Senile dementia is a syndrome that develops after age 65 and gradually progresses. A person’s mental abilities weaken, memory impairment develops, knowledge decreases, skills and activity are lost, judgment is impaired, and emotional impoverishment occurs. At the final stage of the disease, personality degradation occurs.
Neurologists at the Yusupov Hospital use the latest diagnostic methods to detect dementia at an early stage. Doctors at the neurology clinic provide complex therapy aimed at preventing the progression of disease symptoms and personality disintegration. Rehabilitation clinic specialists use innovative methods of rehabilitation therapy.
Causes
Scientists have not yet established the exact cause of the development of senile dementia. The brain processes that cause dementia are not the result of natural aging. Neurologists identify the following causes of senile dementia:
- Compounded heredity - the disease more often develops in people whose relatives suffered from dementia in old age;
- Autoimmune reactions - age-related changes in the body activate autoimmune processes in the human body, which negatively affect nerve cells and destroy the structure of neurons in the brain;
- Concomitant somatic pathology - senile dementia develops more quickly against the background of cerebral atherosclerosis, acute cerebrovascular accident or frequent transient ischemic attacks, diabetes mellitus, arterial hypertension;
- Oncological pathology - space-occupying formations compress the structures of the brain, causing the development of symptoms of dementia:
- Intoxication – smoking and alcohol abuse;
- Suffered traumatic brain injuries;
- Chronic stress.
Diseases that can cause dementia include Alzheimer's disease, Parkinson's disease, acquired immunodeficiency syndrome, Creutzfeldt-Jakob disease (dystrophic disease of the basal ganglia and cerebral cortex, spinal cord), Gaye-Wernicke-Korsakoff syndrome (damage to the hypothalamus and midbrain due to vitamin B1 deficiency). Dementia develops in patients suffering from Pick's disease (a disease of the central nervous system, which is characterized by destruction and atrophy of the cerebral cortex), neurosyphilis, and multiple sclerosis.
Dementia of the brain is a consequence of the disease. Timely examination and treatment of pathology in some cases helps prevent the development of dementia. At the Yusupov Hospital, patients receive a full range of services, including prevention, diagnostics, outpatient care, inpatient treatment and subsequent rehabilitation.
Expert opinion
Author: Polina Yuryevna Vakhromeeva
Neurologist
Dementia is often called “senile dementia,” but this is not always true. Although in the case of senile dementia, the main factor is age. The disease develops very slowly, so in the first stages only the patient himself can notice the changes. It is worth paying attention to such disorders as memory loss, tremors, changes in gait, muscle atrophy, and changes in character.
The average age of life is increasing, and, accordingly, more and more people are suffering from dementia of various types. Almost 50 million people worldwide have been diagnosed with the disease. According to WHO, in 40 years the number of people with dementia will triple!
Dementia is a multi-etiological disease. The most common cause is Alzheimer's disease. Less than 1% of cases of Alzheimer's disease are officially registered, and only 5% of them receive treatment, and this treatment is not at the expense of the state (only 10-15% of expenses are financed).
In our country, the system of care for such patients is just beginning to develop. Currently, there are many drugs that can significantly improve the condition of patients and their quality of life. It is important to remember: the sooner you contact specialists, the higher the likelihood of slowing down the course of the disease.
Corticobasal degeneration*
O.S.Levin, X.Kumru
Corticobasal degeneration (CBD) is a sporadic degenerative disease of the central nervous system, primarily involving the frontoparietal cortex and substantia nigra, less commonly the striatum, ventrolateral thalamus, midbrain nuclei, dentate nuclei of the cerebellum, and inferior olives [5, 10, 28].
The disease is rare, but in recent years it has been diagnosed more often, and the number of cases described in the literature is approaching 100. CBD is part of a group of neurodegenerative diseases characterized by a combination of parkinsonism with other neurological disorders atypical of Parkinson’s disease (“parkinsonism plus”), however, early stage CBD may be difficult to differentiate from Parkinson's disease.
We present a case report of clinically diagnosed CBD.
Patient K., 67 years old. About 2 years ago I noticed gradually increasing awkwardness in my right hand. Then came trembling in the same hand, general slowness of movements, spontaneity, and staggering when walking. A diagnosis of Parkinson's disease was made and Nak (3 tablets per day) and Cyclodol (6 mg/day) were prescribed. Initially, during treatment, the patient’s condition improved, but later it continued to worsen and increasing the dose of Nakoma to 6 tablets per day had no effect.
On examination, mild paresis of upward gaze, moderate dysarthria, reflexes of oral automatism, moderate oligobradykinesia, muscle rigidity (with the “cogwheel” phenomenon), more pronounced in the right arm and axial muscles, revitalization of tendon reflexes, more pronounced on the right. Particular attention is drawn to peculiar motor disturbances in the right hand. She is in a dystonic flexor-adductor position (the shoulder is adducted, and the forearm, hand and fingers are bent), her movements are extremely slow and limited in amplitude, sometimes involuntary movements are noted in her, not similar to ordinary hyperkinesis: the right hand periodically compresses and unclenches, which resembles stereotypies, and the whole arm occasionally slowly rises. In the muscles of this arm, irregular myoclonic twitching is observed, which intensifies with movement. In both hands there is moderate postural and intention tremor, more pronounced on the right.
When moving the more intact left hand, synkinetic mirror movements are sometimes noted in the right hand. The patient experiences significant difficulties when getting up and turning in bed. Moderate dysbasic manifestations are observed in the form of slow initiation of walking, difficulty turning, decreased step length, shuffling gait, and staggering when walking. Acheirokinesis is detected on the right, but there is no flexor posture. In the Romberg position the patient is relatively stable, but reactive postural reflexes are impaired and when pushed into the chest the patient loses balance. On the right are disorders of complex types of deep sensitivity (astereognosis, agraesthesia, impaired sense of discrimination and localization) against the background of moderate impairment of vibration sensitivity and joint-muscular feeling. Cardiovascular tests revealed no signs of autonomic failure.
A neuropsychological study against the background of pronounced neurodynamic disorders, manifested by slowness, aspontaneity, decreased performance, rapid exhaustion, fluctuations of attention, difficulty in entering a task and maintaining its conditions, revealed dynamic aphasia with a pronounced decrease in speech activity, impoverishment of the structure of speech utterances and single paraphasias. A study of praxis in the left hand revealed signs of dynamic apraxia (disautomation of motor skills, disruption of the temporal organization of motor acts, difficulty in learning and retaining motor programs, gross impairment of reciprocal coordination, freezing, motor perseverations) and spatial apraxia (with disruption of constructive praxis and postural praxis) , less pronounced signs of regulatory and kinesthetic apraxia. No violations of gnosis were detected. Memory studies revealed moderate modality-nonspecific defects associated with impaired activity, strength and selectivity of memorization. Intelligence tests revealed a slight decrease in intelligence, mainly due to impaired voluntary regulation and concentration of attention, and impulsivity. In the Wisconsin Card Sorting Test, a low number of completed categories was noted with a significant increase in the number of perseverative responses and errors, which indicated pronounced regulatory violations. The overall assessment of cognitive functions according to the Mini-Mental State Examination is relatively high - 25/30 points. Thus, dysfunction of the frontal and parietal cortex, mainly on the left, with the involvement of the deep parts of the brain and the relative preservation of mnestic and intellectual processes has been established.
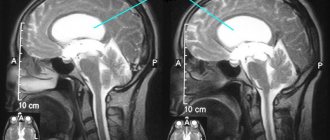
MRI of the head revealed moderate bilateral cerebral atrophy, predominantly in the frontoparietal region with a predominance on the left, manifested by widening of the cortical sulci and lateral ventricles. There were no areas of altered signal intensity or displacement of the midline structures.
Thus, a steadily progressive course with asymmetrical involvement of the cortex and subcortical structures, manifested by a unique set of neurological and neuropsychological symptoms, including levodopa-resistant parkinsonism, focal dystonia, myoclonus, postural and intention tremor, frontal dysbasia and moderate postural instability, the phenomenon of “alien” hand , apraxia and impairment of complex types of deep sensitivity, in the absence of clinical or neuroimaging signs characteristic of other diseases, led us to the conclusion that the patient had CBD.
Subsequently, further progression of the disease was noted with an increase in akinetic-rigid syndrome, gait disturbances, postural disorders, and worsening cognitive defects. The use of parlodel (15 mg/day) and Midantan (300 mg/day) was ineffective. During treatment with clonazepam, myoclonus and intention tremor decreased slightly. After 5 years from the onset, the patient found himself bedridden and absolutely dependent on outside care.
Stages
The clinical picture of senile dementia is determined by the degree of brain damage. In the initial stage of the disease, the patient’s intelligence and ability to work decrease, and the skills of generating ideas and time planning are lost. Patients have difficulty making decisions. They develop distrust of others, paranoia, and difficulties in doing everyday work.
In the second stage of senile dementia, the patient's intellectual abilities disappear. A person loses basic skills in using surrounding objects. He may unintentionally cause harm to himself and his home. At this stage of dementia, the sick person should not be left alone. However, he retains his self-care skills.
At the third stage of senile dementia, a person needs constant supervision. He loses personal hygiene skills and becomes unable to take care of himself.
What is dementia
Mental weakness is a reflection of destructive processes in brain cells.
It can develop as a result of various diseases, injuries or involutionary processes. People with this diagnosis gradually lose acquired knowledge, skills, and memory. Their ability to learn new things disappears. There are more than 35 million people in the world suffering from this pathology. The incidence rate increases, especially after 65 years. It is impossible to cure dementia, but with well-organized treatment it can be significantly slowed down and the level of quality of life improved. The modern level of psychiatry allows patients to maintain working capacity for a long time.
Treatment
The diagnosis of “senile dementia” is made by doctors at the neurology clinic based on the characteristic clinical picture of the disease and computed tomography data. Treatment is performed by neurologists, psychiatrists and rehabilitation specialists. Its goal is to alleviate the patient's condition.
At the Yusupov Hospital, doctors apply international standards of dementia treatment. At the same time, neurologists take an individual approach to choosing a treatment method for each patient. Doctors at the neurology clinic treat the disease that causes senile dementia. Rehabilitation clinic specialists conduct individual and group classes aimed at restoring the patient’s independence skills, provide massage, and conduct physical therapy sessions. Specialists provide psychological support to the patient’s relatives and teach them how to care for the patient.
If rehabilitation is carried out at home, people caring for the patient receive round-the-clock support from specialists at the Yusupov Hospital by telephone. If necessary, the patient can be placed in a comfortable hospice room. To get advice from a neurologist, call the Yusupov Hospital contact center at any time of the day, regardless of the day of the week.
Make an appointment