The prevalence of lesions of the nervous system (CNS) in newborns has recently become almost epidemic. More and more children under one year of age are turning to pediatric neurologists and pediatricians with complaints of hyperactivity and developmental delay, which are nothing more than the consequences of pathology suffered during childbirth.
Many diseases of older children occur due to the fact that damage to the nervous system during the neonatal period was not recognized in time. In 80-85% of dead newborns, the section reveals a spinal cord injury; brain injuries are 2 times less common.
The consequences of damage to the nervous system during childbirth can be hydrocephalus, developmental delay, paresis and paralysis, visual and hearing impairment.
Causes of central nervous system damage in newborns
Suppression of the central nervous system of a newborn during and after childbirth can occur for three main groups of reasons: ischemic-hypoxic lesions, traumatic and infectious-toxic. Let's look at each group in more detail.
- Ischemic and hypoxic lesions of the central nervous system in newborns
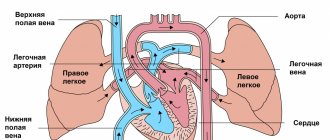
are caused by a lack of oxygen in the child’s blood during childbirth. This may be due to long and protracted labor, weakness of labor, abnormalities of the placenta and umbilical cord. With ischemia (complete absence of oxygen), brain cells die, and the further picture of the disease depends on which part of the cortex this happens. - Traumatic lesions of the central nervous system
- in the vast majority of cases occur during childbirth. The immediate cause may be an early birth (the baby’s head is born very quickly and is injured), a large fetus, unskilled actions of the obstetrician, etc. - Infectious and toxic lesions
can be associated with viral infection, alcohol, smoking during pregnancy, etc.
Brain lesions most often have an ischemic-hypoxic nature, while the spinal cord is more often affected by physical trauma to the child’s neck during childbirth. To prevent this, it is very important to give birth in a good maternity hospital with a competent obstetrician, and in the first days after discharge, go to see an osteopath.
Main complaints
Pathology of the nervous system in newborns does not appear immediately, and this is its insidiousness. After all, the longer the disease remains unrecognized, the more difficult it is to treat it in the future. Only very pronounced disorders make themselves felt in the first days of the baby’s life, usually manifesting themselves in convulsions. Seizures that occur in the first 24 hours after the baby is born are especially dangerous.
Most often, parents pay attention to the child’s hyperexcitability, restless behavior, and sleep disturbances. Also often associated symptoms are excessive regurgitation and choking. Some mothers manage to notice disturbances in motor functions. As a simple home test, you can use a child's skills screening test depending on age.
Screening test. Normal full-term baby:
- By 2 months he can hold his head while lying on his stomach.
- By 6 months, sits independently and steadily.
- At 12 months – the beginning of independent walking.
Children with traumatic lesions of the spinal cord at the neck level are delayed by 1-2 months, however, their developmental delay is not as severe as with damage to the cerebral cortex.
Based on the pace at which the child develops, one can approximately judge the presence of neurological abnormalities and consult a doctor in time. The doctor will conduct more detailed studies that will show the diagnosis and level of damage to the nervous system.
The main types of neurological pathology in children of the first year of life
To identify diseases of the nervous system, manifested by a specific delay in psychomotor development, it is important to assess the neurological and psychopathological signs accompanying the developmental delay. The age-related immaturity of the nervous system of a child in the first year of life determines the fragmentation and undifferentiation of the signs observed in him. The body, especially a newborn and infant, reacts to various hazards with a limited number of typical reactions, the nature of which primarily depends on the age phase of neuropsychic development. Below are the main options, reflecting mainly the type of neuropsychic reaction in the first year of life.
- GENERAL INSPECTION OF A NEWBORN - WHAT PARENTS SHOULD PAY ATTENTION TO
- PERINATAL BRAIN DEPRESSION (NERVOUS HYPOEXCITABILITY)
- PERINATAL BRAIN HYPEREXCITABILITY
- INTRACRANIAL PRESSURE REGULATION DISORDER (HYPERTENSION-HYDROCEPHAL SYNDROME)
- CONVIVUS SYNDROME
- CEREBRASTHENIC SYNDROME
- MOVEMENT DISORDER SYNDROMES (MUSCULAR DYSTONIA, Cerebral Palsy)
General examination of a newborn - what parents should pay attention to
Considering the high incidence of perinatal pathology of the nervous system and the possible difficulties of obtaining qualified specialized care, there is no doubt that there is an urgent need for parents to receive relevant popular scientific information.
What can we see for ourselves? - General examination of the newborn The child normally breathes rhythmically, makes automatic movements of the limbs in sufficient volume and symmetrically. The slightest restrictions in movement in the arms or legs should be the basis for a targeted study - are there any movement disorders? The nature and volume of the baby's crying is important. The posture of a newborn can tell a lot. In some cases, the child is lethargic, inactive, and sometimes literally lying flat. In other cases, on the contrary, the tone in the limbs is evenly increased - when swaddling, the peculiar stiffness of the limbs immediately attracts attention. It is very important not to miss even small convulsive twitches during examination.
Examination of a newborn's head reveals a lot. A birth tumor is typical for most newborns. The larger the size of this tumor, the more difficult the birth of the child was, and such a child should be the subject of a particularly careful examination. Some children notice bruises on the face, neck, and torso as a result of a traumatic birth - in these cases, neurological symptoms are also more often detected. Head deformations (the so-called “configuration”) almost always indicate a birth injury to the skull, and among these children craniocerebral symptoms are much more common, which is understandable and easily explainable. In everyday practice, cephalohematoma is sometimes underestimated, usually only because it is “common” and “located outside the skull.” Indeed, we are talking about a subperiosteal hematoma, sometimes quite significant in size. It is indeed common, but this cannot serve as an argument against it - it is an injury, and what is important for the diagnosis is not even the cephalohematoma itself, but what it indicates - at the level of such a hematoma, there are undoubtedly areas of microhemorrhages in the underlying areas of the brain , which, regardless of the patient’s age, indicate cerebral contusion. One of the important indicators of difficulties with childbirth is such a sign as the location of the skull bones on top of each other. This small dislocation usually does not lead to damage to the underlying brain tissue, but it certainly indicates that the fetal skull passed through the birth canal, experiencing great resistance - in these cases, signs of damage to the nervous system are often revealed.
The condition of the fontanelles plays a major role in assessing the child’s condition: tension and bulging of the fontanelles is a very serious symptom of increased intracranial pressure. The size of a newborn's head tells the doctor a lot: signs of hydrocephalus, if detected from the first days of life, usually indicate intrauterine brain pathology, while the gradual development of hydrocephalus can often be a consequence of birth damage to the brain.
Here it should be noted the catastrophic frequency of the unjustifiably expanded diagnosis of “hypertensive-hydrocephalic syndrome”, which in many hospitals and clinics is made with or without reason. The worst thing is that in such cases, massive and long-term therapy with diacarb immediately begins, which is not only unjustified, but exhausting for the child.
In some newborns, the head is smaller than normal, and the brain part of the skull is smaller than the facial part - sometimes this indicates intrauterine and genetic pathology (microcephaly) and, unfortunately, has serious consequences. Recently, more and more often there are children with very early closure of the fontanelle, while the growth rate of the head in such newborns clearly lags behind the norm.
The sign of a “short neck” is quite common, and it is usually very demonstrative and striking. It seems that the child's neck is very short (although there is no anatomical defect), the head seems to be located directly on the shoulders. With age, the degree of these manifestations gradually decreases. In these same children, attention is drawn to the severity of the transverse folds on the neck with persistent weeping in the area of these folds. It can be assumed that the symptom of a short neck occurs as a result of overextension of the neck during difficult childbirth, followed by a reflex contraction of the neck like the “accordion phenomenon”. Later, it is these children who develop another very important sign - a sharp protective tension in the cervical-occipital muscles.
Assessing the condition of the abdominal wall is very important. It is known that many newborns have a flabby, flat stomach, and in these cases it is impossible to exclude a violation of the contractility of the abdominal muscles as a result of birth injuries to the thoracic spinal cord. This is especially demonstrative when the lesion is predominantly unilaterally localized - the “weak” half of the abdominal wall protrudes slightly, the navel moves when screaming. With a bilateral lesion, it is more difficult to judge. The following test can be useful: if such a newborn cry is weak, then when the doctor’s hand presses on the child’s stomach, the voice becomes much louder.
Priapism, a spontaneous erection of the penis in a newborn, should be considered equally unfavorable. Pediatricians often encounter this sign, but do not know how to interpret it. At the same time, in adult neurology, this symptom is well known and indicates significant spinal pathology.
We tried to consider some possibilities for a general examination of a newborn to look for signs that would suggest one or another neurological pathology. Each of the above signs cannot be considered conclusive, but taken together they acquire great diagnostic meaning. In any case, only a doctor specializing in neonatal neurology can resolve your doubts.
<< Return to contents
Perinatal cerebral depression (nervous hypoexcitability)
Low motor and mental activity of the child, which is always below his motor and intellectual capabilities; high threshold and long delayed period for the occurrence of all reflex and voluntary reactions. Depression is often combined with low muscle tension and reflexes, slow switching of nervous processes, emotional lethargy, decreased motivation and weakness of volitional efforts.
Hypoexcitability can be expressed to varying degrees and manifest itself either episodically or persistently. The episodic occurrence of the syndrome is characteristic of somatic diseases, especially pathologies of the gastrointestinal tract, accompanied by malnutrition. Sometimes mild but persistent manifestations of the syndrome may be due to the type of higher nervous activity. The predominance of cerebral depression in the first months of life is observed in cases of prematurity, in children who have suffered oxygen starvation, or intracranial birth trauma. Severe and persistent depression is often accompanied by delayed psychomotor development, which acquires some characteristic features.
Delayed psychomotor development in hypodynamic syndrome is characterized by a delayed formation of all conditioned reflexes. During the neonatal period and in the first months of life, this manifests itself in a lag in the development of the conditioned reflex during feeding; subsequently, the development of all food conditioned reflexes is delayed (reflex to the position of feeding, the appearance of a breast or a bottle of milk, etc.), the development of food, and then visual and auditory dominance and sensitive local reactions is delayed. Particularly characteristic is the delay in the development of chain motor combined reflexes, which most clearly begins to manifest itself from the second half of life! Such a child at the age of 6-8 months does not pat a blanket or toy with his hand, does not knock an object against an object, does not repeatedly throw out an object by the end of the year, does not put an object into an object. This is also manifested in vocal reactions: the child rarely repeats sounds and syllables, i.e., performing single movements and pronouncing individual sounds, he does not strive to repeat them. As a result of the delay in the formation of conditioned reflexes on the combination of a word with an object or action in both a specific and non-specific situation, the initial understanding of speech and submission to verbal commands in these children occurs at a later date. At the same time, a lag in such functions as object-manipulative activity, crawling, babbling, speech understanding, and one’s own speech is formed.
In the case of hypoexcitability, the formation of positive emotional reactions is noted at a later date. This manifests itself both when communicating with an adult and in the spontaneous behavior of a child. During the newborn period, when communicating with an adult, such children usually lack oral attention; at the age of 2 months, the reaction of joyful animation at the sight of an adult and a gentle voice is not expressed or is weakly expressed. Often, instead of facial expressions of animation, you can only see a reaction of concentration in a child. A smile appears after 8-9 weeks; its appearance requires a complex of stimuli, including proprioceptive ones, and their repetition; the latent period of a smile in response to a stimulus is extended.
While awake, the child remains lethargic and passive; indicative reactions occur mainly to strong stimuli. The reaction to novelty is sluggish and in most cases has the character of passive amazement, when a child with wide open eyes remains motionless at the sight of a new object, without making active attempts to approach it or grab it. The longer the period of absence of active wakefulness and indicative-exploratory behavior, the more pronounced the lag in psychomotor development.
The revival complex, one of the main manifestations of active forms of emotional behavior in a child in the first months of life, is either absent with hypoexcitability or manifests itself in a rudimentary form: a weak facial reaction without sparkle in the eyes and vocal reactions, or the absence of a motor component, clear vegetative manifestations. Active negative emotional reactions are also weakly expressed and have almost no effect on the child’s general behavior.
Features of the emotional sphere determine the secondary underdevelopment of intonation expressiveness of vocal reactions, as well as the specifics of the formation of sensory functions. Thus, at the second age stage, a hypoexcitable child usually fixes and tracks an object well, but the movements of his eyeballs following a moving object do not begin immediately, but after a certain latent period, as is typical for a newborn: the eyes seem to constantly catch up with the object moving in the field. view subject. These visual reactions are variable, and their occurrence often requires special optimal conditions: a certain state of the child, sufficient strength and duration of the stimulus, etc. In the second age period, these reactions most clearly and often occur not in a supine position, but in a vertical position. position in the arms of an adult. A feature of visual perception with hypoexcitability at this age stage is also that the child spontaneously almost does not examine surrounding objects, he does not actively search for a stimulus. A hypoexcitable child usually turns his head and eyes towards an invisible sound source after repeated repetition and a long latency period; auditory perception, like visual perception, usually does not acquire a dominant character.
Delayed psychomotor development in hypoexcitability syndrome is characterized by developmental disproportion, which manifests itself in all forms of sensory-motor behavior. Thus, with sufficient development of differentiated emotional reactions to “friends” and “strangers,” the child shows active joy in communicating with friends and protest in communicating with strangers, i.e., at the age stages, insufficient communication activity remains pronounced. Along with the timely development of individual sensory functions, there is a lag in the formation of intersensory connections, especially in the tactile-kinesthetic analyzer system, so hypoexcitable children later begin to examine and suck their hands, feel toys, and their hand-eye coordination is formed with a delay. The lack of active exploratory behavior is expressed in the disproportionality of the development of visual perception. Therefore, with sufficient development of differentiated visual perception in a child, the automatic nature of object tracking can be maintained.
With a dynamic quantitative assessment of age-related development, a child with hypoexcitability syndrome loses 7-9 points at different periods, with the maximum loss observed at the age of 4-5 months, when normally the first intersensory connections and active forms of behavior should be actively formed.
<< Return to contents
Perinatal cerebral hyperexcitability
Motor restlessness, emotional instability, sleep disturbance, increased innate reflexes, increased reflex excitability, a tendency to pathological movements, often in combination with a reduced threshold of convulsive readiness. Hyperexcitability is not causally specific and can be observed in children with perinatal pathology, some hereditary enzymopathies and other metabolic disorders, congenital childhood nervousness and minimal brain dysfunction. These children may not have a pronounced lag in psychomotor development, but with a thorough examination it is usually possible to note some mild deviations.
Disorders of psychomotor development in hyperexcitability syndrome are characterized by a lag in the formation of voluntary attention, differentiated motor and mental reactions, which gives psychomotor development a peculiar unevenness. By the end of the first year of life, such children usually have well-expressed cognitive interest in the environment and active forms of communication, and at the same time, with strong emotions, a general complex of revival with diffuse motor reactions may appear.
All motor, sensory and emotional reactions to external stimuli in a hyperexcitable child arise quickly, after a short latent period, and fade away just as quickly. Having mastered certain motor skills, children constantly move, change positions, constantly reach for and grab objects. At the same time, manipulative research activities, imitative games and gestures are poorly expressed. Children usually show a keen interest in their surroundings, but increased emotional lability often makes it difficult for them to communicate with others. Many of them have a long-term reaction of fear when communicating with unfamiliar adults with active reactions of protest. Typically, hyperexcitability syndrome is combined with increased mental exhaustion. When assessing the age-related development of a hyperexcitable child, they are usually classified not as a delay group, but as a “risk group” if hyperexcitability is not combined with other neurological disorders.
<< Return to contents
Postpartum intracranial pressure regulation disorder
Hypertensive-hydrocephalic syndrome
Increased and unstable intracranial pressure in young children is often combined with hydrocephalic manifestations, which are characterized by the expansion of certain intracerebral spaces as a result of the accumulation of excess amounts of cerebrospinal fluid. Increased intracranial pressure in newborns and infants can be transient or permanent, hydrocephalus can be compensated or subcompensated, which, along with the anatomical and physiological characteristics of early age, determines a wide range of clinical manifestations.
In most cases, with hypertensive-hydrocephalic syndrome, there is an increase in the size of the head, which is determined by dynamically measuring its circumference and comparing it with the dynamics of height and body weight. An increase in head circumference that exceeds normal by more than 2 sigma deviations is considered pathological. As the head circumference increases, a disproportion between the cerebral and facial skulls is revealed. Enlargement of the skull can be asymmetrical due to a unilateral pathological process or a defect in child care.
An increase in intracranial pressure in infants is also accompanied by a divergence of cranial sutures, which can be determined by palpation and x-ray examination. Dehiscence of the sutures occurs quickly with progressive hydrocephalus and more slowly when intracranial pressure is mildly increased or has stabilized. When percussing the skull o.
Another sign of increased intracranial pressure is bulging and enlargement of the large fontanel. With severe hydrocephalic syndrome, the small and lateral fontanelles may be open. It should, however, be borne in mind that changes in cranial sutures and fontanels are detected only at a certain stage of development of the pathological process, therefore their absence during a single examination cannot be regarded as evidence against the presence of hypertensive-hydrocephalic syndrome.
With increased intracranial pressure in newborns and infants, the venous network of the scalp expands and the skin on the temples becomes thinner.
Neurological symptoms in hypertensive-hydrocephalic syndrome depend both on the severity of the syndrome and its progression, and on the brain changes that caused it. First of all, the behavior of children changes. They become easily excitable, irritable, the cry is sharp, shrill, sleep is superficial, children often wake up. This complex of signs is more typical for the predominance of hypertension syndrome. With hydrocephalic syndrome, on the contrary, children are drowsy in most cases. Decreased appetite, regurgitation, and vomiting lead to a decrease in body weight. Damage to the cranial nerves is manifested by the “setting sun” symptom, convergent strabismus, and horizontal nystagmus.
Muscle tone changes depending on the severity of intracranial hypertension and the course of the disease. In the first months of life, with increased intracranial pressure, especially if it is accompanied by hyperexcitability and the volume of the skull is not increased, muscle tone is often increased, tendon reflexes are high, with an expanded zone, and foot clonus is sometimes observed. In hydrocephalic syndrome with moderate intracranial hypertension, muscle hypotonia is initially observed. If hydrocephalus progresses, you can later notice an increase in muscle tone, first in the legs. This is due to the stretching of the pyramidal fibers of the parasagittal region due to the enlargement of the ventricles of the brain.
In newborns and infants with hypertensive-hydrocephalic syndrome, hand tremor is often pronounced. It can be frequent, small-scale or rare, large-scale, such as hemibalism. Seizures are observed much less frequently; they usually occur with a rapid increase in intracranial hypertension.
Changes in the fundus of the eye in young children do not necessarily develop due to the possibility of an increase in the volume of the skull due to divergence of the cranial sutures. However, in some cases, one can detect dilation of the veins, blurring of the boundaries of the optic nerve nipple, and later, with the progression of hydrocephalus, its swelling and atrophy.
Determination of cerebrospinal fluid pressure during lumbar puncture, which is normally 50-100 mmH2O in newborns, is important for diagnosing hypertension syndrome. Art., for breastfeeding - 60-150 mm of water. Art. With hypertension syndrome, cerebrospinal fluid pressure in infants can increase to 200-3Q mm of water. Art. and higher. The composition of the cerebrospinal fluid in hypertensive-hydrocephalic syndrome depends on the characteristics of the pathological process as a result of which it arose, the nature of the course of the syndrome, and the stage of its development. More often, a normal composition of the cerebrospinal fluid is observed, but there may be protein-cell or cell-protein dissociation.
Along with clinical, ophthalmological and liquorological data, the following are important for the diagnosis of hypertensive-hydrocephalic syndrome: transillumination of the skull, EchoEG, craniography, computed tomography.
The transillumination method is safe, it can be performed repeatedly and on an outpatient basis. The principle of the method is to propagate light rays in a space filled with liquid. Normally, in newborn infants, a ring of luminescence with a width of 0.5 to 3 cm appears around the tube with a light source, depending on the density of the bones of the skull. The most intense glow is observed in the frontal regions (up to 3 cm), the least in the occipital region (0.5-1 cm). An increase in the boundaries of the luminescence occurs when the subarachnoid space expands to 0.5 cm. Transillumination of the cavities of intracerebral tissue or ventricles is possible only when the thickness of the brain tissue is less than 1 cm.
In children with external and internal hydrocephalus, a symmetrical glow is detected. Asymmetrical luminescence occurs with unilateral expansion of the ventricle and suoarachnoid space.
On EchoEG with hydrocephalus, an increase in the number of reflected echo signals, ventricular index (normal 1.9) and amplitude of echo pulsations is recorded. In the case of asymmetric enlargement of the ventricular system, the m-exo is displaced in the direction opposite to the enlarged ventricle.
In infants with a slight increase in intracranial pressure without dehiscence of cranial sutures, craniography does not provide sufficient information for diagnosis. At the same time, it is the craniogram that can provide objective evidence of increased intracranial pressure. With the progression of hydrocephalus, craniograms show divergence of the cranial sutures, most often the coronal and sagittal sutures, already after 2-3 weeks. Asymmetrical expansion of the cranial sutures indicates the localization of the lesion. Thinning of the bones of the cranial vault and pronounced digital impressions in children of the first year of life indicate the relative duration of the process that led to the limitation of intracranial space.
Computed tomography is a safe and painless method of x-ray examination of the skull and brain structures, the radiation exposure is minimal (0.3 load when taking a regular x-ray of the skull). For young children, the significance of these advantages is very great. In addition, it can be performed on an outpatient basis. Computed tomography gives a clear picture of the size of the ventricles of the brain in hydrocephalus, as well as the presence and location of lesions.
The depth and nature of the delay in psychomotor development in hydrocephalus and hypertension syndrome vary widely depending on the primary changes in the nervous system that caused hydrocephalus, and those secondary to increasing hypertension. If the destructive changes in the brain that caused hydrocephalus were pronounced, even if hydrocephalus is compensated by conservative or surgical measures, the child’s development is significantly delayed. At the same time, the addition and progression of hypertensive-hydrocephalic syndrome in any pathology makes the developmental delay even more pronounced and peculiar, despite compensation of the primary process. Finally, with timely effective compensation of both the primary process and hydrocephalus, a slight developmental delay, often partial, is quickly eliminated.
<< Return to contents
Osteopathic examination
An examination by an osteopathic doctor involves not only a neurological examination, but also a search for anatomical abnormalities in the structure of the skull, cervical vertebrae, sacrum, ribs, etc. All this is of great importance for the child’s health, since the slightest deviations in anatomy are projected on an enlarged scale into the future life of the baby. Osteopathic diagnosis is carried out by a doctor and includes:
- Examination: determination of the arch of the body, position of the limbs, behavior of the child.
- Assessing the amplitude, strength and rhythm of the primary respiratory mechanism.
- Assessment of the pattern of the craniosacral system.
- Testing the mobility of the cervical and lumbosacral spine.
- Global skull test, assessing the mobility of each of the bones of the arch and base.
- Diagnosis of intraosseous injuries of the skull and sacrum.
After the examination, the osteopathic doctor gets an idea of all the anatomical disorders in the child’s body and immediately begins treatment.
Prevention of neurology in children
From the first days of life, the child must maintain a sleep-wake schedule. Physical activity should correspond to the characteristics of the body and age. The emotional situation in the family plays an important role. Even if you follow these rules, you can practically eliminate the risk of childhood neurology. If parents and close relatives have been diagnosed with diseases of the nervous system, it is necessary to closely monitor the manifestation of symptoms in the child.
Prevention measures:
- elimination of emotional and physical fatigue;
- quarrels and scandals in the family should never occur in front of a child;
- if a child has suffered a stressful situation, it is necessary to consult a specialist and undergo examination by a neurologist;
- exclusion of overprotection (the child can become not only withdrawn, but also acquire persistent mental disorders);
- the approach to raising a child should be the same for both parents;
- if a child’s living conditions change dramatically, then he needs help to cope with his experiences (for example, moving to another city, transferring to a new kindergarten or school).
The Contact clinic employs highly qualified doctors and a sufficient level of professionalism. If there is a suspicion of neurology in a child, a visit to a specialist cannot be postponed. The clinic's doctors use individual approaches to children and their parents. The advantage of visiting a private center is the absence of queues and the reception of small patients in comfortable rooms. The child will not receive additional stress, which can aggravate the situation, as with a long wait for consultation in government institutions.
Osteopathic treatments
Osteopathic treatment of central nervous system lesions in newborns is aimed at eliminating anatomical dysfunctions in the newborn’s body, restoring normal biomechanical relationships of all bones and joints, as well as soft tissues damaged during traumatic birth. Examples of techniques that are included in the osteopathic course of treatment for newborns:
- Fascial decompression of the sacrum, sacrolumbar joints.
- Removal of blocks at the level of the articulation of the first cervical vertebra and the skull.
- Balancing the tone of the thoracoabdominal diaphragm.
- Release (normalization of muscle tone) of the upper aperture of the chest, collarbones, shoulder blades, first rib.
- Decompression of sphenobasilar synchondrosis.
- Balancing the mutual tension membranes of the cranial cavity and spinal cord.
- Elimination of intraosseous damage to the occipital, temporal, and sphenoid bones resulting from injuries during childbirth.
- Correction of blood outflow and cerebrospinal fluid circulation in the cranial cavity.
- Balancing and balancing techniques.
The goal of treatment is to ensure that there are no tensions, blocks, or dysfunctions in the newborn’s body, so that it functions as an ideally tuned biomechanical system. The entire future life of the baby and diseases that may appear due to missed birth injuries depend on this.