Reasons for development
Tetraparesis is divided into acquired and congenital. The first type of disease occurs due to spinal injury, cerebral hemorrhage, the appearance of benign or malignant formations, encephalitis and polyneuritis. Congenital - due to complications during intrauterine development. Also the reason may be:
- Krabbe disease;
- Arnold-Chiari syndrome;
- cerebral palsy;
- Guillain-Barre syndrome;
- obstruction of cerebral vessels;
- myasthenia gravis;
- high intracranial pressure;
- complication after surgery on the spine or brain;
- dropsy of the brain.
Journal "Emergency Medicine" 5(30) 2010
In the structure of emergency medical calls, in second place after visits to patients with cardiovascular pathology (18.4%) are calls to patients with acute neurological pathology (13.4%). Among acute and emergency conditions of neurological origin, a large number of deaths and disability (second to cerebrovascular disorders) are cases of acute tetraparesis.
Timely diagnosis of the genesis of tetraparesis and adequate treatment of such a patient determine the further course of the disease and its prognosis. Errors in the diagnosis and treatment of acute neurological pathology with tetraparesis at the prehospital stage quite often affect the development of life-threatening conditions, i.e. acute tetraparesis is classified as an emergency condition. At the prehospital stage, the correct choice of tactics allows, in each specific case of acute tetraparesis, to ensure the timeliness and effectiveness of emergency medical care, safety of transportation to the hospital, continuity of observation and treatment at subsequent stages of patient management.
Today, in the medical literature there are separate publications devoted to this problem, at the same time, fundamental ideas have been accumulated about some diseases and the causes of tetraparesis. Often these patients are given the following diagnoses: “common osteochondrosis of the spine”, “dyscirculatory encephalomyelopathy”, “demyelinating encephalitis (myel)opathy”, “tetraparesis of unknown origin”, “polyneuropathy” and others.
That is why the idea arose of summarizing observations on the diagnosis and treatment of cases of acute tetraparesis in adults and comparing them with modern literary sources. The choice to describe some observations of acute tetraparesis was subjective and determined by our actual diagnostic and treatment capabilities.
Tetraparesis can occur with damage to the peripheral and central nervous systems. Tetraparesis can be a manifestation of acute cerebrovascular accident in the brain stem, often thrombosis of the basilar artery.
Blockage of the main artery is manifested by loss of consciousness, oculomotor disturbances, tetraplegia (paresis), decerebrate rigidity, and hormetonic convulsions. The emergency doctor's tactic is immediate hospitalization in the neurovascular department.
Let us present clinical observations of patients who were taken to the clinic with a preliminary diagnosis of “acute cerebrovascular accident of brainstem localization with tetraparesis.”
Clinical observation No. 1
Patient K.S.V., 42 years old, was taken by the MSP team to the neurological department of the Kharkov City Clinical Hospital on November 09, 2009 with complaints of weakness in the arms and legs, facial distortion, and diplopia.
It is known that he became acutely ill on November 2, 2009, when acute burning pain in the lumbosacral region appeared, he did not seek medical help, regarded it as radiculitis, and used local anti-inflammatory ointments and compresses. On November 4, 2009, numbness appeared in the feet, and soon in the hands, which began to gradually increase. Rheumatoid arthritis. "Common osteochondrosis of the spine." On November 5, 2009, the patient was hospitalized in the hospital, where he developed a left-sided facial distortion and unstable hemodynamics (BP 90/60–170/90 mm Hg). The patient's condition progressively worsened - flaccid tetraparesis began to increase to the point of plegia, diplopia appeared, a brainstem stroke was suspected, the patient was transferred to the neurological department of the Kharkov City Clinical Hospital.
From the life history it is known that the blood pressure figures were in the range of 120–130/80–90 mm Hg. Since 1988 he has suffered from rheumatoid arthritis and is recognized as a disabled person of the 1st group. Chronic cholecystitis.
In somatic status: the skin is clean. Vesicular breathing in the lungs. Heart sounds are muffled and rhythmic. Blood pressure 130/80 mm Hg. Heart rate 78 beats/min. The abdomen is soft and painless. The liver is at the edge of the costal arch. Physiological functions are normal, sphincters are controlled. Deformation of the joints of the hands in the form of ulnar deviation, subatrophy of the interosseous muscles, severe deformation of the knee and ankle joints. The range of motion in all groups of joints is sharply limited, flexion contractures.
In the neurological status: clear consciousness, negative meningeal signs, peripheral paresis of the facial muscles on the left, negative bulbar symptoms, deep flaccid tetraparesis up to 0.5 points. Hypoesthesia of the “gloves” and “socks” type. Tendon areflexia. Diffuse muscle hypotonia. Pathological foot signs are not caused. Does not perform coordination tests. MRI of the brain: no pathology.
Clinical blood test, urine test, blood biochemistry, coagulogram: no significant pathology.
Dynamic ECG: sinus rhythm.
In the above observation, the patient presented with acute demyelinating encephalopolyneuropathy (Guillain-Barré syndrome) with peripheral paresis of the facial nerve on the left, flaccid deep tetraparesis, and oculomotor disorders. The leading symptom is acute flaccid tetraparesis, which began from the distal limbs in an ascending manner; respiratory disorders often develop, requiring the connection of a ventilator, autonomic dysfunction (heart rhythm disturbances, blood pressure lability, postural hypotension), which are the most common cause of death in acute period and require special attention.
Classic variants of Guillain-Barré syndrome are manifested by peripheral paresis in at least two limbs. Cranial nerves are often involved in the process. Often the disease begins with girdling pain in the lower back, cranial nerves are affected, and there is no fever. For many years, the terms Guillain-Barré syndrome and acute inflammatory demyelinating polyradiculoneuropathy (AIDP) were synonymous. According to the Scientific Center of Neurology of the Russian Academy of Medical Sciences, Guillain-Barré syndrome is represented by AIDP in 75% of cases [7].
AIDP often occurs after infection, injury, or surgery. Cases of the disease after a viral infection, infectious hepatitis, HIV have been described.
Currently, the tactics for diagnosing and treating Guillain-Barré syndrome are clearly defined. First of all, every third patient develops bulbar syndrome and respiratory disorders. Therefore, at the slightest suspicion of Guillain-Barré syndrome, the patient should be immediately hospitalized in a neuro intensive care unit and be under close attention during the period of increasing neurological symptoms. “Silent” aspiration, caused by a decrease in the sensitivity of the tracheal mucosa, often complicates the course of the disease [6].
Specific therapy is now clearly defined: plasmapheresis, intravenous immunoglobulin G. According to numerous double-blind, placebo-controlled studies, it was concluded that these approaches are aimed at correcting autoimmune disorders, and it has been proven that patient recovery is accelerated. The use of hormonal pulse therapy remains controversial. However, most neurologists still (for known reasons) use hormone therapy.
After the therapy (solu-medrol, quamatel, omez, trental, fragmin, neurorubin, L-lysine escinate, reamberin, neuromidin, exercise therapy, FTL), the patient’s condition improved: blood pressure stabilized, strength in the paralyzed limbs increased to 3 points, diplopia regressed, peripheral paresis of the facial muscles. On the 21st day, the patient sat independently and stood with support. Further observation allows us to talk about positive dynamics.
To make the task easier, we present a brief algorithm for differential diagnosis between stroke of brainstem localization and Guillain-Barré syndrome (Table 1).
Clinical observation No. 2
Patient L.A.I., 61 years old, was taken to the neurological department of the Kharkov State Clinical Hospital for Children's Hospital on November 10, 2009 by the MSP team. Upon receipt of a complaint of numbness, weakness in the arms, legs, mainly in the legs, urinary incontinence.
It is known that she became acutely ill on 09.11.09, when numbness and weakness appeared in the right limbs, she did not seek medical help, on 10.11.09 numbness, weakness in the left limbs, and sphincter disorders appeared - caused by MSP, which the patient with suspected stroke of the brainstem localization was delivered to the clinic.
From the life history: hypertension, does not constantly control blood pressure numbers, does not take antihypertensive drugs. Hypothyroidism, takes thyroxine 50 mg/day. In 2006, against the background of acute respiratory viral infection, she suffered an ischemic stroke in the territory of the right middle cerebral artery with left-sided pyramidal insufficiency; MRI of the brain revealed foci of demyelination; monitoring of MRI of the brain and observation by a neurologist were recommended. According to the patient, since the summer of 2009 there was weakness in her left leg, she “constantly touched the floor with her toe,” she did not seek medical help, was not observed, was not examined, and was not treated.
In somatic status: the skin is clean. Vesicular breathing in the lungs. Heart sounds are muffled and rhythmic. Blood pressure 160/80 mm Hg. Heart rate 82 beats/min. The abdomen is soft and painless. The liver is at the edge of the costal arch. Sphincter disorders.
Neurological status: clear consciousness, negative meningeal signs, no facial asymmetry, no bulbar symptoms, deep flaccid tetraparesis up to 0.5 points, 0 points in the legs. Tendon areflexia. Diffuse muscle hypotonia, with emphasis in the legs. Babinski's sign on both sides. Does not perform coordination tests.
MRI of the brain (evaluated over time compared to 2006): multiple focal lesions of the white matter of the hemispheres paraventricularly involving the structures of the corpus callosum. Focal white matter lesions are more typical of the morphology of disseminated encephalitis. The ventricular system is not changed. The midline structures are not displaced. The brain stem is without focal changes.
Clinical blood test, urine test, blood biochemistry, coagulogram: no significant pathology. Consulted by a therapist, endocrinologist.
Dynamic ECG: sinus rhythm.
In the given clinical observation, the patient had an exacerbation of chronic disseminated encephalomyelitis with tetraparesis and sphincter disorders.
Disseminated encephalomyelitis is an autoimmune demyelinating disease of the nervous system. Most often, the disease develops against the background of a previous respiratory infection or purulent sinusitis, otitis media. The exact pathogen has not yet been identified. However, in the pathogenesis of the disease, allergic reactions play a leading role, leading to a demyelinating process in the brain and spinal cord [3]. The diagnosis is based on an acute infectious onset and the presence of symptoms of multifocal polysystemic lesions. Disseminated encephalomyelitis should be differentiated from encephalomyelitis with measles, chicken pox, and rubella. The anamnesis data is of primary importance. Differential diagnosis with multiple sclerosis is more complex. In most cases, the final diagnosis is established after long-term observation.
For treatment, methylprednisolone is used intravenously, including with a subsequent transition to prednisolone orally. Uncontrolled trials have found corticotropin and plasmapheresis to be effective.
After the treatment (solu-medrol, trental, L-lysine escinate, ceraxon, neurorubin, neuromidin, reamberin, kvamatel, FTL, exercise therapy), pronounced positive dynamics were observed: strength in the paralyzed limbs was restored to 4.5 points, urination was restored.
Tetraparesis can also develop acutely with damage to the cervical spinal cord (trauma, protrusion of the intervertebral disc).
Clinical observation No. 3
The MSP team delivered patient S.V.A., 56 years old, with complaints of weakness in the arms, legs, and difficulty urinating.
He became acutely ill on January 12, 2009, when he slipped on the stairs and hit the back of his head with a sharp throw of his head back. Within 1.5 hours, the above-described symptoms appeared and increased. Hospitalized in the neurosurgical department. As a result of a comprehensive examination, osteochondrosis of the cervical spine with pronounced degenerative-dystrophic changes at the C3–C4 level, with moderate spastic tetraparesis and dysfunction of the pelvic organs was revealed. Severe spinal canal stenosis.
After the surgical intervention (decompression of the spinal cord from the front with resection of the affected osteochondral structures of the spinal motion segment of the cervical spine), the patient showed positive dynamics. By the 21st day, movements in the paralyzed limbs were restored to mild paresis, mainly in the legs, and the function of the pelvic organs was normalized.
In the example given, tetraparesis is caused by a traumatic disease of the spinal cord at the C3–C4 level. Anamnesis data, which made it possible to reconstruct the mechanism of injury, provided significant assistance in establishing the diagnosis.
Clinical observation No. 4
Patient K.I.B., 47 years old, after hyperextension of the head with a sharp movement towards the telephone receiver, suddenly noticed weakness in the lower extremities and numbness in the arms. Was forced to go to bed. A few hours later, urinary retention occurred. Less than 24 hours later, lower paraplegia and pronounced paresis of the upper limbs developed.
An X-ray of the cervical spine revealed severe osteochondrosis of C5–C7 with narrowing of the intervertebral space and posterior subluxation of C5. For 3 days, traction was performed using a Glisson loop - without effect.
The above observation shows the importance of the vascular factor - spinal cord injury as a result of disc protrusion and C5 dislocation was supplemented by overstretching of the spinal arteries, followed by impaired spinal circulation and acute ischemia. The importance of the vascular factor is also confirmed by the fact that after a two-stage surgical intervention aimed at eliminating compression factors, 2 years after the injury, a practical recovery was noted, he works in his specialty, walks with a stick, and atrophy of the interosseous muscles of the left hand remains.
Acute cervical disc herniation results in acute compression of the anterior spinal artery and cervical spinal cord. With central prolapse, flaccid paresis of the arms with distal atrophies, spastic paraparesis of the legs, and superficial anesthesia (while deep sensitivity is preserved) occur. This is often preceded by pain in the neck and shoulder girdle.
Clinical observation No. 5
Patient K.I.N., 19 years old, was admitted to the gynecological department of the MSP with complaints of pain in the lower abdomen and an increase in body temperature to 37.5 °C. After examination by a gynecologist, the condition was assessed as an exacerbation of bilateral chronic salpingoophoritis. Treatment was prescribed, including cephalosporin antibiotics, fluconazole, anti-inflammatory drugs, and analgesics. The patient complains of severe general weakness, severe abdominal pain radiating to the lower back. She was examined by a surgeon, a repeat ultrasound of the internal organs and pelvic organs was performed, and urolithiasis was suspected. She was consulted by a urologist, who noticed the red color of her urine. The patient's condition began to progressively worsen - numbness and weakness in the arms and legs appeared and began to increase. The patient was transferred to the intensive care unit, where, despite intensive therapy, unstable hemodynamics, respiratory failure were observed, bulbar syndrome appeared, and flaccid tetraparesis worsened. The condition was assessed as encephalopolyneuropathy with tetraparesis, bulbar syndrome, and respiratory failure. Only on the 14th day of hospitalization (!) the thought of porphyria arose. A specific analysis was taken - for porphyrins and coporphyrin (PBG, ALA) in the urine, which was sharply positive. After consultation with a hematologist, specific therapy with Normosang was prescribed, and positive dynamics were observed.
Thus, in the above clinical observation, the patient was diagnosed with porphyritic polyneuropathy with tetraparesis, bulbar syndrome, and respiratory failure.
Acute porphyria can be suspected in any patient presenting to the clinic with unexpected abdominal pain, peripheral neuropathy, or mental disturbances. Moreover, in each individual case, either a whole set of the listed symptoms, or only certain of them, can be observed [4].
Often, patients with acute attacks of porphyria undergo multi-stage ordeals in various departments of clinics, including surgical, urological, gynecological, neurological and psychosomatic. If incorrectly diagnosed and, therefore, treated, acute porphyrias are fatal diseases (mortality rate averages 60%). On the contrary, clear, timely diagnosis and adequate therapy save almost all patients, returning them to a normal, fulfilling life.
All patients, as well as clinicians dealing with the treatment of acute porphyria, must have with them a list of medications that are safe and unsafe for use in acute porphyria. These lists are updated and published annually by the Swedish Porphyria Centre. Today, the most common medications are analgesics, sulfonamide and barbiturate drugs. In our example, the patient received cephalosporin antibiotics, analgesics, and fluconazole from prohibited drugs.
In the early stages of the disease, when subjective sensations dominate over objective signs or when the latter are absent or minimally expressed, hysteria may be the cause of tetraparesis.
From our point of view, the most common cause of diagnostic errors, and therefore the failure to prescribe timely and adequate treatment when acute tetraparesis is detected, is the lack of awareness of doctors about the possible causes of this condition. So, a pre-hospital doctor, supervising a patient with acute tetraparesis - sudden weakness in the arms and legs, sometimes accompanied by respiratory disorders, bulbar disorders in a patient in clear consciousness, must remember the following most common causes of tetraparesis:
- Guillain-Barré syndrome;
- acute encephalomyelitis;
- spinal cord injury;
— acute violation of cerebral circulation of brainstem localization;
- polyneuritis, polyneuropathy;
- hypokalemia;
- hysteria;
— disorders of neuromuscular transmission (myasthenia gravis, botulism).
In this article, using clinical examples, the most common causes of acute tetraparesis in adults are presented, the most common errors (including our own) in the diagnosis and treatment of such patients at the prehospital stage are analyzed, and an attempt is made to give recommendations on how to avoid them.
Due to the extreme importance of the problem, the polymorphism of clinical manifestations of acute tetraparesis, we propose on the pages of the journal to continue the publication of clinical observations by doctors of various specialties, discuss approaches to diagnosis and treatment, and develop modern protocols for the management of such patients, starting from the prehospital stage.
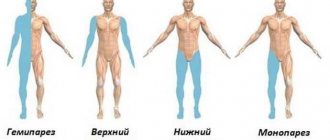
Types of tetraparesis
The disease has several forms:
- Spastic. There is a high tone of the muscles of the limbs and constrained movements due to high intracranial pressure.
- Central. Appears due to injury to two hemispheres, the upper spinal cord or brain stem.
- Reflex. Hypertonicity and hyperreflexia are observed in the arms and legs in the presence of normal muscle strength. Pathological reflexes.
- Lethargic. Weakness and loss of sensitivity appear in the limbs.
- Mixed. This form is characterized by different muscle tone in the limbs—hypotonicity and hypertonicity occur simultaneously.
Some people confuse mixed cerebral palsy and tetraparesis, but these are different diseases. Cerebral palsy is one of the causes of tetraparesis. In this case, the cerebellum is affected in children. They cannot hold their head up, sit, stand or move around without assistance. A child with this diagnosis has delayed mental and intellectual development.
Diagnostics
The cause of tetraparesis is determined by a neurologist. The specialist determines the time and circumstances of the occurrence of the disorder, the rate of development of the symptom, and the presence of other signs. The purpose of a neurological examination is to determine muscle strength, range of active and passive movements, and study reflexes. To clarify the diagnosis, the following procedures are performed:
- Radiography
. X-ray of the skull and spine - basic techniques for traumatic brain and spinal injuries. Confirms dislocations, fractures, displacements of hard structures. - Tomography
. and MRI are prescribed to clarify the data obtained during radiography and identify pathological processes that are not detectable on conventional photographs. Informative for injuries, tumors, hemorrhages, myelopathy, inflammatory lesions. - Myelography.
Contrasting the central spinal canal makes it possible to determine obstacles to the circulation of cerebrospinal fluid. The method is indicated for neoplasms, spinal injuries, herniated intervertebral discs. - Electroneuromyography.
This functional technique makes it possible to assess the conductivity of nerve impulses to skeletal muscles, establish the location of damage, and muscle contractility. - Lumbar puncture.
The procedure is carried out to study the pressure of the cerebrospinal fluid during volumetric processes, subsequent analysis of the cerebrospinal fluid in inflammatory pathologies and subarachnoid hemorrhages. - Lab tests
. Informative for hereditary diseases with metabolic disorders (phenylketonuria, lipoidosis), inflammatory and autoimmune diseases.
Treatment of tetraparesis
Complex measures are needed: a combination of traditional, orthopedic, neurosurgical therapy and rehabilitation. The goal is to reduce spasticity, prevent destruction of the musculoskeletal system and form the correct dynamic stereotype.
For treatment the following are used:
- taking medications;
- reflexology;
- hirudotherapy;
- physiotherapy;
- acupuncture;
- training on simulators;
- massage and physical therapy;
- kinesitherapy;
- hippotherapy.
Prevention
As doctors have long known, the best way to get rid of any disease, including spastic tetraparesis, is to prevent the formation of pathology. Basic preventive measures:
- giving up bad habits - abuse of tobacco and alcohol products;
- avoiding injuries, especially to the spinal column and skull;
- frequent exposure to fresh air - walks in the nearest park in the evenings before bed;
- nutrition correction - predominance in the diet of a large amount of fresh vegetables and fruits, dairy products, as well as cereals;
- drinking at least 1.5–2 liters of clean water per day;
- leading an active life - visiting the fitness room, swimming pool, cycling on weekends;
- timely completion of preventive medical examinations;
- elimination of foci of chronic infections - for example, caries, tonsillitis, sinusitis.
The development of a congenital form of spastic tetraparesis is more difficult to prevent. The expectant mother is recommended to register with an obstetrician-gynecologist as early as possible and undergo the examinations prescribed by him. A pregnant woman should especially carefully monitor her own health - avoid infections, including acute respiratory viral infections or influenza, rubella, and chickenpox. Labor should take place exclusively in the maternity ward, and not at home. This allows you to minimize the risk of injury to the skull and brain with the spine in a newborn child.
If it was not possible to avoid tetraparesis, including its spastic variant, then care must be taken to ensure that the pathology does not progress. Reconsider your lifestyle, take courses in sanatorium-resort healing. Balneotherapy hospitals with mineral waters are well recommended among neurological patients. Courses of acupuncture, laser therapy, and electrical stimulation can improve nervous activity in the limbs and compensate for the manifestations of tetraparesis. The help of relatives and psychological support from friends is of great importance - with a positive, favorable attitude, recovery proceeds faster.
Rehabilitation period
The goal of rehabilitation is to improve the child’s condition and adapt to living conditions. Types of rehabilitation:
- Occupational therapy. Develops motor skills and touch, improves movement and orientation. To do this, play techniques and methods of physical contact are used.
- Classes with a speech therapist. The goal is to develop correct pronunciation and eliminate swallowing problems. It also improves hearing and coordination, and eliminates formed speech disorders.
- Aquatherapy. The child is lowered into water at a temperature of 35 degrees using a special chair. Relaxing spastic areas relieves pain and strengthens muscles. The method has a positive effect on the emotional state.
- Hippotherapy. This is horse riding training and communication with horses. Positively affects motor reflexes, activity and psycho-emotional state.
Forecast
If tetraparesis is congenital and severe mental retardation is observed, it is almost impossible to cure the patient. When there are no signs of intellectual retardation, an integrated approach will help prevent complete damage to the musculoskeletal system and adapt the patient to living conditions.
Treatment for a disease acquired due to a stroke or head injury should begin immediately. Otherwise, the work of the damaged areas of the nervous system and motor system will not be restored. Lack of treatment in older people causes irreversible changes in the spine and general deterioration of the condition. It is important to start therapy in the first 1.5-2 months after a cerebral hemorrhage. Otherwise, the person will remain disabled.
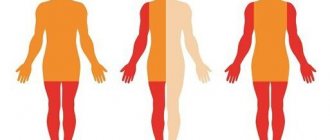
Symptoms and signs
The clinical picture of spastic tetraparesis in children is characterized by pronounced symptoms. The present symptoms will help the specialized doctor determine the stage of the disease and the extent of damage to the small organism.
Spastic tetraparesis in children is accompanied by the following symptoms:
- impairment of motor functions in the legs and arms;
- speech and hearing disorders are also observed;
- vision problems appear;
- the patient's consciousness is impaired;
- the child’s attention and behavior worsens;
- muscle fibers contract involuntarily;
- there is mental retardation;
- the bone structure of the skull develops poorly;
- the functioning of the respiratory organs is impaired;
- the appearance of the lower and upper limbs changes;
- there is a malfunction in the pelvis;
- painful sensations appear in the muscles;
- temporary loss of activity of the lower and upper extremities;
- pathological processes are accompanied by severe shortness of breath;
- the patient is bothered by a cough;
- hiccups appear;
- gait is disturbed;
- general weakness occurs;
- bones are deformed;
- sleep is disturbed, insomnia worries;
- mobility of the hands is limited.
As pathological processes progress, the patient develops problems with intelligence. For small children under one year of age, a characteristic symptom of spastic tetraparesis is cephalic incontinence. The disease often occurs with other concomitant pathologies, which also belong to the group of congenital disorders.
Treatment of tetraparesis in Chelyabinsk
The rehabilitation specialist specializes in recovery and treatment after injuries and strokes. We use a comprehensive method of traditional and modern techniques. We restore lost skills and instill primary ones that the child did not have. We help adapt the patient to living conditions.
To sign up for treatment, send your medical history to our email. After review, we will send a preliminary invoice with a list of procedures, which can be adjusted after an examination by a neurologist. For questions, please contact us by phone.
The medical clinic accepts patients from all regions of the country: Moscow, St. Petersburg, Yekaterinburg, Chelyabinsk, Novosibirsk, Ufa, Kazan and others.
Possible complications and prognosis
Spastic tetraparesis in children and adults develops against the background of various pathological processes. The patient requires emergency medical care to stop the progression of the disease and prevent serious complications.
Without therapy, the patient will face serious consequences:
| Name | Description |
| Spinal deformity | A complication of spastic tetraparesis, which is more often observed in older people. Against the background of pathological processes, a person’s general well-being worsens. The same goes for physical capabilities. |
| Mental retardation | A complication of tetraparesis in children, which occurs against the background of incorrectly selected therapy. The pathological condition is characterized by impaired mental development in the intellectual, cognitive and social spheres. There is a malfunction in the functioning of the brain. |
If spastic tetraparesis develops after a stroke or head injury, treatment must begin immediately in order to have time to restore the affected brain tissue. The victim has 1.5-2 months to stop the progression of pathological changes. Otherwise, rehabilitation will take more time and effort.
For children with congenital spastic tetraparesis, complications include concomitant pathologies that cannot be cured. Correctly selected therapy will improve the quality of life if there are no symptoms of mental retardation.
Spastic tetraparesis cannot be ignored, especially in children, since the disease is serious and can lead to dangerous complications, including disability. Pathology requires a thorough examination to determine the cause of the development of motor dysfunction. Complex treatment is carried out using traditional drugs, physiotherapeutic procedures and, if there are no medical contraindications, folk remedies.