According to indications, ultrasound of the nerve trunk, plexus, and MRI of the nerve plexus are performed.
- Treatment:
In the acute period, immobilization of the injured limb is necessary.
If there is an open wound, it is necessary to consult a neurosurgeon, surgical treatment of the wound with revision of the condition of the nerve, and, if necessary, suturing the nerve.
Drug therapy: B vitamins, decongestant therapy, drugs that improve the rheological properties of blood, drugs that improve microcirculation, neuroprotectors. In the presence of intense pain syndrome, adequate pain relief is required, often with the use of drugs from the group of anticonvulsants and antidepressants.
Physiotherapeutic methods of treatment play a significant role - electro- and phonophoresis with euphyillin and proserin.
In the absence of contraindications, physical therapy, IRT, and massage are used.
Numbness: limbs, finger, arm, leg go numb
Causes of numbness
Numbness is a sensation that typically occurs in certain areas of the skin. The most common accompaniments of numbness are tingling, chilliness, burning and tightening. Such symptoms, for the most part, turn out to be signs of such diseases:
- migraine;
- osteochondrosis;
- the presence of intervertebral hernias;
- poor circulation in the arm or leg area;
- diabetes;
- are signs of deficiency of vitamins, microelements and excessive consumption of alcoholic beverages;
- transient ischemic attacks, which involve one arm or one leg, one or another part of the body, or maybe all limbs;
- compression of the nerve in the narrow areas where it passes, in the areas of the wrist, elbow, groin, ankles, tunnel syndromes are formed;
- nerve damage as a result of joint deformation. These are rheumatoid arthritis and other diseases;
- multiple sclerosis;
- some hereditary diseases that are associated with nerve damage.
People who experience attacks of numbness often wonder what to do: see a doctor or wait until the symptoms go away on their own. In fact, if attacks of numbness occur quite often, a visit to a doctor is mandatory. Moreover, if, in addition to numbness, there is pain, awkwardness, weakness, or loss of sensitivity, and also if, with numbness, there is a lack of coordination of movements. In addition, a visit to a neurologist is mandatory if you cannot distinguish cold water from warm water.
Numbness of the limbs (numbness of the limbs)
Numbness of the limbs is a very unpleasant sensation that occurs when a nerve is pressed for a short time, when a person assumes an uncomfortable position for a while. When you change position, the numbness goes away within a few minutes. But if changing posture does not help get rid of this feeling, and it occurs quite often, this should be taken as a signal that you should consult a doctor.
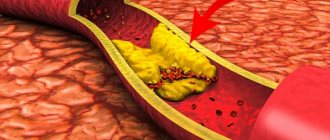
Numbness in the extremities may indicate the presence of arterial vascular disease (most often in the legs). This disease can cause inflammation of the inner lining of blood vessels, the formation of obstruction in the arteries (Raynaud's disease, atherosclerosis obliterans, stroke), and impaired blood circulation. This may result in partial gangrene of the limb. Numbness of the limbs can occur due to nerve injury, which is caused by diseases such as tunnel neuropathy, osteochondrosis, carpal tunnel syndrome.
Numbness of the hands is a very common disease. Its cause is compression of the nerves supplying blood to the median nerve. If this disease is not treated in a timely manner, its consequences can be very negative. First, the disease manifests itself in numbness of the fingers, then the palms, arms, over time, it can turn into pain that occurs at night, then it can appear in the morning. Later, the pain appears during the day, and especially intensifies when you raise your arms up.
Numbness of the limbs may be due to the following reasons:
- Uncomfortable posture when lying and sitting. In such situations, after numbness, a tingling sensation occurs, which goes away when you change position;
- pinched nerve caused by spinal problems, for example, osteochondrosis;
- due to carpal tunnel syndrome. In this case, the first, second and third fingers of the hand usually go numb, as compression occurs on the middle nerve passing in the area of the hand.
Often the cause of this disease is prolonged use of a computer mouse. First, the fingers become numb, followed by a tingling sensation that turns into severe pain;
- lack of vitamin B12 in the body. This vitamin is included in the metabolic processes of nerve fibers and its low content in the body causes not only fatigue and general weakness, but also leads to impaired sensitivity, heart rhythm disturbances and irritability;
- Raynaud's disease. This disease manifests itself as paroxysmal circulatory disorders of the arteries, which most often appear in the area of the feet and hands. The occurrence of the disease can be caused by stress, hereditary factors (consisting of structural features of the nervous system), intoxication (nicotine and alcohol).
Young women who have suffered from hypothermia, infectious diseases, overwork or prolonged exposure to sunlight are most susceptible to this disease. In addition, young women who work a lot with the computer, as well as pianists, are at risk. With Raynaud's disease, not only numbness is felt, but also rapid freezing, as well as the acquisition of a blue tint to the fingers in the cold and during excitement. Most often, the disease affects the second, third and fourth fingers and toes.
If such symptoms are not given proper attention and are not treated, the disease can also affect other organs (chin, ears, nose). The arms are affected first, and later the legs;
- obliterating endarteritis. This disease affects arterial vessels (most often of the lower extremities). Due to significant vasoconstriction, blood circulation is disrupted, accompanied by a feeling of numbness, as well as cooling of the extremities. A progressive disease leads to complete blockage of blood vessels, resulting in gangrene;
- neuropathy. This disease affects the nerves. It is caused by metabolic disorders or intoxication. Symptoms characteristic of this disease are: itching, tingling, burning, tightening sensations in the toes and hands, and on the protruding parts of the foot. Patients often describe their sensations as “numbness.” There is a manifestation of spontaneous pain. Neuropathy is also characteristic of diseases such as rheumatoid arthritis, diabetes mellitus, multiple sclerosis, and so on;
- ischemic stroke of the vertebral and inferior cerebellar arteries. Often numbness of the limbs accompanies this disease;
- There are cases when numbness of the limbs occurs due to hyperventilation, accompanied by rapid and shallow breathing in a state of anxiety or fear.
Numbness of the limbs is a symptom caused by bending of nerve bundles or blood vessels, uncomfortable body position, impaired blood circulation, or more dangerous diseases that were described above. Numbness is a change in the sensory function of the limbs, often accompanied by painful sensations and tingling sensations.
The consequences of numbness of the extremities can vary significantly: from blood circulation disorders and up to gangrene of the extremities (partial). These consequences depend on what caused the numbness. However, regardless of the reasons, if numbness occurs frequently, this means that the functioning of blood circulation and blood vessels in the extremities is impaired. This implies that there is a risk of dangerous diseases and you should consult a doctor in order to diagnose the disease in time and prevent its development.
Numbness of hands (hands go numb)
The most common reason for numbness in the hands is considered to be compression of the neurovascular bundle by connective tissue, as well as muscles. This bundle provides nutrition and innervation to the muscles. There are seven places where compression can occur. After conducting a diagnosis, the doctor can identify the affected area and eliminate compression of the vessel or nerve. In cases where numbness of the limbs is associated with disorders in the functions of the spine, the doctor will also determine the location of the lesion and take action to eliminate it.
Numbness of the fingers (numbness in the fingers)
Numbness of the fingers, or carpal tunnel syndrome, was not common until the 1980s and was almost unheard of. However, from that time on, the number of people using computers began to increase rapidly. Daily use of a computer keyboard is a significant risk factor in the development of this syndrome. But not only people associated with computers are at risk for this disease; it also includes carpenters, painters, seamstresses, that is, those people who have to make the same type of hand movements every day. In practice, carpal tunnel syndrome occurs when, after straining, the tendons swell, thereby compressing the nerve responsible for sensation in the palm, middle, index and thumb. The nerve and tendons pass through the same fairly narrow canal. This compression of the nerve due to swelling of the tendon leads to tingling, numbness, and throbbing pain localized in the fingers. Pain and other symptoms of this syndrome are often felt more strongly at night or in the morning. Lack of timely treatment can cause death of the muscle responsible for the movement of the thumb. As a result, a person will not be able to bend his thumb, as well as clench his hand into a fist. A large number of people, in such a situation, have to change their profession. Statistics show that women are more susceptible to carpal tunnel syndrome. The most common age at which the disease occurs is 40-60 years.
Numbness of the legs (feet go numb)
Numbness in the legs is a very common symptom in people of working age. This manifestation of the disease causes a large number of inconveniences and concerns. In this case, the concern is not unfounded, since impaired nervous sensitivity is a sign of a serious illness. According to statistics, 90 percent of leg numbness is caused by spinal problems: intervertebral hernias, osteochondrosis, and so on.
The spine is responsible for many functions in our body. The normal functioning of the legs and arms is also the responsibility of the spine. Pain in the legs may occur as a result of changes in the lumbar spine. The frequency and nature of numbness may vary, depending on the reasons for which they arose. Intervertebral hernias can compress the nerve roots, thereby causing a reflex spasm of the tissues, as a result, patients have numb legs, a feeling of “cottonness”, pain, a feeling of “crawling goosebumps”, prolonged standing, sitting, tilting the head, coughing, and so on lead to increased pain. Less commonly, the occurrence of numbness is caused by osteochondrosis or other systemic diseases (for example, diabetes mellitus).
Osteochondrosis is a disease that progresses over a long period of time and can be accompanied by various clinical manifestations. To determine the causes of numbness in the legs, additional examinations often need to be performed. In order to clarify the diagnosis, an X-ray of the spine, namely its lumbar region, is used, MRI and ultrasound are used.
In order to establish the cause of numbness in the legs, additional research methods are often required. To clarify the diagnosis, MRI, X-ray of the lumbar spine, and ultrasound are used.
Usually, before numbness in the legs occurs, the patient experiences other symptoms of diseases associated with the spine, such symptoms can appear as early as the age of twenty and be in the nature of chronic lower back pain. If medical care is not provided on time, the disease will continue to progress, despite the fact that the pain goes away over time, leaving behind a feeling of stiffness in the spine, and then various pains in the legs appear.
If the cause of numbness turns out to be radiculitis, hernia, osteochondrosis (in 95% of cases), then timely assistance from a specialist who can find out the causes of the disease, as well as take all measures to prevent its development, is very important. Our clinic offers highly accurate diagnosis of diseases, as well as their effective treatment.
Numbness of the toes (numb toes)
There are many reasons that cause numbness in the toes. For example, various metabolic disorders, such as radiculoneuritis, can lead to numbness in the legs. Similar reasons also include spinal osteochondrosis, accompanied by narrowing of the intervertebral spaces, vascular disorders, spinal tuberculosis, and sometimes the development of cancer.
Oncological diseases lead to numbness of the fingers due to the growth of a tumor outside or inside the spinal cord, creating pressure, which in turn causes numbness. This process does not carry the danger that a person will not be able to walk. However, if the numbness is caused by the development of a tumor in the legs, then the risk that the person will quickly develop disability is very high.
If numbness is caused by osteochondrosis, loss of the ability to walk can occur either quite quickly or develop slowly - it all depends on the degree of damage to the spine.
Obviously, if you experience numbness in your legs, you should immediately consult a doctor. The doctor must conduct all the necessary examinations and, only after that, make a diagnosis. It is impossible to make a diagnosis based solely on the patient’s complaints.
It is impossible to delay contacting a specialist, since it is a well-known fact that the earlier treatment is started, the more effective and faster it will be.