Author: Druzhinkina V.Yu., neurologist. April, 2021.
Synonyms: PHN, post-zosteric neuralgia. ICD-10 code: G53.0
Postherpetic neuralgia is a complication of herpes, manifested by severe pain that occurs at the site of the rash. It can bother the patient from several weeks to many months. Therapy drugs - anticonvulsants, antidepressants, local anesthetics, antivirals, hormones. In women and elderly patients, a severe course with severe pain is more often observed.
According to most experts, postherpetic neuralgia should be called pain that occurs after herpetic eruptions - vesicles - dry up. They are small bubbles with transparent or slightly cloudy contents; their appearance is often accompanied by itching and scratching.
Photo: fresh herpetic rash and dried rash after scratching
Another part of doctors uses the term PHN to refer to pain that occurs during any period of herpes manifestations, including during or even before the appearance of blisters.
But still, postherpetic neuralgia (“post” means after) is more logical to call a pathology that manifests itself after an exacerbation of herpes, and not before.
The pathology is characterized by severe and prolonged pain, which worsens the quality of life of patients. It is diagnosed quite quickly, since it has a characteristic connection with the manifestations of herpes. Often requires the prescription of anticonvulsants and antidepressants to relieve pain.
Statistics
The number of cases is up to 3 diseases per 1000 people per year. According to statistics, older people are more susceptible to pathology - in people 80 years of age and older, the detection rate is already 10 cases per 1000.
If we consider the percentage distribution of pathology within age groups, we can note that people aged 60–75 years account for half of all cases, those aged 76 years and older account for three quarters.
People aged 60+ are at risk of developing constant pain for a long time - about 10% of patients note that the discomfort persisted for up to six months.
6% of people who have suffered postherpetic neuralgia experience relapses, and 10 years or more may pass from the first to the next case.
Postherpetic trigeminal neuralgia
Gasserian ganglionitis (GGU, synonym: herpes zoster, herpes zoster) is a common infectious disease caused by the Varicella zoster virus, a member of the group of herpes viruses. According to epidemiological studies obtained from the analysis of information on visits to outpatient medical care, up to half a million cases of the disease are registered annually in the United States [1]. The incidence is about 2–3 cases per 1000 people per year [2]. It has been convincingly proven that the incidence of HGU development increases with age, reaching a maximum in old age. Thus, in the population of people over 80 years of age, the frequency reaches 10 cases per 100 thousand population per year, which significantly exceeds the corresponding figure among young people [3].
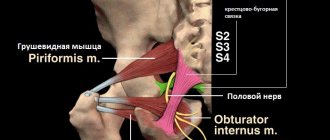
The development of HGU is caused by the reactivation of the Varicella zoster virus, which has persisted in the dorsal horn ganglia of the spinal cord for a long period of time. In relation to the trigeminal nerve, the area where the virus is located is the gasserian ganglion itself. When certain conditions are favorable for the activation (or reactivation) of the virus, the disease develops. It has been established that risk factors for its reactivation are old age, infection in childhood (up to 18 months), a state of immunosuppression, in particular, suppression of cellular immunity of various origins (acquired immunodeficiency, cancer, some systemic diseases, immunosuppressive therapy), intrauterine contact with chickenpox virus.
The Varicella zoster virus can be transmitted from person to person in cases where the individual has not had chickenpox or was not promptly vaccinated for this infection. As a rule, HGU is not prone to recurrence, but it has been established that relapses occur in approximately 6% of patients, and the period from the first to the second episode can be several decades [4]. As clinical experience shows, a repeated episode of HGU may be caused by a newly emerging disease in the patient, the presence of which negatively affects the state and nature of the immune response.
Clinical manifestations
The development of HGU itself is usually preceded by a prodromal period, which is characterized by general malaise, low-grade fever, nausea, and diffuse headache. These manifestations increase and can continue for several days. Often there is the occurrence and subsequent intensification of local pain of a neuropathic nature. Such pains have an unpleasant burning, stabbing tone and are combined with allodynia, hyperesthesia and hyperpathy. The pain may be accompanied by itching and paresthesia. Often it is difficult for the patient to correctly describe his feelings, which forces him to choose unusual wording. Typically, the pain syndrome associated with HGU is localized in the area where rashes subsequently appear and are limited to the area of one or more corresponding dermatomes. However, due to the presence of a neuropathic component of pain, its localization is possible. In the vast majority of cases, these manifestations are unilateral, although in some patients they extend to the opposite half of the body [5].
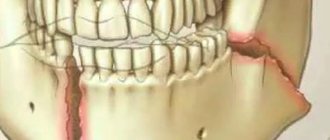
Painful sensations during HGU can be extremely intense, as a result of which the doctor may have a false assumption about the presence of a somatic disease: pleurisy, acute myocardial infarction, renal colic. The occurrence of HGU can cause difficulties in differential diagnosis with dental diseases, damage to the paranasal sinuses, and serve as the basis for dental or otolaryngological intervention.
Against the background of the listed nonspecific symptoms, hyperemia and multiple maculopapular rashes appear, which subsequently acquire the character of vesicular, filled with transparent colorless serous contents. In cases of a favorable course of the disease, the rash can be localized only in a separate part of the dermatome. The appearance of new rashes, which increases over time, is possible over a period of 5–7 days. A few days after the appearance of the first rash, the pustulation stage begins, the contents of the vesicles become cloudy. Subsequently, in the absence of complications (in particular, associated local purulent infection), dry crusts form at the site of the existing rashes, which disappear on their own after 2–3 weeks. Scarring or altered pigmentation may remain in these areas. The disease, as a rule, has a favorable nature, is characterized by a monophasic course and rarely tends to recur.
Diagnosis is sometimes difficult until characteristic rashes appear. Once they occur, making a correct diagnosis usually does not cause difficulties. Confirmation of the diagnosis is possible by performing a polymerase chain reaction, which can detect the DNA of the Varicella zoster virus in the contents of the rash.
Complications
Among the possible complications, it should be noted local infectious lesions caused by infection of damaged skin and deeper tissues with streptococcus or staphylococcus, up to the development of cellulite. With HGU, if the ophthalmic branch of the trigeminal nerve is involved in the pathological process, keratitis may develop, which can lead to severe consequences of corneal damage, including monocular blindness. Rarely there are lesions of herpetic infection of brain tissue (with the development of encephalitis) or its membranes with the occurrence of serous meningitis.
One of the most common complications of HGU caused by herpetic infection Varicella zoster is postherpetic trigeminal neuralgia (PTN). Its pathogenesis is quite complex and includes at least two main mechanisms [4]. Firstly, an increase in the excitability of primary afferents due to damage to peripheral neurons takes part in the development of neuralgia. As a result, increased excitability of nociceptors occurs and, as a result, central sensitization occurs. Clinically, this set of pathophysiological processes is manifested by the occurrence of pain accompanied by allodynia. Secondly, due to the degeneration of nociceptive neurons, deafferentation of the elements of the sensory system located above occurs, causing their hyperactivity. This leads to pain, which, however, is not accompanied by allodynia. According to the authors, the predominance of certain pathophysiological mechanisms is associated with individual characteristics of the pain syndrome and differences in the effectiveness of the therapy. At the same time, a combination of both mechanisms is possible in one patient, which determines the uniqueness of the pain syndrome. PTN has all the clinical manifestations typical of neuropathic pain syndrome. A diagnosis of PTN is possible if the neuropathic pain syndrome persists for at least 30 days after the existing rash has completely healed.
The risk of developing PTN is higher in people over 60 years of age, women, and in the presence of a prodromal period; there is also a dependence of the development of PTN on the prevalence of rashes and the presence of intense pain at the onset of the disease [6]. Age in general is an important independent risk factor for the subsequent development of pain. It has been established that half of patients over the age of 90 years who have had herpes zoster develop PTN [4]. In addition, an unfavorable prognostic factor for its development is the presence of the Varicella zoster virus in the blood. A relatively favorable course of HGU with a less severe pain syndrome, not accompanied by the development of PTN, is much more often observed in young patients and even in the presence of extensive local tissue damage with multiple, often confluent rashes. In the development of PTN, as in the formation of the vast majority of chronic neuropathic pain syndromes, a combination of psychological and social factors plays an extremely important role. Thus, it has been established that the presence of depressive and anxiety disorders preceding Varicella zoster infection, insufficient social adaptation of the patient, disruption of social (including professional) connections, living outside the family, etc. can increase the likelihood of developing pain syndrome.
The clinical course of PTN may vary. It may have a benign course, observed in a significant proportion of patients, which is characterized by significant or complete regression of the pain syndrome over the course of a year. A more severe unfavorable course is observed when the pain syndrome becomes chronic, leading to a sharp decrease in the patient’s quality of life and, in some cases, to his disability [7]. Serious and fairly common complications of Varicella zoster infection are the occurrence of severe pain, which increases with age, as well as damage to the soft tissues of the face by the virus itself or an associated bacterial infection. The most dangerous is the involvement of the sclera of the eyeball in the pathological process, which can lead to keratitis and complete monocular blindness. Infectious damage to the brain itself is relatively rare, and damage to the spinal cord is less common. It is believed that in more than 5% of elderly patients, intense pain persists for at least 12 months [4]. Features of the course of the disease may be associated with differences in the pathogenesis of pain, the direction and intensity of the body's compensatory reactions, as well as the effectiveness and adequacy of the therapy, in particular, its timely initiation.
In some cases, along with the development of PTN, motor disorders are observed in the form of peripheral paresis of the cranial nerves (most often the facial nerve) [8]. This form of herpes infection is described under the name Ramsay–Hunt syndrome [9]. There is currently no convincing data on the prognostic significance of emerging movement disorders in relation to the intensity and duration of pain.
Treatment
The most effective way to treat patients with HGU caused by the Varicella zoster virus is the timely use of antiviral drugs. Currently, the high effectiveness of valacyclovir (Valogard) in the treatment of patients with herpes zoster has been convincingly demonstrated. Of practical interest is the recommendation for use in accordance with the “50-50-50” rule [5]. The authors of this rule demonstrated that the maximum effectiveness of antiviral therapy is observed when it is started no later than 50 hours from the moment the first rash appears, when it is prescribed to patients over the age of 50 years and in the presence of at least 50 elements of the rash. If this rule is observed, it is possible to reduce the healing time of existing skin lesions, as well as reduce the risk of developing PTN [10]. Studies on the effectiveness of therapy for patients with HGU have shown that, regardless of the criteria used to evaluate the effectiveness of therapy (the likelihood of developing pain, the timing of its onset, the intensity of pain), the timely prescription of valacyclovir and the correct choice of indications for its use are of fundamental importance. It has been shown that a delay in the start of treatment, a late start of initial antiviral therapy (more than 72 hours after the appearance of the first rash) can provide only a slight reduction in healing time, without causing a reduction in the risk of developing PTN [11]. On the other hand, the use of antiviral drugs in the case of a small number of rashes (less than 50) does not significantly affect the course of the disease and is not associated with a significant reduction in the likelihood of developing neuropathic pain syndrome. If the “50-50-50” rule is not followed, i.e., the selection of indications for prescribing valacyclovir is not carried out entirely correctly, the effectiveness of therapy turns out to be relatively low. Thus, the results of a systematic review examining the results of antiviral therapy for HGU could not confirm its effectiveness in preventing the development of neuralgia 4 and 6 months after the onset of rashes [12]. The results obtained once again demonstrate the need for correct patient selection to achieve the desired effect and the importance of timely initiation of treatment.
To achieve a therapeutic effect, including reducing the risk of developing PTN, valacyclovir is prescribed at a dose of 500 mg 2 times a day for 5 days. Release form: film-coated tablets, 500 mg, 6 or 10 pcs.; 7 blisters (6 tablets each) or 1 blister (10 tablets each). Along with parenteral administration of the drug, which ensures sufficient concentration in the blood, it is possible to use local dosage forms of antiviral drugs (gels, ointments, creams), however, it should be taken into account that achieving a therapeutic effect is possible only with systemic administration of the drug in adequate daily dosages for a sufficient period of time treatment. The drug is well tolerated and can be used simultaneously with other drugs. The currently available information on the effectiveness of the use of valacyclovir (Valogard) in patients with herpes zoster allows us to recommend its widespread use in this group of patients. Timely initiation of treatment and proper selection of patients for drug administration can increase the effectiveness of therapy.
The simultaneous administration of glucocorticoids is proposed as a means of potentiating the therapeutic effects of valacyclovir. Information has been obtained that combination therapy can significantly reduce the intensity of pain in the acute stage of the disease [13]. Information about the possibility of reducing the risk of PTN formation due to the use of glucocorticoids turned out to be relatively less convincing. The authors of these studies showed that the use of glucocorticoids is associated with an increased risk of unwanted side effects, such as exacerbation of gastric ulcers, hyperglycemia; addition of local infectious and inflammatory processes. The risk of this kind of complications increases with age, in the presence of risk factors for damage to internal organs due to the use of corticosteroids, in patients with diabetes mellitus, gastric ulcer, etc. In this regard, combination therapy with the use of corticosteroids requires comprehensive consideration of its possible positive effect and associated with treatment of the risk of side effects due to the individual patient's condition. To relieve local pain that is not neuropathic in nature, it is possible to use non-steroidal anti-inflammatory drugs, in particular meloxicam (Liberum), which is well tolerated and sufficiently effective. However, its prescription is poorly justified in patients with true PTN.
If the patient has persistent PTN, treatment requires different approaches. According to numerous recommendations adopted in various countries, in this situation, drugs that have a central or peripheral analgesic effect should be used. For a long time, such patients have been using tricyclic antidepressants (amitriptyline, nortriptyline), which are characterized by fairly high analgesic efficacy. Unfortunately, despite the high probability of complete relief or reduction in the intensity of pain when they are used, the widespread use of these drugs is limited due to the frequent occurrence of unwanted side effects, especially when they are prescribed in high dosages. Achieving an analgesic effect while reducing the risk of side effects is possible by prescribing antidepressants that have the ability to inhibit the reuptake of both serotonin and norepinephrine. It is important that the analgesic effect of antidepressants in PTN and other neuropathic pain syndromes is realized without a direct connection with the antidepressant effect [14].
Another of the main directions of treatment for patients with PTN is the prescription of antiepileptic drugs, in particular carbamazepine. In recent years, new drugs have become widespread, the pharmacological effects of which are due to interaction with the receptors of gamma-aminobutyric acid, the main inhibitory neurotransmitter in the central nervous system (gabapentin, pregabalin). With analgesic activity almost comparable to carbamazepine, they are characterized by significantly better tolerability and fewer significant unwanted side effects.
Of undoubted practical interest is the possibility of using local forms of drugs. Thus, it has been shown that the local use of lidocaine preparations, in particular in the form of patches, may be advisable in the presence of pain accompanied by allodynia. There is information about the possible effectiveness of capsaicin in patients with PTN, although it is not approved in all countries for use in pain syndromes in the face and head [15]. Widespread use of the drug is limited by not always satisfactory tolerability of therapy.
In order to reduce the drug load on the body and shorten the duration of therapy, combination therapy is used to treat pain syndromes of various origins. The use of B vitamins, which are of exceptional importance for the functioning of nervous tissue, is considered as drugs that increase the effectiveness of treatment for patients with PTN. As evidenced by data obtained from experimental and clinical studies, vitamins take part in various biochemical reactions occurring in neurons and glial cells and are necessary for their normal functioning. Thiamine acts as a coenzyme in the oxidative decarboxylation reactions of alpha-ketoglutaric and pyruvic acids, and takes part in the processes of protein synthesis and regeneration of damaged nervous tissue [16]. Pyridoxine is a coenzyme in the reactions of decarboxylation and transamination of amino acids in various tissues, including the peripheral nervous system. Its effectiveness has been shown in patients with various forms of damage to the peripheral nervous system, in particular, with polyneuropathies of various origins, spondylogenic dorsopathies, and discogenic radiculopathies. Cyanocobalamin and other derivatives of vitamin B12 take part in the processes of energy supply to cells; it is involved in protein synthesis and some other mechanisms of their functioning [17]. Important clinical effects of the use of B vitamins are both the activation of the processes of regeneration of nervous tissue in conditions of damage, and its own analgesic effect.
The combination of these properties determines the widespread use of B vitamins in patients with pain syndromes.
It has been shown that their simultaneous use with analgesics and non-steroidal anti-inflammatory drugs reduces treatment time and reduces the need for pain relief in patients with musculoskeletal pain syndromes [18]. This kind of combination therapy provides an increase in the duration of the remission period in patients with both isolated dorsopathy and compressive radiculopathy [19]. Similar results were obtained in other clinical studies performed in accordance with the requirements of evidence-based medicine, in which various analgesic drugs were prescribed [20, 21]. The advantages of combination therapy, including B vitamins, compared to monotherapy with analgesic drugs are noted in the European guidelines for the management of patients with chronic nonspecific musculoskeletal lumbar pain [22]. There are clinical and experimental data on the effectiveness of vitamin therapy in patients with damage to sensory cranial nerves and their branches by neuropathic pain syndrome [23, 24]. The new drug Vitaxon, containing a complex of B vitamins, deserves special attention. The solution for parenteral administration includes thiamine hydrochloride and pyridoxine hydrochloride (100 mg each), as well as 1.0 mg of cyanocobalamin. Ampoules for intramuscular injections of 2 ml are packaged in packages of 5 or 10 pieces. Vitaxon injection solution is used for the treatment of neuritis, neuralgia, alcoholic and diabetic polyneuropathy, myalgia, relief of radicular syndrome, and herpes zoster. The drug can be used in the complex treatment of various pain syndromes, complex therapy of facial nerve paralysis, treatment of retrobulbar neuritis, including PTN. Vitaxon solution is administered intramuscularly, following standard recommendations for intramuscular injections. For acute pain and in severe clinical cases, the recommended dose is 2 ml of solution, injected intramuscularly once a day. In mild forms of pathology or after pain has decreased, the drug intake can be reduced to 2 ml, injected intramuscularly with a break of 1 day. The standard course of injection therapy is 1 month.
Causes and risk factors
The etiological factor leading to the development of postherpetic neuralgia is the herpes virus – varicellazoster. The mechanism of pain is not fully known. One theory is the occurrence of an immune-mediated reaction, as a result of which the body reacts aggressively to the cells of its own body, perceiving them as foreign agents.
As a result, irritation and swelling of nerve fibers occur, and the functioning of pain receptors changes. All this gives rise to characteristic attacks of neuropathic pain - they can easily be described with a capacious, sonorous word, for example, “burning”, “stabbing”. This is characteristic of nerve damage.
A well-established risk factor for the development of postherpetic neuralgia is advanced age. In such patients, the pain syndrome is observed even before the appearance of the rash, and is so pronounced that the doctor has to rule out a heart attack, renal colic, or an attack of cholelithiasis.
Immunodeficiency, diabetes mellitus, cancer, a large area of herpetic rash, and female gender also increase the risk of postherpetic neuralgia.
How is the problem diagnosed?
Diagnosis of PHN is complicated by the large time gap between the development of the acute phase of herpes zoster with skin rashes and the appearance of neurological complications, which can make themselves felt 6 months after the onset of shingles.
The localization of pain determines which doctor the patient will see. As a rule, with complaints of discomfort in the neck and back, the patient consults a neurologist.
The main task of the doctor is to differentiate PHN from other diseases of a non-infectious nature:
- Visit to the doctor. If the pain is localized in any part of the spine, then the diagnosis will be carried out by a neurologist. If the facial nerves are damaged, the patient can contact both an otolaryngologist and a dentist.
- The doctor takes an anamnesis (finds out the patient’s medical history). Here it is important to find out the duration of the manifestation of pain symptoms, as well as the fact of having chickenpox or shingles in the distant and not so past.
- The doctor conducts diagnostics in order to differentiate PHN from other diseases. For this purpose, instrumental research methods (MRI, CT) are used. They help confirm or refute other diagnoses with similar symptoms (hernia, osteochondrosis, spondylitis, etc.)
- Laboratory differential diagnosis includes blood tests that will help exclude rheumatoid arthritis, diabetes mellitus and a number of other diseases that cause symptoms similar to PHN (polyneuropathy in diabetes, common pain in rheumatism, etc.)
- To confirm the diagnosis of postherpetic neuralgia, the doctor evaluates the totality of symptoms in the pain area and conducts laboratory tests to determine antibodies to Herpes zoster (in order to find out whether the patient has ever had this virus). In the absence of rashes, postherpetic neuralgia can be confirmed by immunohistochemical analysis and taking a biopsy from the area affected by pain.
Kinds
In medical practice, it is important to subdivide the disease depending on the type of pain and area of the rash.
Based on the duration of the pain syndrome, the following types of neuralgia are distinguished:
- Spicy. Manifestations are observed no more than a month from the moment the vesicles appear.
- Subacute. This name is appropriate when pain persists from one to four months.
- Chronic. The pain syndrome can last for years, then subside, then appear again.
The localization of the rash can be in the chest (from a fifth to half of all cases), head (about 12–20%), neck (up to 11%), much less often - the lower back, extremities.
Symptoms
The main manifestation of postherpetic neuralgia is pain. It is characterized as burning, pronounced, sharp, shooting, stabbing, and may be accompanied by unpleasant itching. Symptoms develop quickly - pain with postherpetic neuralgia appears immediately, their intensity increases over 2-5 days.
The first signs of the disease are pain in the area of the rash, aggravated by touch (including clothing) under any influence. Types of pain syndrome:
- Constant. A feeling of dull pain coming from the depths, often with stabbing, burning shades.
- Periodic. Shoots, stabs, burns. The attacks occur abruptly, comparable to an electric shock.
- Allodynic. It is based on a change in perception, when any impact is perceived by the nerve fibers as causing pain.
Manifestations of the disease differ in the strength of the pain syndrome. Symptoms of certain types of PHN:
- Postherpetic intercostal neuralgia is a common variant of the disease that occurs after the manifestations of herpes zoster have subsided. Pain syndrome is noted along the ribs, i.e. where the intercostal nerves go.
Photo: one of the common variants of localization of the rash with herpes zoster
- Postherpetic trigeminal neuralgia, or trigeminal neuralgia, is quite rare. It is characterized by the occurrence of severe pain on the face - in the area of the eyes, nose, cheeks, lips.
- Postherpetic neuralgia of the sciatic nerve - unpleasant sensations spread along the course of the nerve of the same name, i.e. from the back of the thigh to the heel.
- Postherpetic neuralgia in the oral cavity occurs very rarely and is associated with rashes after chickenpox.
What can be confused with
In situations where pain occurs before the appearance of vesicles, or the disease occurs without a rash, postherpetic neuralgia can be mistaken for manifestations of other diseases.
Differential diagnosis:
- An attack of renal colic - in the case of postherpetic neuralgia, there are no changes in the general blood test and during ultrasound of the kidneys.
- Gallstone disease – it is not possible to see stones or sand in the gallbladder, liver, or its ducts on ultrasound.
- Myocardial infarction - no signs of ischemia on the ECG. Difficulties with this point may arise in older patients who already have chronic myocardial ischemia, or when hypoxia (lack of oxygen) develops in the heart muscle against the background of severe pain. In such cases, a dynamic ECG is required - 20-40 minutes after the first examination with subsequent comparison.
- Intercostal neuralgia - it is difficult to tell the difference here, especially at the beginning of the development of the disease, but with intercostal neuralgia there is a clear increase in pain when inhaling, when coughing, sneezing, and sudden movements of the body. With PHN, pain usually does not significantly increase with such actions.
Etiology of development
Postherpetic neuralgia develops as a complication of herpes zoster (or “shingles”).
The disease is one of the variants of the clinical manifestation of the chickenpox virus (Varicella zoster). It is he who provokes the development of chickenpox in childhood.
After a child has had it at an early age, the virus can remain in the body in a latent form for many years.
The main areas of colonization are the nerves of the thoracic and lumbar regions, as well as the trigeminal nerve (on the face) . Shingles appears in the form of a blistering rash and is accompanied by an increase in temperature.
The disease goes through three stages of development:
- Initial (lasts 2-3 days, preceding the rash. May be accompanied by acute skin pain and itching).
- Rash stage (lasts about two weeks: from the appearance of blisters to their breaking and drying).
- Pain stage (develops after the rash has healed; it is this that can subsequently develop into postherpetic neuralgia).
According to statistics, about 20% of patients suffer from complications of the disease in the form of postherpetic neuralgia.
The virus affects the peripheral nervous system and leads to chronic pain that does not go away for months. The diagnosis is made when pain persists for 4 months after the onset of the disease . At the same time, a number of experts claim that the disease can be called chronic if after 2-3 weeks a new rash does not appear and the pain does not subside.
Survey
If you suspect postherpetic neuralgia, it is advisable to consult a neurologist.
The diagnosis is not difficult in cases where pain occurs after the appearance or extinction of vesicles. The difficulty is presented by patients whose pain has developed before the skin manifestations of herpes. During the examination, the neurologist (in his absence, the therapist) notes the following abnormalities in the patient:
- hyperalgesia - excessive pain with slight impact - pressure, gathering the skin into a fold;
- allodynia – the appearance of pain from contact with irritants that normally do not cause it (touching clothes, patting with the palm of the hand);
- hypoesthesia - a decrease in all types of sensitivity along the nerve fiber.
Laboratory and instrumental studies are prescribed quite rarely. To confirm the GWP, 2 main studies are carried out:
- Tzanck test - scraping from a vesicle, placing the contents on a glass slide, followed by staining. In this case, multinucleated giant cells are revealed.
- Blood test for antibodies to the pathogen - HerpesZoster.
A general blood test, indicating the viral nature of the disease, and a biochemical study, which determines an increase in acute-phase inflammatory proteins, are less informative.
Herpes virus infection does not always manifest as rashes. In such cases, in order to exclude other neurological pathologies, the patient may be referred for ENMG - a study that allows identifying disturbances in conduction along nerve fibers, a change in response when exposed to a stimulus.
Symptoms and nature of pain after shingles
The peculiarity of postherpetic manifestations is the expansion of the affected area . Places where there were no rashes may begin to hurt.
The virus can infect different parts of the peripheral nervous system (the nerve itself, its root, etc.). Hence the different types of pain that patients complain about.
There are 3 groups:
- Constant pain (it can be described as dull, burning, pressing).
- Sudden (it is described as shooting, stabbing, sharp).
- Pain from non-painful stimuli (can occur from light touch, contact with clothing, etc.).
What do patients complain about?
For PHN there is no single characteristic of pain syndrome . For some it may be permanent, while for others it may appear periodically. Its intensity also varies greatly: from mild to unbearable.
Some patients complain of severe skin itching , which persists after the disease passes from the acute to the chronic stage. In some cases, complete loss of tactile and pain sensitivity is possible.
Patients with PHN often report chronic fatigue, lack of appetite, weight loss, and depression. Statistics show that more than 50% of patients have sleep disorders. Such manifestations seriously complicate a person’s life, reducing its quality up to the point of social disadaptation.
For example, increased sensitivity to even light contact with the body makes everyday activities difficult: patients cannot wash dishes, take a bath, get a haircut, etc.).
Find out more about the types and forms of neuralgia:
- inflammation of the sciatic and external cutaneous nerve of the thigh;
- glossopharyngeal and pterygopalatine node;
- damage to the pelvic, occipital and brachial nerves.
Treatment
Postherpetic neuralgia is treated by a neurologist, or, in his absence, by a therapist. At the 9th Congress of the EFNS (European Federation of Neurological Societies), recommendations for the treatment of post-herpetic, neuropathic peripheral and diabetic pain were adopted, then Russian protocols for the treatment of herpes and PHN were developed.
Main drugs:
- Anticonvulsants are first-line drugs because they have the ability to reduce neuropathic pain. The best option is gabapentin. Lamotrigine and valproate are also used. The often previously prescribed carbamazepine has not confirmed its effectiveness in clinical trials, and also has a different set of side effects.
- Local impact. For analgesic and distracting purposes, ointments and gels are used, including those with anesthesin, lidocaine, and capsaicin.
- Antidepressants. These are fluoxetine, paroxetine, amitriptyline. Prescribed strictly by the attending physician, available with a prescription.
- NMDA receptor blockers. To relieve acute pain, the drug of choice is amantadine sulfate.
- Glucocorticosteroids (for example, prednisolone) are prescribed to inhibit the inflammatory process and reduce swelling around the nerve.
- GABAergic receptor agonists. Baclofen is used. It blocks the transmission of pain impulses at the level of the spinal cord, thereby removing or reducing discomfort.
- Antiviral - act on the herpes virus circulating in the blood, but do not reach pathogens sleeping in the nerve ganglia of the spinal cord. Prescribed in the acute period or during exacerbation. Valciclovir (a relatively new drug in the treatment of postherpetic neuralgia), penciclovir, acyclovir, famciclovir, and ganciclovir are used.
- As an alternative therapy for severe pain, opiates, tramadol, and, less commonly, anti-inflammatory drugs are prescribed.
Postherpetic neuralgia can be cured, especially if treated early. But in some situations, even with therapy, the pathology becomes chronic.
Duration of treatment:
- anticonvulsants, antidepressants - the timing is determined by the duration of the pain syndrome;
- immunostimulants - depending on the regimen, which is individual for each drug, the terms range from 5 days to 2 months;
- antiviral drugs - up to 3 weeks, also depends on the specific drug.
Over time, postherpetic neuralgia may go away on its own, but in most cases it is difficult to endure the pain syndrome, so patients seek medical help.
The approximate duration of treatment is determined by the duration of the pain syndrome, ranging from a month or more. Recovery and rehabilitation takes up to six months; in elderly patients, these periods are often prolonged, which is associated with a decrease in the overall capabilities of the body.
Physiotherapy for postherpetic neuralgia, together with basic therapy, helps relieve pain. A magnetic field with an intensity of 1.6 Tesla and a frequency of 1 Hz is prescribed, and the healed elements are irradiated with a laser.
They are not included in the treatment recommendations, but additional acupuncture, vibration massage, blockade with glucocorticosteroids, and botulinum toxin may be prescribed.
How to treat pain after herpes?
Treatment methods for postherpetic neuralgia (after shingles) in young and elderly people will depend on the stage of the disease and the severity of complications.
Antiviral therapy
Antiviral therapy is used to treat the acute phase of herpes. The use of Acyclovir and its analogues is effective .
The essence of the drug’s action is its ability to integrate into the DNA chain of viral particles in order to interrupt the pathological process and stop the reproduction of the virus.
Drug treatment
To treat complications in the form of PHN, medications are prescribed: tricyclic antidepressants (amitriptyline, nortriptyline) and antiepileptic drugs, in particular Finlepsin (Carbamazepine).
Pain relieving patches
The use of local (local) painkillers is quite effective.
For example, they actively use patches that are glued to the affected area ; they contain an anesthetic, in particular Lidocaine.
Another effective patch is one with a high content of capsaicin. The active substance blocks pain receptors in the skin. Using this method can relieve pain for up to 3 months .
Ointments
Another option for local anesthesia is the use of ointments. In particular, capsaicin is also available in this form. Ointments containing non-steroidal anti-inflammatory drugs (diclofenac) are also used.
Epidural blocks
Epidural blockades are used to relieve pain. This is an effective method of pain relief for various pathologies of the spine.
Anesthetics and steroid hormones are injected into the epidural space, which leads to loss of sensitivity in the area of influence.
Traditional recipes for home use
To relieve the symptoms of the disease, you can use traditional recipes:
Rubbing with garlic tincture . 1 tablespoon of garlic is infused with 500 ml of vodka for several days. The resulting tincture is rubbed on the sore spot several times a day.- Radish compresses . You need to cut a hole and fill it with honey. Leave in a warm place for a couple of days. The resulting liquid is applied to the affected area.
- Baths with pine infusion . A decoction is prepared from young pine cones and shoots. Baths are recommended to be used 2-3 times a week in the evenings before bed.
Radiofrequency nerve destruction
Radical methods are also used to combat the consequences of complications. Destruction is a modern technology for treating various types of neuralgia . Its essence is to destroy the nerve by heating it with electric current.
The operation is minimally invasive (gentle) and does not require deep intervention in the body tissues. The current is transmitted through a needle, which is inserted directly into the nerve.
Forecast
With timely treatment, the prognosis is favorable - the vast majority of cases end in recovery. When predicting the outcome, it is important to take into account risk factors; the more there are, the higher the likelihood of transition to a chronic form.
The transition to a chronic form can be considered a complication, since intense pain significantly affects the patient’s lifestyle and quality of life.
Other possible complications include changes in skin sensitivity at the site of the rash, the addition of a secondary infection, mycosis,