Symptoms
Among the symptoms of cerebral atherosclerosis are:
- Certain signs of cerebral atherosclerosis include the following symptomatic picture:
- Sleep problems: insomnia, disturbing dreams, difficulty getting up and problems falling asleep again;
- Loss of sensation in half of the body;
- Severe, frequently recurring headaches;
- Increased cholesterol levels in blood tests:
- Changes in gait and loss of coordination;
- Changes in vision, flickering of “spots” before the eyes, tinnitus;
- Emotional changes: irritability, depression, tearfulness and anxiety;
- Hot flashes and sweating of the face;
- Increased fatigue, constant weakness and absent-mindedness;
- Trembling of the chin and limbs;
- Memory impairment, problems with short-term memory;
- The appearance of facial asymmetry. Source: L.S. Bizhanova. Ischemic brain disease // Bulletin of KazNMU, No. 2, 2015, pp. 241-242 Shabir O.
Clinical signs do not appear immediately. This happens long after cholesterol has begun to be deposited. Symptoms appear after the lumen of the arteries and capillaries of the brain narrows so much that 15% or more less blood begins to flow to the organs.
Signs of the disease depend on the stage:
1. In the first stages, the disease makes itself felt only after physical or emotional stress and quickly passes when the patient goes into a state of rest. The main symptom is asthenia, accompanied by fatigue, weakness, decreased alertness, and general lethargy. Rarely, sleep is disturbed, insomnia or daytime sleepiness occurs. Mostly, patients complain of headaches, tinnitus, and memory impairment. In the latter case, patients remember the past well, but do not remember new information well.
2. As the disease progresses, anxiety, suspiciousness, depression, and mood swings appear. Memory impairments become more pronounced, to the point that the patient does not remember what happened to him today. There is a constant headache and noise in the ears, speech is persistently impaired - it becomes unclear, diction changes, patients feel dizzy and have unsteady gait. Hearing and vision also deteriorate, limbs and head shake, and a person stops thinking logically and clearly.
3. At the last stage of atherosclerosis, dementia develops; the patient may behave like a child or become aggressive and tearful. Most people completely or partially lose their memory and cease to be interested in the world around them and the events in it. The ability to navigate in time and space is lost, the patient needs constant care because he loses self-care skills in everyday life. This stage is irreversible.
Classification of vascular diseases of the brain
There are two main groups of vascular pathologies: acute and chronic cerebrovascular accidents. The first group is divided into three subgroups: transient cerebrovascular accidents, cerebral strokes, mixed strokes. Transient disorders of cerebral circulation include transient ischemic attacks and hypertensive crises. Brain strokes are ischemic and hemorrhagic. Hemorrhagic strokes are divided into subarachnoid hemorrhage, parenchymal-subarachnoid hemorrhage, and ventricular-parenchymal-subarachnoid hemorrhage. Ischemic strokes, in turn, are divided into lacunar, atherothrombotic, cardioembolic and hemodynamic stroke.
The second group includes: chronic subdural hematoma, initial manifestations of cerebrovascular insufficiency, subcortical vascular dementia, discirculatory encephalopathy. The initial manifestations of cerebrovascular insufficiency are divided into two stages. The first stage is characterized by the absence of neurological manifestations. At the second stage, neurological manifestations are clearly expressed. Discirculatory encephalopathy is the most common among chronic cerebrovascular accidents. It is divided into three main stages:
- The first stage is moderately severe, characterized by diffuse symptoms. The patient may complain of short-term headaches, periodically suffer from sleep disorders and increased irritability.
- The second stage is more pronounced; clinical manifestations form in it. The person often experiences surges in blood pressure, loss of space, and cognitive impairment. As a rule, at this stage the disease is most often diagnosed.
- The third stage is pronounced, during which irreversible changes occur in the body. Serious disturbances in memory and cerebral circulation in general appear. In rare clinical situations, complications in the form of strokes are observed (in the absence of timely consultation with a doctor).
Diagnostics
A neurologist deals with this disease. First, the doctor collects anamnesis, interviews the patient about complaints, and conducts a series of tests. So, the following factors indicate the presence of the disease:
- The patient cannot look up;
- Reflexes are weakened or excessively increased, most often asymmetrically;
- In a standing position, legs together, arms extended forward, the patient cannot maintain balance;
- When the patient stretches his arms forward, his fingers tremble and become weak;
- Closing his eyes, a person cannot bring his finger to the tip of his nose.
These are indirect signs that only allow us to make an assumption about the presence of atherosclerosis. Therefore, a comprehensive examination is then carried out with consultations of other doctors - ENT, ophthalmologist, etc., depending on the existing disorders. At the medical office, you can get advice from related specialists on any disease, including in cases of suspected cerebral atherosclerosis. Source: Berwick J, Francis SE. Neurovascular dysfunction in vascular dementia, Alzheimer's and atherosclerosis // BMC Neurosci. 2021 Oct 17;19(1):62. doi:10.1186/s12868-018-0465-5.
In addition, it is necessary to undergo a biochemical analysis of the blood lipid spectrum (cholesterol, triglycerides, etc.)
List of instrumental studies:
- REG – radioencephalogram;
- Angiography of cerebral vessels;
- Duplex head scanning;
- Ultrasound Dopplerography of cerebral vessels;
- MRI of cerebral vessels;
- CT – computed tomography;
- EEG – electroencephalogram.
The diagnostic capabilities of a medical doctor allow you to accurately diagnose atherosclerosis, the extent of the disease and choose an effective treatment regimen.
Diagnosis of pathology
If the symptoms described above appear, it is recommended to immediately consult a cardiologist or neurologist. During the initial examination, the specialist collects an anamnesis of the patient’s life, asks in detail about his complaints (how long ago and under what circumstances they appeared), about diseases of the cardiovascular system of his closest relatives. Based on these data, further examination is prescribed.
To diagnose vascular diseases of the brain, they resort to laboratory and instrumental diagnostics. First of all, the patient is prescribed a general and biochemical blood test to determine the level of cholesterol, glucose, triglycerides, lipoproteins and prothrombin index (PTI). These substances affect the functioning of the heart and blood vessels. Biochemical indicators are very important in making a diagnosis. An increased level of leukocytes indicates the presence of an inflammatory process in the body. Among the instrumental diagnostic methods, the following are in particular demand:
● electrocardiography (ECG). This is a simple technique that does not require additional preparation. The essence of an ECG is to record the electrical potentials of the heart, due to which it is possible to detect changes in rhythm, electrolyte deficiency and other initial signs of cardiovascular pathologies;
● Doppler ultrasound of the vessels of the neck and brain (USDG). This is a modern, highly informative diagnostic method. It is used to determine damage to the arteries and indicates insufficient blood supply to the brain. With its help, it is possible to assess blood flow in the vessels of the neck and head;
● duplex scanning of blood vessels. Thanks to color contrast of flows during duplex scanning, it is possible to more clearly distinguish between moving and stationary objects (blood and vessels, respectively);
● ultrasound examination of the heart (ultrasound). This technique makes it possible to visually view the contractions of the heart muscle, assess the condition of its valves, and diagnose heart failure;
● echocardiography (EchoCG). Sometimes specialists prescribe echocardiography in addition to an ECG. This is a highly accurate examination method, with its help it is possible to assess the condition and determine the size of the valves;
vascular magnetic resonance imaging (MRI). This is a completely safe technique for the body (there is no radiation), it shows the lumen and patency of large vessels, and makes it possible to detect abnormalities in vascular development.
Treating atherosclerosis
- Shishkin A.A.
- Volkov A.M.
- Kabirov A.V.
- Baranov V.S.
Shishkin Andrey Andreevich
Candidate of Medical Sciences. Surgeon, proctologist, phlebologist at SM-Clinic. Proficient in all modern methods of conservative and surgical treatment of diseases of the veins of the lower extremities (including sclerotherapy, EVLT - endovasal laser coagulation, traditional phlebectomy)
Read moreVolkov Anton Maksimovich
Phlebologist, surgeon at SM-Clinic. Performs operations with a modern proprietary method of treating varicose veins using a laser (modified endovenous laser coagulation. M-EVLC).
Surgical treatment of varicose veins of any complexity (phlebectomy, miniphlebectomy) More detailsKabirov Alexander Vitalievich
Cardiovascular surgeon at SM-Clinic. Candidate of Medical Sciences Proficient in all modern methods of conservative and surgical treatment of diseases of the veins of the lower extremities (including sclerotherapy, EVLT - endovasal laser coagulation, traditional phlebectomy)
More detailsBaranov Vladimir Sergeevich
Cardiovascular surgeon at SM-Clinic. Candidate of Medical Sciences Treats lower varicose veins using non-surgical and surgical methods (aesthetic sclerotherapy, ECHO sclerotherapy, stem sclerotherapy, phlebectomy, miniphlebectomy, EVLT).
More details
Violation of venous circulation in the brain
The brain is a complex structure, its normal functioning depends on the state of blood circulation. In addition to the need to deliver oxygen and glucose to the nervous tissue, the outflow of venous blood and the removal of toxins with it, the result of cell activity, is important. If this process is disrupted, chronic venous insufficiency of the brain is formed.
A peculiarity of the vessels of the brain is the course of the veins: it does not coincide with the direction of the arteries, and a network is formed that is independent of them. If the outflow of blood through one of the vessels is impaired, venous blood is directed to the other, and compensatory expansion occurs. A prolonged decrease in tone leads to vascular atrophy, they collapse, and the risk of thrombosis increases. Dilated vessels contribute to the development of venous circulation insufficiency, the functioning of the valves is disrupted, they do not close tightly, and the direction of blood flow is disrupted.
Stages of the pathological process
The following stages are distinguished during cerebral venous insufficiency:
- latent: no clinical symptoms, no complaints;
- cerebral venous dystonia: some symptoms are observed: headaches, weakness;
- venous encephalopathy: severe symptoms caused by organic lesions are observed, venous outflow is impaired in all areas of the brain, there is a high risk of hemorrhages from dilated vessels.
Classification
There are chronic and acute variants of venous circulation in the brain. Chronic include venous congestion and venous encephalopathy, acute include venous hemorrhage, thrombosis of the veins and venous sinuses, thrombophlebitis.
Causes and risk factors
Insufficiency of cerebral venous circulation can be caused by diseases or individual characteristics of the patient. The most common causes of pathology:
- neoplasms in brain tissue can cause disruption of venous outflow;
- head injuries that impair blood circulation to the brain;
- injuries during childbirth;
- hematomas formed as a result of stroke, atherosclerosis, bruises and other causes contribute to the formation of tissue edema, which complicates the outflow of blood from the affected area;
- blood clots and embolisms narrow the lumen of the vessel or completely close it, preventing the movement of blood;
- diseases of the spinal column, in which deformed sections of the canals compress the vessels and disrupt blood flow, also cause venous insufficiency;
- vascular features: hereditary predisposition and impaired development of veins can provoke the development of a violation of the outflow of venous blood.
Circulatory disorders can be physiological and occur when coughing, sneezing, or physical strain. Such short-term deviations do not cause significant harm to health.
One-time attacks of cerebral circulatory disorders do not cause serious consequences for the body. However, prolonged blood stagnation can contribute to the development of serious consequences. The following risk factors increase the likelihood of cerebral venous insufficiency:
- frequent stress;
- smoking;
- alcohol abuse;
- prolonged dry cough;
- professional singing;
- hypertension;
- heart failure;
- reading in the wrong position
- professional swimming;
- frequent wearing of clothes that compress the neck;
- chronic rhinitis:
- work in high-altitude, underwater, underground professions;
- office work that involves staying in a position with the head tilted or turned;
- frequent physical activity of high intensity
Clinical manifestations
Disturbances of venous circulation, as a rule, are genetically determined. Currently, the role of the initial tone of the veins in the formation of venous discirculation is undeniable. Constitutional and hereditary factors are key for the development of venous dyshemia. Patients with a family “venous” history usually have several typical manifestations of constitutional venous insufficiency - varicose veins or phlebothrombosis of the lower extremities, hemorrhoids, varicocele, impaired venous outflow from the cranial cavity, esophageal varicose veins. Pregnancy is often the trigger.
Typical complaints:
- morning or afternoon headache of varying intensity;
- dizziness, depending on changes in body position;
- noise in the head or ears;
- visual disturbances (decreased visual acuity, photopsia);
- “tight collar” symptom - increased symptoms when wearing tight collars or ties;
- “high pillow” symptom - increased symptoms when sleeping with a low headboard;
- sleep disorders;
- feeling of discomfort, “fatigue” in the eyes in the morning (symptom of “sand in the eyes”);
- pastiness of the face and eyelids in the morning (with a pale, purple-cyanotic tint);
- mild nasal congestion (outside the symptoms of acute respiratory infections);
- darkening of the eyes, fainting;
- numbness of the limbs.
Signs of impaired cerebral venous blood flow are related to weather conditions. Headaches are poorly controlled by analgesics; often some relief is brought only by a change in body position - in a horizontal position, venous blood flow is redirected along collaterals - bypassing the affected vessel.
The patient’s psyche changes in such a way that minor experiences can lead to neuroses. Tearfulness increases, the patient often breaks into a scream. Mania and depression are observed. Severe damage leads to psychosis, accompanied by hallucinations and delusions; this can make the patient dangerous to himself and others.
Diagnostics:
- radiography determines the strengthening of the pattern of the veins of the skull, which indicates the presence of a pathological process;
- angiography is a contrast method for diagnosing blood stagnation, determining the patency of blood vessels;
- computed tomography and magnetic resonance imaging make it possible to accurately determine the presence of a pathological process in the brain, as well as in surrounding tissues;
- ultrasound examination of the veins of the brain and neck;
- rheoencephalography is a functional diagnostic method that assesses the condition of blood vessels;
- An increased level of pressure in the ulnar vein allows one to suspect abnormalities in the vessels of the brain.
Therapy is complex and includes several areas
- drug treatment;
- non-drug treatment: physiotherapy, massage, physical therapy;
- surgery.
Drug therapy
The following drugs are used to normalize cerebral circulation:
- venotonics strengthen the vascular wall, reduce permeability, have an analgesic effect, and eliminate inflammation;
- diuretics to eliminate swelling;
- neuroprotectors improve nutrition and metabolism of the brain;
- anticoagulants to thin the blood and prevent thrombosis;
- vitamin therapy (vitamins B and PP).
Non-drug treatment
There are a number of non-drug therapies that are effective as an additional treatment method and improve vascular tone. However, before treating impaired cerebral venous outflow with their help, it is necessary to assess individual risks and contraindications: in some cases, such procedures can lead to the opposite effect and worsen the patient’s condition.
Applicable:
- head and neck massage;
- oxygen therapy;
- foot baths;
- physical therapy: breathing exercises, neck exercises, yoga classes.
Intern of the ophthalmology department Gurlo A.I.
Head of the department ophthalmological department Rudova
Treatment
The basis of treatment for this pathology is lifestyle adjustments. This means:
- lipid-restricted diet,
- rejection of bad habits,
- physical activity regimen,
- avoiding stress,
- treatment of chronic diseases.
The focus of drug therapy is the use of lipid-lowering drugs, antiplatelet, antihypertensive and antioxidant drugs, drugs to improve microcirculation and symptomatic therapy. Therapy, as a rule, takes a very long time and depends on the stage at which it was started.
In case of severe stenotic processes, surgical treatment is recommended for the patient. Most often, surgical intervention is performed on the internal carotid arteries. Source: E.A. Shirokov. Stenosing atherosclerosis of the cerebral arteries: modern strategies for diagnosing and treating patients // Consilium Medicum, vol. 18, no. 9, 2021, pp. 37-42.
Treatment for this disease is aimed at ensuring that metabolic processes are restored, and harmful cholesterol no longer settles on the walls of blood vessels. At the same time, attention is also paid to restoring blood circulation and normalizing the nutrition of brain tissue.
Drug therapy
This is the most important part of the comprehensive treatment of atherosclerosis. Patients may be prescribed several groups of medications:
- Statins - reduce the size of cholesterol plaques, reduce the risk of narrowing of the main arteries of the brain, and stop the growth of plaques.
- Antiplatelet agents – reduce blood viscosity and prevent blood clots.
- Fibrates are similar in action to statins, but do not affect the size of plaques, but lower the triglyceride content in the blood.
- Means for restoring vascular function.
- Bile acid sequestrants prevent cholesterol from being absorbed from food.
- Nootropics and medications that improve metabolic processes in nervous tissue.
- Hypotensives that stabilize blood pressure and help prevent stroke.
- Vitamin and mineral complexes to improve the general condition of the body. They must contain vitamins A, C, group B and nicotinic acid.
Medicines are taken in long courses, and most of them are taken for life with periodic dosage adjustments.
Surgical treatment
Operation is a last resort, indications for it:
- narrowing of the lumen of the carotid artery by 70% or more;
- condition after a minor stroke;
- recurrent ischemic attacks.
Surgical options:
- bypass - the formation of a vessel bypassing the one affected by cholesterol deposits;
- endarterectomy - a procedure to remove cholesterol plaques along with a small amount of tissue that lines the vessel from the inside;
- stenting using endoscopic technology - an expanding structure impregnated with a composition that dissolves cholesterol is installed in the vessel.
Operations can be performed under general anesthesia or local anesthesia. An anesthesiologist is consulted before the operation. The length of hospital stay varies depending on the technique, as do recommendations for the recovery period. SM-Clinic doctors inform patients in detail about all the nuances and are ready to answer any questions related to treatment at the initial consultation. Consultation on the operation is free of charge.
You can find out more about discounts on preoperative examinations by following the link.
Symptoms of cerebral vasoconstriction
In the initial stages, narrowing is manifested by the following signs:
- Decreased memory (especially often in such situations, people forget events that happened to them quite recently).
- Deterioration in learning and ability to work.
- Dizziness.
- Chronic fatigue.
- Loss of interest in what is happening.
- Depressive states.
- Mood swings.
- Emotional instability.
- Problems with concentration.
- Sleep disorders: insomnia, restless sleep.
If treatment is carried out at this stage, the disorders can be eliminated and the patient’s quality of life can be restored.
As the pathology progresses, the following are observed:
- Speech disorders.
- Noise in the head.
- Hearing loss.
- Hand trembling.
- Clumsiness of movements.
- Change in gait.
Diet
Changing your diet is also a way to improve your well-being and is a great help for other treatment methods. Atherosclerosis very often progresses precisely against the background of poor nutrition and lifestyle, so it is necessary
- follow a certain diet:
- reduce consumption of red and fatty meats and meat in general;
- limit the consumption of confectionery products and baked goods;
- eat as few egg yolks as possible;
- limit solid vegetable fats – margarine – in the diet;
- completely eliminate alcohol, sausages, fast food, and canned food.
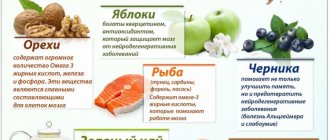
Recommended products include vegetables (fresh, pickled, dried), cereals (rice, buckwheat, barley, millet, oats, flax, etc.), dried, fresh and dried fruits, turkey and chicken fillets, river and sea fish.
You need to eat at least 5 times a day at the same time in small portions. It is necessary to avoid fried foods and prepare food using the methods of boiling, steaming, stewing, and baking.
Possible risks associated with atherosclerosis
The most dangerous complication is a stroke. If at the same time the patient has poor eating habits, is overweight, moves little and is regularly exposed to stress, then with an 80% probability he will become disabled as a result, unable to care for himself. The mortality rate is also high.
Prevention
To prevent cerebral atherosclerosis, you need to avoid smoking, follow a diet, and keep yourself in good shape with moderate physical activity. It is very important to establish a psycho-emotional background, protect yourself from stress, and if this is not possible, then take courses of sedatives and amino acids, for example Glycine.
| Name of service (price list incomplete) | Price, rub.) | In installments* |
| Appointment (examination, consultation) with a cardiovascular surgeon, primary, therapeutic and diagnostic, outpatient | 1 750 | — |
| Program “Risk of atherosclerosis and ischemic heart disease, predisposition to dyslipidemia” | 19 000 | — |
* You can read more about the conditions here - Treatment on credit or in installments.
Risk group
The risk group includes people with infectious pathologies during the neonatal period. The likelihood of developing vascular diseases of the brain increases significantly with hemolytic anemia, surgery and head injuries. The mother’s poor lifestyle (abuse of alcohol and tobacco products) can also negatively affect the condition of the child’s brain. A family history of cardiovascular pathologies (for example, myocardial infarction or arterial hypertension in close relatives) doubles the risk of developing cerebrovascular diseases.