Our clinic specializes in neurology and we perform electroneuromyography. We have competent specialists and modern equipment : an electroneuromyograph, a transcranial magnetic stimulator, equipment for studying evoked potentials, etc. We usually offer electromyography 7 days a week, including Saturday and Sunday. You will receive the ENMG results and a description of them by your doctor. A formal referral is not required.
Electroneuromyography (ENMG) is a study of indicators of electrical activity of nerves and muscles in response to their electrical or magnetic stimulation.
We carry out almost all the main electroneuromyography techniques (ENMG, needle EMG, TMS), incl. in diagnostically difficult and non-standard cases. We perform a range of electromyography techniques that assess the different functions of different motor and sensory nerves. A group of experienced neurologists is at your service, incl. neurologist-immunologist.
- Electromyography of the upper and lower extremities
- Electromyography of the median, radial and ulnar nerves, brachial plexus. ENMG for carpal (carpal tunnel) Guyon's canal syndrome. ENMG brushes
- Electromyography of the lumbosacral plexus, sciatic nerve, tibial and peroneal nerves. Electromyography of the foot
- Spinal cord studies using electroneuromyography
- Electroneuromyography (ENMG) of the facial and trigeminal nerve. Electromyography of the face, facial muscles and masticatory muscles. Electromyography in dentistry
- Decrement test for myasthenia gravis. EMG for myasthenia gravis. Study of neuromuscular transmission
- Stimulation electromyography. Diagnosis of tunnel syndromes, polyneuropathy, mononeuropathy
- Needle myography / Needle electromyography / Needle EMG / Needle ENMG
- Electromyography with transcranial magnetic stimulation
In fact, electroneuromyography (ENMG), electromyography and myography are synonymous names for the same group of diagnostic studies . These are studies of the electrical potentials of nerves and muscles using various methods of stimulation. We will choose the method of stimulation (weak electrical discharge, electromagnetic field, etc.) depending on what problem needs to be found or excluded. It is very important that we understand the essence of your problem and the purpose of the study, so be sure to take with you the results of all previously performed studies: MRI, CT, ENMG, tests, referrals and conclusions of specialists, etc., if they have been performed.
Just doing ENMG is not enough: the results of myography are calculated, interpreted and described by the doctor immediately after the study. You will receive a detailed study protocol with measurement results and a description from the doctor. All calculations and descriptions are already included in the price of ENMG.
Cost of electromyography. The price of myography depends on the research technique. The volume and, accordingly, the price of ENMG in many cases can be reduced by choosing the most suitable research technique, and we use quite a lot of techniques. Therefore , when going to our clinic for electromyography, please take with you the results of previously performed studies, tomograms, tests, consultations, if any. This will help us choose the electromyographic technique that best suits the diagnostic task, and in many cases reduce the cost of electromyography.
Electromyography of the upper and lower extremities
We offer electromyography of the upper and lower extremities, mainly for polyneuropathy of various origins, damage and compression of nerves. ENMG in these cases helps to determine the cause and location of damage, compression or inflammation of the nerves of the arms and legs. Depending on the task of electroneuromyography, we can offer you myography of only the upper or lower extremities or a joint study of the upper and lower girdles (i.e. myography of the upper and lower extremities in one study); the price for electromyography of each belt in this case will be lower.
Stimulation electromyography of the lower extremities
Spinal cord studies using electroneuromyography (ENMG, EMG)
The purpose of electromyography in diseases of the spinal cord is to clarify the diagnosis and cause of the disease, to distinguish diseases of the spinal cord from diseases of the peripheral nerves and muscles with similar symptoms (treatment varies). What other methods are often used when examining the spinal cord?
Our many years of experience suggest that electroneuromyography is one of the most accurate methods in diagnosing diseases such as:
- Amyotrophic lateral sclerosis
- Various myelopathies, i.e. spinal cord entrapment, spinal circulatory disorders
- Herniated discs with entrapment of the spinal cord or its root
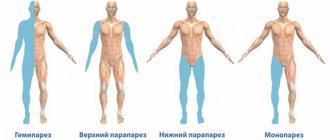
- Paralysis and paresis of unknown origin
- Unexplained walking and sensory disturbances
- Spinocerebellar degenerations are a group of hereditary diseases of the spinal cord and the entire central nervous system
- Neuroinfections with damage to the spinal cord (myelitis, spinal arachnoiditis, encephalomyelitis, radiculitis, neuroradiculopathy) and their consequences
Needle myography in the study of the spinal cord. Needle EMG is perhaps the most informative electromyography technique for studying the spinal cord. Needle myography allows you to evaluate the work of spinal cord motor neurons (motoneurons are the cells that control muscles), the condition of the muscles themselves (differential diagnosis of spinal cord diseases with muscle diseases), peripheral nerves, and even evaluate the effectiveness of the treatment. After performing a needle EMT, in many cases it is possible to accurately say about the condition of the pathways passing through the spinal cord to the muscles, whether the patient has amyotrophic lateral sclerosis, whether there is a prospect of restoring walking, how the peripheral nerves of the arms and legs feel. Read more about needle myography.
Diagnosis of the spinal cord using electroneuromyography (ENMG) using surface electrodes. The simplest method of ENMG - diagnosing diseases of the spinal cord - is the study of electrical potentials of muscles using the application of surface electrodes. Disturbance in the conduction of signals along the spinal cord is immediately reflected in the electrical activity of the muscles and can be recorded using electromyography. We rarely use superficial myography in the study of the spinal cord due to its poor information content. Needle myography and ENMG with transcranial magnetic stimulation help to create a more accurate picture of the condition of the spinal cord.
Electromyography of the spinal cord with transcranial magnetic stimulation (TMS). Transcranial magnetic stimulation (TMS) provides information about the spinal cord's ability to carry stimulation from the brain to the periphery, to the arms and legs. With TMS, the brain is stimulated by a short magnetic pulse, then transforms the magnetic pulse into an electrical pulse, and the electrical pulse, in turn, is recorded and measured by a diagnostic device and analyzed. Basically, the study of the spinal cord with TMS is used in the diagnosis of paralysis, paresis and walking disorders in doubtful and unclear cases. Read more about electromyography with TMS.
Diagnostics of the ascending tracts of the spinal cord (conductors of sensitivity). Somatosensory evoked potentials (SSEPs) are a study of the ascending nerve pathways that transmit signals from sensory receptors in the body through the spinal cord. Learn more about somatosensory evoked potential testing.
Stimulation electromyography during examination of the spinal cord. Stimulation electromyography is a method of examining peripheral nerves that allows one to examine the conductive function of nerves and determine the location of damage or destruction of nerve fibers. This method is excellent for identifying diseases of the peripheral nerves, which must be differentiated from damage to the spinal cord (symptoms may be similar, but treatment may be different). With stimulation ENMG, some parameters of spinal cord function are also indirectly assessed. Learn more about stimulation electromyography.
What is ELECTRONEUROMYOGRAPHY (ENMG)?
Electroneuromyography is a well-established type of functional diagnostics, the main goals of which are:
- Determination of the degree of damage to the human neuromuscular system;
- Determining the nature and topic of damage, as well as the prevalence of the process;
- Determining the degree of development of the pathological process.
HEALTH TESTS On Line
In what cases is it recommended to perform ELECTRONEUROMYOGRAPHY (ENMG)
ENMG is often used to diagnose a wide range of diseases of the peripheral nervous system:
- traumatic injuries of the radial, median, ulnar, greater, peroneal, femoral nerves and other nerves of the peripheral system;
- polyneuropathy of various origins: - lead, chlorophos polyneuropathy - predominant damage to motor fibers of nerves;
- post-diphtheria, otulinic, post-vaccination polyneuropathy;
- plexopathies (damage to the nerve plexus of the anterior branches of the spinal nerves, which are characterized by motor, sensory or trophic disorders);
- neural amyotrophies (Charcot-Marie-Tooth disease), tunnel neuropathies;
- diabetic polyneuropathy;
- polyneuropathy in systemic connective tissue diseases and vasculitis.
- dismetabolic polyneuropathy can occur in the presence of somatic diseases: diabetes mellitus, liver disease, kidney disease, digestive canal, etc.;
- Syringomyelia is a chronic disease of the nervous system accompanied by the formation of voids in the spinal cord.
- spinal osteochondrosis with the presence of radicular syndrome;
In our clinic, when performing ENMG, a qualified doctor can accurately determine not only the site, but also the degree of damage to the nervous system, and also carry out:
- control examination of the effectiveness of the treatment,
- determination of characteristic hereditary disorders,
- determining the statute of limitations for neurological disorders,
- prognosis of the course of the disease,
- early diagnosis of concomitant diseases.
Electroneuromyography (ENMG) is used as the leading method for diagnosing in neurology; in our clinic, the examination is performed by highly qualified specialists with a GUARANTEED result. The use of the ENMG technique is the only method for timely diagnosis of lesions of the roots and nerve plexuses of the spinal cord. The technique makes it possible to identify disturbances in the conductive function of the brain and spinal cord, the condition of peripheral nerves, the presence or consequences of traumatic nerve damage, determine the degree of damage to various nerve structures, and also monitor the process of restoration of motor functions. Based on ENMG examination data, it is possible to make a complex diagnosis of myasthenia gravis, multiple sclerosis and other degenerative diseases of the nervous system.
ENMG of the upper and lower extremities
To view additional materials, select the required section.
ENMG of the upper extremities
enmg upper
ENMG of the upper extremities
Electroneuromyography of the upper extremities involves the study of the brachial plexus, as well as all nerves of the arm: median-ulnar-radial.
ENMG of the upper extremities: brachial plexus.
Our nerves, leaving the cervical and thoracic spine, intertwine and form the brachial plexus of nerve fibers in the clavicle area. Stimulation enmg evaluates the muscle response (contractions of one or another shoulder muscle), the speed of passage and amplitude of the impulse in response to irritation of certain areas of the plexus. As a result, it is possible to reliably determine the possible degree and nature of damage to the nerves of the plexus itself.
ENMG of the upper extremities: brachial plexus, median, radial and ulnar nerve.
The brachial plexus is the origin of both the median, radial, and ulnar nerves. The diagnostic technique for the brachial plexus and the nerves listed below is the same, only the stimulation points and the location of the recording electrode differ.
- The median nerve innervates the muscles of the forearm and some of the flexor muscles of the fingers (thumb).
- The ulnar nerve innervates not only the finger flexors, but also the wrist.
- The radial nerve , passing along the forearm, innervates the extensors of both the fingers and the wrist.
ENMG of the lower extremities
Enmg lower
ENMG of the lower extremities
Electroneuromyography of the lower extremities includes examination of the sciatic, peroneal and tibial nerves. The method of studying the legs is fundamentally not much different from the enmg of the arms: recording electrodes are also applied to certain areas of the legs, the nerves of the legs are also irritated with a weak electrical impulse, then the muscle response (amplitude) and the speed of propagation of the impulse along the nerves of the lower extremities are assessed.
ENMG of the lower extremities: sciatic, peroneal, tibial nerves
The sciatic nerve is the largest nerve in the peripheral nervous system of our body and innervates almost the entire lower limb, and in the hip area it is divided into the tibial and peroneal nerves.
Damage to the mentioned nerves can occur at any point or several places simultaneously. The main task of enmg of the lower extremities is to find all places of possible damage and determine their nature in order to prescribe the correct treatment. It should be added that if, as a result of this examination, it turns out that the condition of the nerves is within acceptable parameters, and dysfunction occurs, then in this case an additional needle emg is usually performed to identify possible radiculopathy.
Read more about this type of research in our article “Myography” .
ENMG IN MEDICINE
- Urology and gynecology. ENMG is a correct assessment of bladder or urethral function disorders, determination of the functional state of the muscles of the urethral and anal sphincters, as well as the nerves that innervate them. Determining the cause of difficulty urinating, suggesting the presence of neoplasms - tumors, assessing the function of the pyramidal tracts when diagnosing sexual disorders and much more.
- Neurosurgery. ENMG – makes it possible to assess the need for surgery, as well as monitor the postoperative recovery period.
- Endocrinology. ENMG - Determination of the degree of damage to muscles and nerves in diseases of the thyroid gland (hypothyroidism and thyrotoxicosis) and diabetes.
- Orthopedics and rehabilitation. ENMG - Study of the motor act and contractile function of muscles, determining the degree of restoration of damaged muscles and nerves, as well as possible contractures and monitoring their development.
Decrement test for myasthenia gravis. EMG for myasthenia gravis. Study of neuromuscular transmission
"Decrement test". The main problem with myasthenia gravis is the inhibition of the transmission of excitation from nerves to muscles. Hence the reversible myasthenic weakness of muscles of various groups. Accordingly, EMG - the diagnosis of myasthenia gravis is based on the study of the transmission of excitation from nerves to muscles. The decrement test is a convenient and fairly reliable option for studying neuromuscular transmission in cases of suspected myasthenia gravis. When conducting the decrement test, we are guided by generally accepted international standards, i.e. We usually study 5 muscles. Each muscle under study is subjected to rhythmic stimulation (i.e., it makes artificially induced contractions), and we record the electrical characteristics of the muscle’s responses to stimuli. Decrement is a gradual decrease in the intensity of muscle responses characteristic of myasthenia gravis in response to its rhythmic stimulation. The presence of a clinically significant decrement usually indicates a disorder of neuromuscular transmission: myasthenia gravis or myasthenic syndrome.
Proserine test or proserine test. Prozerin is a drug, one of the effects of which is a reversible improvement in neuromuscular transmission. In doubtful cases of diagnosing myasthenia gravis, we use prozerin to perform the test. The proserine test (proserine test) is as follows:
- First, we conduct an EMG - a standard Decrement test. Detection of neuromuscular transmission disorders during the decrement test may be an indication for conducting a proserine test.
- We introduce proserin. Prozerin is administered intramuscularly or subcutaneously using a syringe, then absorbed and improves neuromuscular transmission.
- We repeat the decrement test against the background of the action of proserin. If prozerin significantly improves the performance of the decrement test, then a violation of neuromuscular transmission is considered proven.
Symptoms of myasthenia gravis
Most often, myasthenia gravis begins with weakness of the eye muscles: drooping eyelids and/or double vision of objects occurs when trying to focus on them. Later, weakness in the limbs occurs, problems with performing everyday activities due to the inability to raise and hold arms in a certain position, climb stairs or lift objects. In severe cases, there is a worsening of the existing symptoms of myasthenia gravis, which are accompanied by problems with swallowing, pronouncing certain sounds, and the throwing of food into the nose during swallowing.
We recommend that you be examined for myasthenia gravis if such symptoms occur in order to prevent further development of the disease.
Differential diagnosis between myasthenia gravis, paraneoplastic myasthenic syndrome, myopathy, polyneuropathy
Myasthenia gravis is just one possible cause of muscle weakness. The task of establishing the true cause of muscle weakness arises quite often. The usual differential diagnostic series in such cases is:
- Myasthenia gravis, congenital myasthenia;
- Myasthenic syndromes associated with cancer (paraneoplastic myasthenic syndromes), for example, Lambert-Eaton syndrome;
- Myopathy and amyotrophy, i.e. hereditary or acquired (metabolic disorders, the effect of certain medications, etc.) muscle disease with gradual destruction and muscle weakness;
- Polyneuropathy, i.e. of various natures, a decrease in the conduction of excitation along the peripheral nerves themselves;
- Myelopathy, i.e. diseases of the spinal cord of various nature.
In this case, we conduct a series of electromyographic studies using various techniques. We select EMG methods based on the clinical picture of the disease: to identify polyneuropathy, myasthenia gravis, myopathy or myelopathy, respectively. In these cases, we also recommend that you consult a neurologist (neurologist-immunologist) in our clinic and conduct some laboratory tests. Data from tests, examination by a neurologist and EMG results complement and specify each other, helping to accurately determine the cause of muscle weakness and find the correct treatment path.
What laboratory tests can we perform for muscle weakness:
- Antibodies to the acetylcholine receptor (diagnosis of myasthenia gravis);
- Antibodies to skeletal muscles (diagnosis of polymyositis and polymyalgia, autoimmune myopathy);
- Myositis-specific antibodies (diagnosis of polymyositis and polymyalgia);
- Antineuronal antibodies (diagnosis of paraneoplastic neurological diseases);
- Creatine kinase (CK) and lactate dehydrogenase (LDH) are muscle enzymes (markers of muscle tissue destruction in myopathy, polymyositis and other muscle diseases);
- Studies of immune status, autoimmunity, diagnosis of concomitant infections.
Medical indications for diagnostics
- The following patient complaints are the reason for prescribing the procedure:
- numbness of any part of the body;
- increased, pathological nature of sensitivity;
- pain, burning sensation in the limbs, often worsening at night or with movement;
- weakness of legs, arms;
- general weakness, pathologically rapid fatigue;
- unsteadiness of gait;
- inability to move without support;
- difficulty walking up stairs;
- reduction in limb volume.
Stimulation ENMG allows you to identify diseases of the nerves and muscles:
- polyneuropathy of the extremities of various origins (with hypothyroidism, diabetes mellitus, chronic intoxication, poisoning);
- acute inflammatory demyelinating polyneuropathy;
- nerve injuries after bone fractures, wounds;
- tunnel syndrome;
- radiculopathy (lumbago);
- neuropathy of the facial and trigeminal nerves.
Needle ENMG is needed for diagnosis:
- congenital, hereditary, acquired myodystrophies;
- myasthenia gravis;
- myopathies;
- motor neuron diseases;
- amyotrophic lateral sclerosis;
- vibration disease;
- spinal muscular atrophies.
In some cases, both methods are prescribed for differential diagnosis of several diseases. This test is called complex electromyography.
To choose the right technique, a referral for ENMG must contain a preliminary diagnosis, so it is important to consult a neurologist in advance.
The technique gives the doctor the opportunity to identify disorders before the first symptoms appear and begin treatment on time.
Stimulation electromyography. Diagnosis of tunnel syndromes, polyneuropathy, mononeuropathy
Using stimulation electromyography, we can reliably diagnose disturbances in the conduction of impulses along nerves in various diseases, when planning surgical operations on the nerves of the arms and legs.
Stimulation electromyography is a method for studying the peripheral nerves of the arms, legs or face. Stimulation ENMG examines the response of muscles to electrical stimulation of a nerve at different levels, starting from its exit from the spine and further along its course in the arm, leg or facial nerve system.
| Stimulation electromyography of the upper limbs, electroneuromyography (ENMG) of the upper limbs / EMG of the hands |
Thus, we can accurately diagnose damage and disease of nerve fibers and their condition after injury or unsuccessful surgery, when the nerve can become scarred or cut. This study is informative for carpal tunnel syndrome, in which we recommend additionally performing needle electromyography to see if there is a tendency for the nerve to recover, which is important when deciding whether to perform surgery. Thanks to the study, we will be able to see an increase in resistance to the passage of nerve impulses, which can develop as a result of neuroinfections, metabolic disorders due to diabetes mellitus or poisoning with toxic substances, including alcohol.
Difference between ENMG and EMG
Formally, electroneuromyography involves the study of impulse transmission along a nerve fiber, while electromyography is only a recording of electrical activity resulting from muscle contraction. However, in practice, the modern research algorithm practically does not provide for performing EMG in isolation - without studying the speed of impulse transmission along the nerve fiber. ENMG makes it easy to determine the specific “site” of damage to the structures of the peripheral nervous system. Electroneuromyography also allows you to measure the speed of impulse transmission along nerve fibers and assess the functional state of muscles, that is, the ability of muscle tissue to adequately contract in response to a nerve impulse.
Needle myography / Needle electromyography / Needle EMG / Needle ENMG
Needle electromyography (EMG) is one of the best methods for studying nerves and muscles today. Needle EMG is used to diagnose the condition of the muscles themselves, and those nerves that conduct signals from the brain and spinal cord to the muscles. To conduct the study, the doctor inserts a thin sterile needle into the muscle being examined - an electrode (we use disposable needles), with which the electrical muscle potential is measured. Muscle electrical potential deviates from the norm in diseases of the central nervous system and nerves of the upper and lower extremities.
By the bioelectrical activity of the muscle, we can diagnose the presence of muscle diseases (myopathies of various natures), amyotrophic lateral sclerosis, polymyositis and other rheumatic muscle lesions, look at the tendency to restore damaged nerves, determine where the problem is located - at the level of the peripheral nerve or nerve cells of the spinal cord, assess its nature and even determine the presence/absence of an inflammatory process. Needle electromyography plays a very important role in deciding whether it is advisable to perform surgery to restore a peripheral nerve, because With the help of this study, we will understand whether there is reinnervation (restoration of nerve conduction) or whether this nerve is completely lost.
Private methods of conducting ENMG
Electroneuromyography of the lower extremities
Prescribed for suspected polyneuropathy, pathology of the nerves of the lower back, legs, myodystrophy. Often prescribed to determine the cause of restless legs syndrome, loss of sensation or muscle mass after a lower extremity injury. Both methods are used, depending on the intended diagnosis.
The patient is asked to lie down on the couch and relax as much as possible. After this, electrodes are sequentially attached to the muscles of the feet, legs, and thighs. An electroneuromyogram is recorded at rest and then after stimulation.
During the procedure, the doctor may ask the patient to tense any muscle group. In this way, it becomes clear which muscles are impaired and in which fields the sensitivity is changed. This helps determine the location of damage to the nerve endings.
Facial nerve examination
Facial nerve neuropathy can manifest as pain and a feeling of numbness in half of the face. Paresis of the facial muscles on the side of the affected nerve often occurs. At the same time, facial expressions are weakened, the corner of the mouth droops, and the eye cannot be completely closed by the eyelid.
The main technique is stimulation. It is believed that if on the third day of illness the ENMG response is not lower than 50% compared to the healthy side of the face, the prospects for recovery are favorable. Electrodes are installed on the behind-the-ear, frontal, and temporal areas. If necessary, the frontalis muscle, orbicularis oculi and oral muscles are checked using the needle method. In addition, the blink reflex is examined.
Electroneuromyography of the trigeminal nerve
The trigeminal nerve is divided into the orbital, maxillary, and mandibular branches. Therefore, with neuralgia, severe pain appears in these areas of the face. But neuropathy may not manifest itself as pain, but, on the contrary, as a decrease, sometimes loss of sensitivity, muscle activity in the area for which the affected branch is responsible. Myography helps to establish the nature and level of damage. The technique is carried out similarly to ENMG of the facial nerve.
ENMG of the upper extremities
The reason that led to impaired sensitivity or muscle activity of the hands may be located in the neurons of the cerebral cortex, the cervical spinal cord, or at the level of the peripheral nerve endings of the hand. The task of the neurophysiologist conducting the study is to find out this point.
The study can be prescribed for the diagnosis of neuropathies, tunnel syndrome, injuries, inflammation of the median, radial, and ulnar nerves. Both methods are used. The electrodes are alternately placed on the back, then the palmar surfaces of the hand, on the forearm, shoulder, upper arm area, and neck.
To sign up for electroneuromyography at a medical clinic in Veliky Novgorod, contact the reception desk in person or by phone, 8(8162) 90-11-22.
Electromyography with transcranial magnetic stimulation
Transcranial magnetic brain stimulation is a method of measuring the conductivity of the descending nerve pathways that carry impulses from the brain to the arms and legs.
How is electromyography with TMS performed? Using a special magnetic coil, the doctor delivers an impulse to the cerebral cortex (the coil is simply applied to the head). In the brain, the magnetic impulse is converted into an electrical one, which, in turn, travels from the cerebral cortex to the peripheral nerves in the limbs, where it is recorded by the device. Based on the speed of conduction of this impulse and various additional parameters, it is possible to accurately determine whether there is a conduction block at the level of the spinal cord or brain.
Main indications for ENMG with transcranial magnetic stimulation. TMS is mainly used to diagnose disorders of the upper and lower extremities, such as walking. Here it is very important to distinguish muscle paralysis (damage to the nerve innervating the muscle) from muscle disease (damage to the muscle cells themselves from toxic effects, trauma, etc.). We also recommend this research method to determine the cause of bladder dysfunction (urinary retention, loss of urge to urinate), since with the help of transcranial magnetic stimulation it is possible to understand whether the cause of bladder dysfunction is a disturbance in the conduction of impulses along the spinal cord or there is another reason.