Meningitis in children is an acute infectious disease in which inflammation of the membranes of the brain and spinal cord develops. Children's meningitis is severe. If antimicrobial therapy is not started in a timely manner or is inadequate, severe complications develop in children with meningitis. The Yusupov Hospital has all the conditions for the treatment of meningitis:
- the wards are equipped with forced-air ventilation and air conditioning;
- patients are provided with individual personal hygiene products and dietary nutrition;
- Patients are examined using devices from leading global manufacturers and modern laboratory diagnostic methods;
- Doctors use the latest generation antibacterial and antiviral drugs, which are highly effective and have minimal side effects.
Severe cases of meningitis are discussed at a meeting of the expert council with the participation of candidates and doctors of medical sciences. Leading specialists in the field of treatment of infectious diseases of the central nervous system make a collegial decision regarding the management of patients with severe meningitis. The clinic accepts patients aged 18+.
Providing first aid to a child
The first thing the baby’s parents must do is call an ambulance.
There is no need to put off calling, much less try to treat your child on your own! Remember: the faster quality, qualified assistance is provided, the greater the child’s chances of recovery.
Before the arrival of specialists, it is necessary to provide the little patient with peace, silence and darkness. You should not let your child get up.
The same technique should be carried out in the case when a small patient experiences convulsions. This will protect the baby during an attack from the tongue retracting and blocking the respiratory tract.
What can be the consequences of meningitis suffered in childhood?
HomeQuestion answer What can be the consequences of meningitis suffered in childhood
Question: What can be the consequences of meningitis suffered in childhood?
Answer: The consequences of meningitis in a child depend on the age at which it occurred, what the cause was, and how severe the disease was. Self-medication also has a negative impact on future health. After all, parents could decide that it was a common cold and treat the child themselves. At the same time, an illness developed, the consequences of which would negatively affect the future well-being of the baby. Therefore, adequate and timely therapy will help get rid of severe consequences.
But the consequences of meningitis suffered in childhood are not always so dangerous. For example, if we are talking about its viral variety, complications are most often not observed. If you follow all medical recommendations, you will be able to fully recover after 3-5 years. During this period, you will have to take medications and visit a neurologist.
Statistics say that after 5-7 years, the consequences of meningitis suffered in childhood disappear, and such children are not at all different from their peers.
As for having serous meningitis in childhood, there are consequences from it. They are expressed through periodic pain in the head, which can affect the learning process. It is also possible to experience anxiety for no reason.
As for the infectious type of the disease, disorders are expressed in the form of seizures, similar to epileptic ones, muscle twitching. Unfortunately, there are consequences after this meningitis, and the prognosis is often unfavorable. This applies to cases where untimely assistance was provided.
The bacterial species almost always carries complications. The consequences manifest themselves in the form of deterioration of vision and hearing. This can also lead to their complete loss. Cerebral palsy and epilepsy attacks may occur. The manifestation of these complications occurs after a year or two after recovery.
The consequences of purulent meningitis suffered in childhood are the most severe. Complications include cerebral infarction, multiple organ failure with paresis of the limbs.
The more severe the form, the worse the consequences. Some of the symptoms last until the end of days. These include:
- epileptic seizures;
- partial or total disruption of brain function. Depending on the affected area, the patient experiences impairment in hearing, thinking, or movement;
- partial paralysis;
- hormonal imbalance;
- deterioration of vision up to loss;
- hypertensive-hydrocephalic syndrome.
RELATED ARTICLES: Serous-purulent meningitis Is it possible to go swimming after meningitis Incubation period of serous-viral meningitis
Bibliography
- Medical microbiology, immunology and virology: a textbook for medical universities / A.I. Korotyaev, S.A. Babichev. - St. Petersburg: SpetsLit, 2008. - 4th ed., revised. and additional -767 pp.: ill.
- Yushchuk N.D. Infectious diseases: Textbook / N.D. Yushchuk, Yu.Ya. Vengerova. - M. GEOTAR-Media, 2013. - 692 p.
- Bogoleptov N.K. Clinical lectures on neuropathology / N.K. Bogoleptov. - M.: Medicine, 2012. - 431 p.
- Meningitis is dangerous, but curable. BUDGETARY INSTITUTION OF THE KHANTY-MANSI AUTONOMOUS DISTRICT – YUGRA. CENTER FOR MEDICAL PREVENTION.
- Differential diagnosis of neuroinfections in children. Kharkov, KhNMU, 2014
Meningitis in all its diversity
We have already mentioned that most often meningitis in children is of an infectious nature, they are different and differ depending on the pathogen. For example, viral meningitis often occurs against the background of viral infections such as chickenpox, rubella, measles, herpes infection, influenza, etc.
In children with immunodeficiency (for example, in patients with AIDS), fungal meningitis most often occurs.
As a rule, meningococcus enters the child’s body through the nasopharynx (airborne) and then spreads through the bloodstream - into the meninges, joints, lungs, internal organs, etc. Wherever meningococcus appears, it can cause an inflammatory process (meningococcal infection). If this happens in the membranes of the brain, it means that the child will have to be treated for meningococcal meningitis.
By the way, before the advent of antibiotics, every meningococcal meningitis ended in the death of a child and an adult. Nowadays, the mortality rate from meningococcal infection (including meningococcal meningitis) is also high - from 5 to 15% of the number of cases.
In addition to meningococcus, the causative agents of bacterial meningitis in children can be: pneumococci, staphylococci, Haemophilus influenzae, Koch's tuberculosis bacillus and other bacteria.
If there is any suspicion of meningitis, parents are required to seek medical help, preferably immediately to an infectious diseases clinic. Meanwhile, it will be useful for parents to know that, for example, most viral meningitis is not at all terrible. They go away on their own 5-7 days after the onset of inflammation, as soon as the immune system produces a sufficient amount of antiviral interferon.
But bacterial meningitis (and, alas, they are the majority) are much more dangerous! This group of meningitis in children is successfully treated, as a rule, only if antibacterial treatment was started on the first day after infection.
A 100% accurate method for confirming the diagnosis of meningitis in a child (and identifying the pathogen) is a spinal puncture.
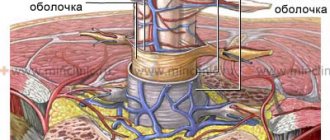
Meningitis and its classification
What is meningitis? This is an infectious disease that causes damage to the lining of the brain. There are three of these membranes in the brain: the hard shell, under it is the arachnoid membrane, and under it is the soft shell. Each of the membranes performs its own function, and all of them are important for the proper functioning of both the brain and the entire body as a whole. However, the disease is quite rare. As Dr. Komarovsky notes: “Of the several thousand who got meningococcus in the nose, one will have a runny nose. And of the several thousand who develop a runny nose, one will develop meningitis.” Nevertheless, the disease is quite dangerous, since untimely treatment can lead to a number of serious complications and consequences for life, which we will also talk about in this article.
There are several classifications of this disease:
- by origin;
- according to the nature of the disease;
- by which membranes of the brain are damaged;
- by pathogen.
Based on their origin, there are primary and secondary meningitis. In other words, primary is an independent disease, and secondary is a consequence or complication of another disease.
Based on the nature of the disease, there are two types: serous and purulent. The symptoms of serous meningitis are milder compared to the symptoms of purulent meningitis.
Based on damaged membranes of the brain, three types of meningitis are distinguished:
- leptomeningitis - with this disease the arachnoid and soft membranes are damaged, it occurs most often;
- pachymeningitis - in this case the hard shell suffers;
- arachnoiditis is a rather rare type of meningitis that affects the arachnoid membrane.
Based on the pathogen, there are two types of meningitis - viral and bacterial, each of which has its own subtypes, depending on the pathogen. For example:
- pneumococcal meningitis;
- meningococcal meningitis;
- Escherichia meningitis;
- hemophilic meningitis;
- streptococcal meningitis;
- staphylococcal meningitis;
- meningitis caused by other bacteria;
- unspecified bacterial meningitis;
- salmonella meningitis;
- listeria meningitis.
One of the most dangerous types of meningitis is tuberculous meningitis.
Photo source: shutterstock.com
The first signs of meningitis in a child
The incubation period of meningitis in children and adults can range from 2 to 10 days. Most often - from 4 to 6 days.
The development of inflammation of the meninges is characterized by the appearance of:
- a sharp increase in body temperature;
- severe headaches;
- repeated vomiting.
Patients also experience photophobia and a sharply negative reaction to loud sounds.
All the main symptoms of meningitis are divided into general infectious, cerebral and meningeal. The appearance of inflammatory changes in the cerebrospinal fluid is also specific.
How does meningitis manifest in children?
The clinical picture of general intoxication syndrome is characterized by the appearance of elevated body temperature, fever, chills, severe pallor, restless behavior in the child, and refusal to eat and drink.
Symptoms of meningitis in children
General cerebral signs of meningitis in children are manifested by intense pain in the head, localized mainly in the frontotemporal region and intensifying when the child tries to move the eyeballs. Loud noises and bright lights also lead to a sharp increase in headaches. Vomiting in patients with meningitis is repeated, does not bring relief, is independent of food intake and is not accompanied by nausea.
Impaired consciousness, development of psychomotor disorders, stupor, stupor or coma are possible. Seizures may develop.
For manifestations of meningeal syndrome, a forced lying position (posture of a pointing dog or cocked gun) is specific.
Pointing Dog Pose:
Pointer dog pose for meningitis
In addition to severe photophobia and increased pain sensitivity, specific meningeal symptoms develop (the main diagnostic signs of inflammation of the meningeal tract).
The main specific symptoms of meningitis in a child
The most commonly identified meningeal symptoms (signs) are:
stiff neck;
Rigidity of the neck muscles
Brudzinski's symptoms;
- Kerning's sign;
- Lessage's symptom (specific only to young children). It is manifested by the baby pulling his legs towards his stomach when he lifts his armpits;
Symptoms of meningitis according to Lessage
- Bekhterev's symptom, accompanied by the appearance of local pain when tapping on the zygomatic arches;
- Mondonesi's symptom, manifested by sharp pain with light pressure on the eyes.
The most characteristic signs of meningitis in a teenager or adult will be the symptoms of neck stiffness, Kerning and Brudzinski.
The development of meningococcemia is accompanied by the appearance of an extremely specific meningococcal rash. Meningitis rashes have a star-shaped irregular shape and are localized mainly on the buttocks and legs. The rash may also spread to the torso, arms and face. In the center of the elements of the rash, necrosis may appear. With severe meningococcemia, the elements of the rash may merge.
Skin rash due to meningitis
Meningitis rash
It should be noted that in babies in the first year of life, meningitis can lead to severe hydrocephalus in a very short period of time. For infants, typical signs of meningitis are the appearance of a high-pitched cerebral cry, pulsation and significant bulging of the large fontanel.
From the editor: How dangerous is a brain cyst?
Symptoms of meningitis in teenagers
For adolescents and adults, the presence of meningococcal nasopharyngitis preceding meningitis is more typical. Meningococcal nasopharyngitis differs from ordinary viral nasopharyngitis in its bluish-purple hue and pronounced granularity of the posterior pharyngeal wall.
Also characteristic is the appearance of high temperature, fever, weakness, dizziness, headaches, nasal congestion, hoarseness, etc. That is, there are no special differences from a regular acute respiratory infection.
The diagnosis of meningococcal nasopharyngitis is made only after bacteriological or serological tests. The development of meningococcal nasopharyngitis can be suspected by the presence of contact with a patient with inflammation of the bladder. In this regard, all patients with an acute respiratory viral infection who have had contact with the patient must be hospitalized in an infectious diseases hospital.
Nasopharyngitis can occur as a separate form of meningococcal infection, but in a short period of time they can turn into severe forms of inflammation of the bladder or meningococcemia.
Classification
According to clinical manifestations, meningococcal infection is divided into the following types:
- Localized - meningococcal carriage (asymptomatic presence of meningococcus on the nasopharyngeal mucosa), nasopharyngitis.
- Generalized - meningitis, meningoencephalitis, acute, typical, chronic forms of meningococcemia, as well as a mixed generalized form (meningitis and meningococcemia).
- Rare forms - meningococcal arthritis (synovitis), polyarthritis, pneumonia, endocarditis, iridocyclitis.
According to the severity of the disease, it is divided into mild, moderate-severe, and severe forms. Separately, there is a hypertoxic form of meningococcal infection, which is also called the “lightning killer”. The patient's condition quickly deteriorates: the temperature rises to +40 C, a rash appears before our eyes, convulsions appear, blood pressure drops, and the person may lose consciousness. The lack of emergency medical care leads to infectious-toxic shock, coma and inevitable death.
Treatment
Important! Under no circumstances should you self-medicate. If the presence of this disease is suspected, the child is immediately hospitalized
Treatment is carried out under the close supervision of a doctor. The disease is very insidious, and at any moment the patient’s condition can worsen, even becoming critical.
Meningitis can cause irreversible damage to the brain and can also be fatal. That is why his treatment should be carried out in a hospital under the strict supervision of a doctor.
Important! Correct diagnosis and spinal puncture will help determine the form of the disease and select the correct treatment.
Treatment of meningitis in a child depends on what causes it (viruses or bacteria), as well as on its stage and the extent of damage to the meninges. The main form of treatment for this disease is the use of medications.
- The viral form of meningitis in children is considered the easiest to treat, since it is almost never accompanied by a bacterial infection. In this case, the basis of treatment is antiviral drugs that inhibit the interaction of the cell with the virus at different stages of the disease. The most commonly prescribed antiviral drugs are:
- Interferon – 120 rubles.
- Amantadine - in the form of tablets 200, and in the form of injections - 1350 rubles.
- Oksolin - average cost 60 rubles.
- Remantadine – 230 rub.
- Antibacterial drugs are prescribed for acute meningitis caused by various bacteria. Antibiotic therapy is also prescribed in cases where it is impossible to determine the causative agent of the infection. The most commonly prescribed drugs are:
- Amoxicillin - average price 130 rubles.
- Cefuroxime – 1300 rub.
- Aztreonam – 120 rub.
General recommendations
To alleviate the condition of a sick child, you should adhere to the following recommendations:
- Due to the increased sensitivity to light that appears after inflammation is relieved, the sick child should be in a darkened room.
- Provide complete rest to the child. He shouldn't be nervous or cry.
- Immunity should be boosted with vitamin complexes.
- It is recommended to follow a gentle diet, excluding hot dishes (even soups should be warm), sweets, fatty foods, marinades and pickles (they have a stimulating/irritating effect on the nervous system).
Remember:
- Under no circumstances should you rub or squeeze boils or large pimples on the neck or face.
- When the first symptoms of sinusitis, otitis media or any other disease develop, immediately obtain specialist advice regarding the effective treatment of one of these ailments.
- Ask your family doctor about the possibility of vaccination at the clinic.
ethnoscience
It is worth noting that treating this disease at home is unacceptable.
Many parents try to protect their child from taking medications, but in this case it can lead to disastrous consequences, even death. Treatment of meningitis in children should be carried out using special medications prescribed by a doctor. However, some traditional methods can complement treatment and have a beneficial effect on the body.
- For severe headaches, you can give your child decoctions of herbs such as barberry, meadowsweet. It is recommended to take such decoctions no more than 2 times a day, 1-2 tablespoons after meals.
- An infusion of medicinal lavender flowers helps well against cramps and spasms. To do this, you need to pour boiling water over 2 teaspoons of dry raw materials, and then let it brew for several hours. Should be taken 2 times a day, morning and evening.
- Linden tea is an excellent pain reliever and anti-inflammatory agent for meningitis. You need to brew a quarter cup of linden blossom with boiling water and let it brew for 10-15 minutes.
- During convulsions, a sick child is recommended to do a wrap. Salt must be diluted in warm water and soak the sheet in it. Then the child is wrapped in it, insulated and left in this position for 1 hour.
- Another good folk remedy is a bath with Veronica officinalis infusion. It is necessary to grind 200 g of raw materials and pour 2-3 liters of boiling water. After the decoction has infused, it is added to the bath water, the temperature of which should not exceed 37.5 degrees. The duration of the procedure should not exceed a quarter of an hour. The use of this folk remedy should be agreed with the attending physician.
Risk group
Children and the elderly are at risk for meningitis. In addition, this disease is often diagnosed in people with an absent spleen and immunodeficiency.
The spread of meningitis, like all other infectious diseases, is more active in crowded places, closed groups, for example, in kindergartens, schools, student dormitories, barracks, since it is easier to get meningitis if you are in the company of asymptomatic carriers.
Most often, meningitis is transmitted by airborne droplets. This mechanism of infection transmission is considered the most common and characteristic of meningitis of viral origin. The infectious agent is transmitted through coughing, sneezing, kissing and sexual contact.
Newborn babies can become infected from an infected mother through the birth canal. The likelihood of infection is especially high in children born by caesarean section. Bacterial and viral meningitis can be transmitted this way.
Infection with meningitis can occur through the oral-fecal route: through dirty food or untreated water.
In addition, meningitis can develop as a result of the bite of an insect or animal that carries an infectious agent.
Expert opinion
Andrey Igorevich Volkov
Neurologist, Candidate of Medical Sciences
Meningitis of any origin is a dangerous infectious disease that affects adults and children. Without timely treatment, death occurs in 80% of cases. It has been proven that, despite the initiation of therapy, 10% of patients die within the first day from the onset of pathological symptoms. Meningitis most often affects children. Viral etiology accounts for 60–70% of cases. Fungal meningitis accounts for 1–3%. It is not possible to diagnose and treat an infectious disease at home. Therefore, it is necessary to seek medical help soon after the first signs of the disease appear.
The most informative method for diagnosing meningitis is lumbar puncture. The causative agent of the disease is sown in the cerebrospinal fluid. To identify the localization of the pathological focus in the brain area, neurologists at the Yusupov Hospital prescribe MRI and CT. Etiotropic therapy is selected depending on the results obtained. Symptomatic treatment is aimed at alleviating the general condition. Vaccination is considered the only reliable means of preventing meningitis.
Symptoms of meningitis in infants
The disease develops quickly. Sometimes meningitis is preceded by otitis media or ARVI. The child develops a high fever, becomes restless and irritable, or, conversely, unusually lethargic. He reacts to touch by crying, as if his skin is irritated by something. The fontanel on the head thickens, swells and pulsates. The child may develop an aversion to food to the point of vomiting, and the occipital and posterior femoral muscles become tense. I may experience convulsions. An alarming symptom is the appearance on the child’s skin (usually on the legs and torso) of petechiae - purple pinpoint hemorrhages of various shapes and sizes that do not disappear with pressure.
Editor's note: How a pituitary adenoma is removed
If a child exhibits symptoms indicating meningitis, you should immediately seek medical help: call an ambulance or go to the hospital yourself!
Symptoms of the disease
Now about how to recognize meningitis in a child yourself. This is important to know, since only timely consultation with a doctor can protect the child from torment and suffering in the future.
List of warning signs:
- Strong headache;
- photophobia;
- temperature increase;
- pallor (even if the temperature is low);
- nausea and/or vomiting;
- stiff neck – this is when a child cannot bend his head forward; when lying down, he throws his head back;
- lethargy, drowsiness;
- a rash that looks like red or purple bruises that doesn't go away when you put pressure on it.
In children under 1 year of age, it is more difficult to determine meningitis, since infants are just adapting to a new world. In this case,
the following symptoms may help:
- increased temperature (feet and palms may be cold);
- lethargy and drowsiness, difficult to wake up;
- refusal to breastfeed and reluctance to contact mother;
- flexion of limbs;
- refusal to eat and/or vomiting;
- constant monotonous crying;
- pallor;
- a bruise-like rash that doesn't go away when you press on it;
- empty look.
Once again, we draw your attention to the fact that meningitis is a rare disease, so if you find something, this does not mean at all that the child has meningitis. But nevertheless, if you find something from the list, it is better to call an ambulance or rush to the nearest hospital if the ambulance takes a long time to get to you, since delay can lead to serious consequences.
Photo source: shutterstock.com
Diagnosis of meningitis in newborns
Lumbar puncture for cerebrospinal fluid analysis. Complete blood count, levels of CRP, blood glucose, electrolytes; coagulogram, blood culture.
Diagnosis is based on microbiological methods (isolating a culture of microorganisms from cultures of CSF and blood). CSF cultures are positive in 70-85% of patients who have not previously received antibiotic therapy.
Negative cultures can be obtained during antibacterial therapy, brain abscess, infection caused by M. hominis, U. urealyticum, Bacteroidesfragilis, enteroviruses or herpes simplex virus. Infectious meningitis in newborns is characterized by an increase in protein content in the CSF and a decrease in glucose concentration. The number of leukocytes in the CSF is usually increased due to neutrophils (more than 70-90%).
Despite the wide variation in the cellular composition of the CSF, the generally accepted level of leukocytes in the CSF is >21 cells per 1 mm3 for culture-proven meningitis (sensitivity - 79%, specificity - 81%). Cytological and biochemical methods (changes in the cellular and biochemical composition of the CSF) are not always specific.
CSF glucose should be at least 55-105% of the blood glucose level in premature infants, and 44-128% in full-term infants. The protein concentration may be low (<0.3 g/L) or very high (>10 g/L).
There is no clear opinion on the need for CSF examination in patients with RNS. The American Academy of Pediatrics recommends performing a spinal tap on newborns in the following situations:
- positive blood culture;
- clinical or laboratory data strongly suggest bacterial sepsis;
- worsening during treatment with antimicrobial drugs.
If necessary, lumbar puncture can be delayed until the condition is stabilized, although there is a risk of delay in diagnosis and possibly inappropriate use of antibiotics. If a newborn with suspected sepsis or meningitis has abnormal CSF values, but blood and CSF cultures are negative, a repeat lumbar puncture should be performed to rule out anaerobic, mycoplasma, or fungal infection; It is also necessary to study the CSF for herpes, cytomegalovirus, and toxoplasmosis. Late analysis (delay greater than 2 hours) may significantly reduce the white blood cell count and glucose concentration in the CSF. The optimal time for delivery of material to the laboratory should not exceed 30 minutes.
Meningitis with normal indicators. Up to 30% of newborns with GBS meningitis may have normal CSF values. In addition, even microbiologically confirmed meningitis does not always lead to changes in the cellular composition in the CSF. Sometimes, in addition to increased CSF pressure, no other pathology in the CSF may be detected or the indicators may be “borderline”. In doubtful cases, for example, with “borderline” values of CSF parameters (leukocytes > 20 in 1 mm3 or protein > 1.0 g/l), in the presence of clinical symptoms, it is necessary to examine newborns for the presence of specific infections (syphilis, rubella, cytomegalovirus, herpes, AIDS virus).
Microscopy with Gram stain. Organisms in Gram-stained CSF smears are detected in 83% of neonates with GBS meningitis and in 78% of those with Gram-negative meningitis.
The likelihood of bacteria being visualized on a Gram stain correlates with the concentration of bacteria in the CSF. CSF culture is critical to diagnosis, regardless of other findings. A complete examination of the CSF is all the more necessary, since the pathogen isolated from the blood will not always match the CSF culture.
Ventricular puncture should be considered for meningitis that does not respond clinically or microbiologically to antibiotic therapy due to ventriculitis, especially if there is obstruction between the cerebral ventricles and between the ventricles and the spinal canal.
Diagnosis of meningococcal infection
The choice of laboratory material for analysis depends on the form of the disease; it can be blood, nasopharyngeal mucus, cerebrospinal fluid, scrapings from a hemorrhagic rash, purulent discharge from the meninges.
For nasopharyngitis and asymptomatic carriers, nasopharyngeal secretions are collected using a special swab. The material must be taken from the back wall of the throat behind the soft palate.
For cerebrospinal meningitis, CSF (cerebrospinal fluid) is collected. It is collected by puncture in an amount of 2 - 5 ml into a sterile tube. They are immediately sown on a nutrient medium or urgently, observing the temperature regime, sent to the laboratory. At the time of collection of cerebrospinal fluid, the presence of pus can be visually determined; in this case, the cerebrospinal fluid will be cloudy. In some cases, bacteria can only be detected under a microscope.
When collecting biomaterial posthumously, pus from the membranes of the brain is most often taken for analysis. The study is necessary to clarify the diagnosis. If meningococcal disease is confirmed, the circle of contacts should be identified to prevent the spread of infection.
Blood and serum tests are optional. It allows you to assess the severity of the condition, as well as detect antibodies to meningococcus. Based on urine test data, kidney function can be determined. To make a diagnosis and assess the extent of damage to the body, instrumental diagnostic methods such as echocardiography, x-ray, ultrasound of the brain and abdominal organs, Doppler examination of blood vessels, ophthalmoscopy, and magnetic resonance imaging are used.
Types of laboratory diagnosis of meningococcal infection
Bacterioscopic examination (RA, PCR). Determines the presence of meningococci, serogroup and their concentration. Allows differentiation from other bacteria that cause inflammation of the brain and spinal cord. The crop is sown for 18 to 24 hours in a thermostat at +37 C, with a high CO2 content (up to 10%). Neisseria meningitidis is determined by detecting the production of acetic acid as a result of the fermentation of glucose and maltose.
The serological method (ELISA, RIA) is based on the detection and determination of the concentration of IgM antibodies. The titer increases significantly at the onset of meningococcal infection in generalized forms. The concentration decreases during the period of remission, IgG antibodies begin to predominate over IgM immunoglobulins. In patients who have recovered from the disease, specific bactericidal antibodies are detected in the blood serum: agglutinins and hemagglutinins.
Regardless of the type of biomaterial, it requires urgent analysis since the pathogen dies outside the human body. Laboratory diagnostics includes microscopy, biological culture, and requires not only identification of the pathogen, but also determination of antibiotic sensitivity.
Consequences in adults
Some people who have had meningitis are lucky - after treatment they remember the disease as a bad dream and do not face any serious health problems, with the exception of headaches that almost do not interfere with life, arising from overwork or changes in weather.
Sometimes meningitis reminds itself of itself by decreased concentration and attention, as well as worsened memory.
However, those who recovered often experienced loss of hearing or vision, stuttering or strabismus, developed epilepsy, dropsy of the brain, or a decrease in their level of intelligence.
A person who has had meningitis may also experience mental disorders, including the development of schizophrenia.
Depending on the cause of the disease and its causative agent, problems associated with internal organs may also appear. Often a person’s limbs were even amputated due to developed necrosis.
Fortunately, with the modern level of medicine, this disease can be successfully treated: it is unlikely that a person who sees a doctor in time will remain disabled for life. He will not necessarily become weak-minded - often those who have had meningitis continue to build a career or receive a second higher education.
If a person has had a purulent form of meningitis, he or she becomes immune to the specific bacterium that causes the disease. But he can become infected with meningitis more than once. By the way, most often only people with skull injuries get it again.
Meningitis is a disease that should never be joked with.
It is important to remember that everything can end happily if the patient is taken to the doctor on time. The main thing is not to lose composure and not to panic, but to dial the emergency number as soon as possible
From the editor: How to develop memory in preschool children
In order to protect yourself and your loved ones, you need to know how meningitis is transmitted and what are the first symptoms of this insidious disease. Everyone should know this.
Based on the nature of the headaches, we can talk about possible diseases. You can find out how headaches with a brain tumor manifest themselves by following this link.
Complications and consequences of meningitis
As a rule, complications after an illness occur in every 5th patient.
The consequences most often appear in children under 7 years of age and in adults after 60. The most common complication is headaches, which appear with a sudden change in weather or excessive mental and physical stress. Meningitis is a serious disease in which dangerous complications develop.
Most often, its consequence is the development of convulsive syndrome, hydrocephalus of the brain, hearing loss, and the development of subdural exudate in newborns.
Such conditions prolong the rehabilitation period and often leave permanent health consequences.
But this is not the only pathological condition that can develop against the background of a previous illness. Among the neurological consequences of meningitis, early and late are distinguished.
The early group includes:
- irreversible deformations of the cranial nerves;
- ICP, that is, increased intracranial pressure;
- various chronic and acute diseases of the hematopoietic system;
- dropsy of the brain (hydrocephalus);
- rare epileptic seizures;
- strabismus;
- subdural effusion.
Late complications include:
- epilepsy;
- a sharp decline in intellectual abilities, dementia;
- sensorineural hearing loss;
- a sharp decrease in the functioning of the organs of hearing and vision.
In addition to neurological consequences, against the background of meningitis, systemic pathologies can develop or be complicated: pneumonia, arthritis, sepsis, endocarditis, and in women there is a risk of developing psychological diseases. However, if treatment was started in a timely manner, then most of the possible complications can be avoided.
Causes of the disease
There are many reasons for its occurrence, but most are similar in that a harmful pathogen (virus, bacteria, fungus, etc.) enters the body, which is why the disease develops. Therefore, in this case, it is more appropriate to talk about transmission routes and risk groups.
You can become infected with meningitis:
- by airborne droplets (both from the patient and from the carrier);
- through rodent and insect bites;
- by the oral-fecal route (residues of rodent excrement on unwashed vegetables or fruits);
- when drinking dirty water;
- through contact and household contact (again, both from the patient and from the carrier);
- during childbirth.
There are also cases of traumatic meningitis, when due to a head injury (trauma to the base of the skull, open fracture of the skull), pus flows out and the pathogen enters through the mucous membrane, ear canal or wound.
Most often the disease is affected by:
- children under 5 years old;
- premature babies;
- children who had a difficult pregnancy (pregnancy had complications);
- children who have suffered purulent diseases (otitis media, tonsillitis, sinusitis, etc.);
- children suffering from nervous system disorders (acquired or congenital);
- children who have not been vaccinated against meningococcus, rubella, measles, Haemophilus influenzae, mumps;
- children with acquired or congenital immunodeficiency;
- children who attend preschool or have frequent contact with large numbers of people;
- people with weakened immune systems.
Since immunity plays an important role in whether meningococcus or any other microorganism will be able to penetrate the body and take root there, it is worth mentioning the factors that reduce immunity.
The following weakens the body:
- stress;
- smoking;
- excessive use of alcohol or drugs;
- hypothermia;
- unbalanced diet;
- lack of vitamins;
- improper use of medications (self-medication);
- head, neck, back injuries;
- chronic diseases (bronchitis, HIV infection, diabetes, etc.);
- past infections (rubella, otitis media, acute respiratory infections, acute respiratory viral infections, etc.).
You should also remember that you can get meningitis more than once.
Disease Prevention
Post-infectious immunity. After an illness, a strong immunity develops that protects against re-infection. However, it occurs only in the serogroup of bacteria that caused the disease. In total, there are 12 types of meningococcal groups.
- Vaccination. 3 types of vaccines have been developed:
- Polyvalent polysaccharides (invented 30 years ago).
- Mono- and polyvalent conjugate vaccines (used since 1999).
- New monovalent conjugate vaccine MenA (developed in 2010-2011).
As much as possible, the drug can cover only 4 serogroups: A, C, Y and W. Unfortunately, such a vaccine has not yet been developed to protect against all types of infection.
The meningococcal vaccine is not included in the childhood vaccination schedule. You can only get vaccinated yourself. It should be carried out before traveling to countries at risk and for epidemiological reasons, i.e. during an epidemic when the serotype is known.
Differential diagnosis of pathology
After examining and interviewing parents, the following procedures are prescribed:
Cerebrospinal fluid examination.
When the diagnosis is confirmed, an increase in protein levels is detected in the cerebrospinal fluid with a normal glucose concentration. An increase in lymphocytes means the viral nature of the disease. After the puncture, the child feels much better.
Serological examination of cerebrospinal fluid in the blood.
This test helps identify the virus that caused the disease and find antibodies to it.
PCR of cerebrospinal fluid.
Can detect viral DNA. This is the final analysis aimed at confirming or refuting a specific virus.
Inoculation of cerebrospinal fluid on a nutrient medium.
The doctor may prescribe additional tests to make sure which form of the disease has overcome the baby. .
What is the difference between viral and bacterial meningitis
Bacterial differs in that it is provoked by streptococcal bacteria. This type attacks people with HIV, those who have undergone surgery in the abdominal area, and those with alcohol addiction.
This type is detected by laboratory analysis of cerebrospinal fluid.
Diagnostics
If a child has meningitis, you should contact a pediatric infectious disease specialist. He will first conduct an inspection and ask questions that interest him in order to get a complete picture. In addition to the standard history taking, in all cases of suspected meningitis, a spinal puncture is required. This is a very painful and unpleasant procedure: the patient is placed on his side, a needle is inserted into the spinal cord, and then some cerebrospinal fluid is removed. It is this that is used as material for analysis.
In addition to the puncture, a number of other tests are performed:
- general urine analysis;
- general stool analysis;
- general blood analysis;
- culture of mucus from the nasopharynx;
- bacteriological examination of blood and cerebrospinal fluid;
- ECG;
- radiography;
- MRI;
- KG;
- EEG;
- PCR.