Postherpetic neuralgia is a complication of herpes zoster, a disease caused by the varicella zoster virus. During an infection, a tingling sensation occurs in a limited area of the skin corresponding to the affected nerve, and after some time a painful rash with blisters appears.
Our expert in this field:
Nasilevsky Pavel Alexandrovich
Oncologist
Call the doctor Reviews about the doctor
When a crust forms on the site of the blisters and they heal, a burning pain occurs that can persist for a long time (for several years, months or a lifetime).
There is no effective treatment for postherpetic neuralgia. Neurologists can only prescribe medications that will help manage pain.
Description and causes of postherpetic pain
Postherpetic pain (or postherpetic neuralgia) occurs as a result of a previous shingles infection caused by the Herpes Zoster virus.
When the virus enters the body for the first time, it causes chickenpox, but after recovery it does not disappear, but circulates in the body for life and can be reactivated when the immune system is weakened (HIV infection, taking immunosuppressants, aging of the body). The virus affects the spinal ganglia and cranial nerves. Clinically, the disease manifests itself as pain along the affected dermatome (an area of skin innervated by an infected nerve), impaired sensitivity, and blistering rashes on an erythematous background. Most often, the pain goes away after the disease subsides, but in some cases it remains persistent.
The pain can be of different types:
- constant, unabating, burning, pulling, pressing,
- "shooting"
- a burning sensation that occurs when you touch the affected area.
Postherpetic neuralgia
Let's start with the fact that this disease is not independent, but manifests itself against the background of herpes zoster, also called herpes zoster.
The occurrence of shingles is caused by the unexpected awakening of the Varicella zoster virus, the causative agent of chickenpox in children. Like all viruses of different types of herpes, this “parasite” does not leave the body of a person who has recovered from the disease. For many years, the patient may not even suspect that he is carrying a time bomb in his nerve cells.
What causes the activation of the virus that causes shingles is still not known exactly. “Waked up” Varicella zoster quickly spreads throughout the nervous system, most often localizing in the intercostal nerve trunks and trigeminal nerve trunks. During this period, the patient feels general malaise, body temperature rises, itching and unpleasant stabbing sensations in the area of the developing rash. Then small pink swellings appear, the place of which, after 3-4 days, will be taken by compactions, quickly turning into bubbles filled with clear liquid. Often the disease is cured quite quickly, in just 3-4 weeks.
If the virus has infected the nerve cells, the person experiences severe pain and some other complications, even with a seemingly complete cure for herpes zoster (shingles). Then we can say with confidence that we are dealing with postherpetic neuralgia.
Causes of postherpetic neuralgia
We also know from biology lessons that our nerve fibers resemble the structure of wires through which electrical impulses run. And they work in exactly the same way, sending impulses to the brain and receiving responses. What happens if the system suddenly fails? That's right, we'll get a short circuit.
The same thing will happen if the Varicella zoster virus damages our nerves. The affected nerve fibers will not be able to perform their functions correctly, which will lead to pain localized in the areas of nerve damage, as well as to impaired sensitivity in the affected areas of the body.
Symptoms
- Different types of pain.
- Itching, numbness of the skin, tingling sensation in the affected area.
- If shingles is localized in the face or head, headache.
- In rare cases, paralysis and weakening of the muscles of the limb are observed.
As a rule, these symptoms appear only in those places that are affected by herpes zoster. In some cases, a patient suffering from postherpetic neuralgia may experience a condition of Allodynia. Allodynia is the occurrence of pain, sometimes even barely tolerable, in response to an irritant that in the normal state of the body would not cause the slightest inconvenience.
Risk factors
Let's say by the way that only people who have had chickenpox can become victims of herpes zoster. However, the risk zone includes several other groups of people in whom the likelihood of developing postherpetic neuralgia increases.
- People over 60 who have had herpes zoster are more likely to suffer from postherpetic neuralgia than younger people.
- Location of the rash. The manifestations of postherpetic neuralgia will be stronger if the rash was in the upper area of the head.
- Disorders of the immune system due to radiation, chemotherapy, acquired immunodeficiency syndrome, etc.
It should be noted that the risk of developing postherpetic neuralgia can be avoided by timely treatment of the disease that precedes this condition, namely herpes zoster. Treatment should begin 2-3 days after the rash appears.
Diagnosis
If there is pain in the area of the skin where the rash appears, or loss of sensitivity in this area, you should immediately consult a doctor. After studying the medical history, a medical examination, and after taking tests, a diagnosis will be made. If the doctor deems it necessary, he can give directions for diagnostic methods such as Ultrasound examination (ultrasound), MRI or another differential diagnostic method.
Prevention
The use of special antiviral drugs helps reduce the risk of herpes zoster, thereby minimizing the possibility of postherpetic neuralgia. To prevent this disease, the following are used:
- The Varivax antiviral vaccine, now widely used to vaccinate children, is also suitable for older age groups who have not had chickenpox. Of course, vaccination does not provide a 100% guarantee that a person will never get shingles or chickenpox, but, in case of infection, it reduces the chance of postherpetic neuralgia, and also helps alleviate the course of a disease such as herpes zoster.
- Zostavax, used against herpes zoster, is prescribed to people over 60 who have had chickenpox but have not gotten shingles. Not recommended for cancer patients undergoing treatment or people with weak immune systems.
- Antiviral drugs, which include drugs such as famciclovir, acyclovir, etc., must be taken within 72 hours after the appearance of the rash. These drugs will not only shorten the duration of the disease, but also reduce the possibility of postherpetic neuralgia.
Treatment
Treatment of this disease includes taking painkillers for oral, local and intramuscular administration.
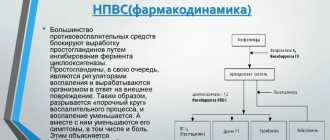
- Conventional analgesics such as Panadol, Acetaminophen and those with anti-inflammatory effects (aspirin, Celebrex, etc.).
- For excruciating pain that conventional analgesics cannot cope with, it is possible to prescribe opioid analgesics. For example: oxycodone, tramadol. But such drugs have serious side effects and must be prescribed with great caution.
- If depression is present, antidepressants (Novopassit, Anafranil) are prescribed to improve well-being and sleep.
- Anticolvusants, such as Neurotin, Topamax, etc., have also shown themselves to be effective in the condition of postherpetic neuralgia.
- Corticosteroid blockades at the affected sites, with drugs such as Dexamethasone, significantly reduce pain.
- Ointments and gels, such as Fastumgel, Capsicam, Diclofenac, containing analgesics or lidocaine, help muffle the symptoms.
An important role in restoring the elasticity of ligaments and muscle tissue is played by physical therapy (physical therapy), in the form of gymnastic exercises and training on simulators.
It would also be a good idea to visit a physiotherapy room and have acupuncture sessions. The latter treatment method is especially effective in reducing pain and restoring neuronal conductivity.
And, although a lot of methods for treating this type of complications have been developed, we should not forget that it is better to take preventive measures in time than to undergo long-term treatment in the future.
Author: K.M.N., Academician of the Russian Academy of Medical Sciences M.A. Bobyr
Diagnosis of pain
The diagnosis of postherpetic neuralgia is made based on the patient’s complaints, history and clinical picture. For confirmation, PCR is performed to detect the DNA of the herpes virus.
Treatment of pain with postherpetic neuralgia is carried out in the following areas:
Pain from postherpetic neuralgia exhausts patients and reduces quality of life. Long-term pain syndrome causes depression, anxiety, decreased concentration, weight loss, and limitation of physical and social activity. It is necessary not to endure pain, but to treat it promptly and effectively.
Symptoms of herpetic neuralgia
Disturbances occur in a limited area of the body, usually on one side, where the nerve trunk affected by the virus passes. The disease is characterized by a combination of three signs:
- Pain. It can be burning, stabbing, aching. Typically lasts 3 months or longer after recovery from shingles.
- Allodynia. This compound word denotes a condition when pain arises from influences that do not lead to it in healthy people. With herpetic neuralgia, pain can occur from light touches to the skin or clothing.
- Itching and numbness. Less common symptoms.
The disease does not pose a great danger, but due to constant pain, over time, a person begins to experience increased fatigue, depression, his appetite decreases, and he cannot sleep properly.
In order to prevent complications, you need to consult a doctor at the first signs of herpes. The earlier a sick person began taking antiviral drugs, the lower the risk that he will be bothered by pain in the future.
Most often, the doctor makes a diagnosis after examining the patient. Additional studies and analyzes are not needed.
Statistics
The number of cases is up to 3 diseases per 1000 people per year. According to statistics, older people are more susceptible to pathology - in people 80 years of age and older, the detection rate is already 10 cases per 1000.
If we consider the percentage distribution of pathology within age groups, we can note that people aged 60–75 years account for half of all cases, those aged 76 years and older account for three quarters.
People aged 60+ are at risk of developing constant pain for a long time - about 10% of patients note that the discomfort persisted for up to six months.
6% of people who have suffered postherpetic neuralgia experience relapses, and 10 years or more may pass from the first to the next case.
Kinds
In medical practice, it is important to subdivide the disease depending on the type of pain and area of the rash.
Based on the duration of the pain syndrome, the following types of neuralgia are distinguished:
- Spicy. Manifestations are observed no more than a month from the moment the vesicles appear.
- Subacute. This name is appropriate when pain persists from one to four months.
- Chronic. The pain syndrome can last for years, then subside, then appear again.
The localization of the rash can be in the chest (from a fifth to half of all cases), head (about 12–20%), neck (up to 11%), much less often - the lower back, extremities.
Symptoms
Symptoms of postherpetic neuralgia typically occur only in the area of the body affected by shingles and include:
- Pain (can be sharp, cutting, throbbing, burning),
- Numbness, tingling, itching
- Headaches if shingles is localized to the head or face
- Rarely, muscle weakness or paralysis if the nerve supplying a particular muscle is damaged.
Sometimes patients experience allodynia. Allodynia is a reaction that is not proportionate to the stimulus (that is, the patient reacts to minor stimuli such as a slight change in temperature or the touch of clothing with severe pain).
Forecast
With timely treatment, the prognosis is favorable - the vast majority of cases end in recovery. When predicting the outcome, it is important to take into account risk factors; the more there are, the higher the likelihood of transition to a chronic form.
The transition to a chronic form can be considered a complication, since intense pain significantly affects the patient’s lifestyle and quality of life.
Other possible complications include changes in skin sensitivity at the site of the rash, the addition of a secondary infection, mycosis,
Diagnosis
If pain occurs after an episode of rashes or sensory disturbances, you should consult a doctor. Diagnosis is based on medical history, examination and laboratory tests (necessary to exclude other diseases). Instrumental diagnostic methods (CT, MRI, EMG, ultrasound) are prescribed only if there is a need for differential diagnosis.
Forecast
Exercise therapy, physiotherapy and drug treatment in most cases help reduce symptoms and restore quality of life. Especially if treatment is carried out in a timely manner.