What is neurosis
Many people know about neurosis firsthand and have experienced this painful state more than once.
Stress and overwork can cause this negative state, which suppresses all desire to live, be active, and work. The person becomes either too lethargic or irritable. Neurosis is also characterized by severe fatigue, which can manifest itself without obvious reasons. Neurosis is a disease that affects the nervous system. Sometimes it is not visible from the outside, and the patient may appear to be completely healthy. But in fact, at the same time, he may feel fear, panic, irritation, a desire to cry, which may be absolutely independent of external factors. Sometimes neurosis does not manifest itself due to stress or depression, or extreme fatigue at work. Symptoms may appear for other reasons, which lie in physical diseases of the internal organs. Also, neurotic conditions are often suffered by people who have experienced a nervous breakdown or suffered from thyroid diseases at least once in their lives. Neurosis-like conditions do not arise from stress, as experts believe, unlike ordinary neuroses. And psychological factors do not play a special role here. Many believe that the problem lies elsewhere.
Diagnostics
When diagnosing neurosis, it is important to identify the traumatic trigger. To do this, psychological testing of the patient is carried out. Then the structure of his personality is examined and a pathopsychological examination is performed. To exclude mental disorders, the patient is referred for consultation to a psychiatrist. During a neurological examination, no signs of focal symptoms are found in a patient with neurosis.
There is a general revival of reflexes and tremor of the fingers with arms extended forward. Then the neurologist prescribes additional diagnostics to exclude organic brain disorders (EEG, REG, MRI, vascular ultrasound). To exclude pathologies from the cardiovascular system, a consultation with a cardiologist is prescribed.
Types of neurosis-like conditions
Asthenic syndrome.
This is one of the most common neurosis-like conditions that a person can experience. It does not appear immediately; it develops gradually, increasing and worsening the patient’s well-being. At first, you may experience severe fatigue and a constant desire to lie down, sit down, and rest after minimal exertion. At the same time, emotional instability manifests itself when a person himself cannot control his emotions. After strong irritability comes an apathetic state when you don’t want anything and don’t need anything. A person may distort reality and have an incorrect assessment of current events. Such people have a very difficult time tolerating too bright stimuli, such as strong light, loud sound and unpleasant smell. At night I don’t want to sleep, but during the day I constantly feel sleepy. Even physical aspects such as heart pain and headaches can manifest themselves. Inside there is a feeling of constant anxiety and expectation of bad things, although no real factor contributes to this. All these manifestations become especially aggravated during sudden changes in weather and season.
Obsessive-compulsive syndrome.
It manifests itself as obsessive thoughts, movements, unreasonable fears, which are difficult to get rid of, even thinking logically. At the same time, the patient understands everything and can evaluate his condition as strange and stupid, but physically he cannot cope with it. Some people with a strong will can, by constantly controlling themselves, get rid of obsessive states. But this may not last long, since without proper treatment of the nervous system, everything can come back again. Such conditions are precursors to depression, neuroses and various psychopathic diseases.
Hysterical syndrome.
A person with such a syndrome will behave brightly, and sometimes even too defiantly. He will play to the public, express his emotions and behave demonstratively, drawing considerable attention to himself. His gestures are broad and attention-grabbing. Emotions may include loud laughter, crying, exclamations, and even fainting. In fact, such manifestations have nothing to do with real hysteria, when a person cannot control himself. In fact, this is just an imitation of a seizure. Unfortunately, this syndrome is not very harmless: as a result of these manifestations, deafness and blindness, as well as paralysis, can even develop.
Hypochondriacal syndrome.
The patient may be completely healthy and have no problems other than with the nervous system. And at the same time, he will constantly fear for his well-being, listen anxiously to himself and not find peace during the day, worrying about the slightest pain or unpleasant sensation in the body. At the same time, he is very suspicious and invents many diseases for himself. Most often, such people spend days in hospital queues, visiting all kinds of specialists in order to identify at least one far-fetched ailment. They undergo diagnostics, undergo consultations and constantly complain about their health, although there may be no real reasons for this.
The article presents data on the characteristics of mental disorders in 3-year-old children with residual symptoms of perinatal CNS damage of hypoxic-ischemic origin. The leading disorders include neuropathic syndrome and residual organic psychosyndrome.
Nonpsychotic psychic disorders of residual-organic genesis in infants with perinatal defeat of the central nervous system
The article presents data of nonpsychotic psychic disorders in children 3 years with perinatal hypoxic-ischemic defeat of CNS. Major syndromes are neuropathic symptoms and residual-organic psychosyndrome.
Adverse effects in the early stages of ontogenesis can cause developmental defects, cerebral palsy and mental retardation, and other diseases of the nervous system. The impact of pathogenic factors on the fetus in late pregnancy causes a deviation in the formation of higher cortical functions [1].
Disorders of intrauterine development of the fetus due, first of all, to chronic intrauterine hypoxia, increase the risk of perinatal damage to the central nervous system. And if in the first half of life, disorders of the nervous system are of a medical nature, then later they acquire a social connotation, posing a threat to physical and mental health [2-7].
An important task facing specialists working in the field of perinatal medicine is the creation of a system of prognosis, early diagnosis, development of unified programs for the prevention, treatment and rehabilitation of children in the neonatal period and subsequent periods of life [1, 8, 9].
With the emergence and improvement of reproductive, fruit-preserving and neonatal technologies, there is an increase in the birth of children with perinatal pathology. In addition, technologies themselves can become sources of the birth of children with disabling pathologies [1, 8].
Epidemiological studies in recent years indicate an increase in the number of borderline neuropsychiatric disorders in various groups of the world population. According to WHO experts, up to 20% of children worldwide have mental health problems. The leading place among child and adolescent borderline pathologies is occupied by non-psychotic mental disorders of residual organic origin [15, 16, 17].
Knowledge of the clinical characteristics of the initial manifestations of mental disorders caused by perinatal pathology allows us to identify a risk group for special rehabilitation measures from the first year of life, “at the origins of the disease” [11-13].
The modern paradigm of the biopsychosocial approach to diagnosis, therapy and rehabilitation argues that the provision of psychiatric care requires more intensive development of out-of-hospital, consultative and therapeutic types of care, including a multiprofessional and interdepartmental approach, relying on the primary links of general somatic services. Unfortunately, despite numerous studies [12, 14, 16, 17, 19, 20, 22], the issue of the influence of perinatal damage to the central nervous system on the subsequent mental development of a child in an early age remains insufficiently studied. Observation, diagnosis and therapy of children under 3 years of age with this pathology is carried out mainly by pediatricians, taking into account the diagnostic criteria of the specialty. As a consequence, there is often insufficient understanding of the mechanisms of occurrence of neuropsychic disorders at this stage of ontogenesis, their interpretation from a somatological position and ineffective therapy.
The purpose of the study was to establish the nature of mental disorders in young children who suffered perinatal damage to the central nervous system of mild and moderate severity. This study was carried out on the basis of the Federal State Budgetary Institution Ural Research Institute of OMM of the Ministry of Health of the Russian Federation (director - Doctor of Medical Sciences, Professor V.V. Kovalev). 153 children of both sexes aged 3 years were subjected to a comprehensive study. The selection of children was carried out using a random sampling method.
The inclusion criteria for the study included: 1. Full-term children aged 3 years who had suffered from hypoxic-ischemic PPNS of mild to moderate severity. 2. Full-term children aged 3 years without indications of cerebral pathology of the perinatal period. 3. The overall intellectual indicator of the sample is not lower than average in accordance with the methodological recommendations developed by S.D. Zabramnaya and O.V. Borovik [20], and the indicators of the D. Wechsler subscale (drawing test adapted for children from three years old). Children with pathologies of the organs of hearing, vision, cerebral palsy, mental retardation, EDA syndrome (early childhood autism), degenerative diseases of the central nervous system, intrauterine malformations (IUD), TORCH-associated infections, congenital hypothyroidism, and epilepsy were excluded from the study.
The assessment of the degree of perinatal damage to the central nervous system was carried out on the basis of the “Classification of perinatal lesions of the nervous system in newborns” (2000), adopted by the Russian Association of Perinatal Medicine Specialists (RASPM). Clinical interpretation and differentiated diagnosis of mental disorders are classified in accordance with the syndromic scheme of perinatal damage to the central nervous system (ICD-10, 1996, RASPM, 2005).
The main group consisted of 119 children who had signs of residual organic cerebral insufficiency of perinatal origin at the start of the study. The children under observation were divided into 2 subgroups: 1 subgroup included 88 children who had mental disorders at 3 years of age; Subgroup 2 consisted of 31 children without mental disorders at the age of 3 years. The control group included 34 children aged 3 years who were born healthy and without mental disorders.
Research methods
The clinical research method was the main one and included clinical-anamnestic, clinical-psychopathological and clinical-follow-up research using a specially developed examination card, including a questionnaire among parents. The study of children was carried out by examining and interviewing them, collecting data from parents and close relatives. Testing of children was carried out on the basis of parental consent at 9-10 am, no more than 1 hour, taking into account the psychophysiological characteristics of this age.
In addition to assessing the neurological status, the psychomotor and speech development of children was taken into account. Mental status was assessed based on a clinical examination by a psychiatrist and a psychological block of studies with parental consent.
In the diagnosis, not only the diagnostic rubrics of ICD-10 were used, which ignores the dynamic principle of assessing conditions, but also domestic principles for determining the clinical picture and course, as well as the prognosis of the disease, used in psychiatry. Assessment of mental health, psychomotor and speech development was carried out by a child psychiatrist and, if necessary, a speech therapist.
Statistical processing of the research results was carried out using the Microsoft Excel 7.0 software package for Windows 98 “STATISTICA 6” (M was determined - mathematical expectation (arithmetic mean), standard deviation for the sample, error of the arithmetic mean - m). To assess the significance of differences between groups, Student's t-tests were used for independent samples adjusted for differences in variances (differences in means were considered statistically significant if the significance level did not exceed 0.05; if P ≥ 0.05, differences were rejected) [20, 21].
In the course of this study, an analysis of biological factors influencing the occurrence of neuropsychiatric disorders in 119 young children was carried out. At the same time, it was possible to establish the specific features of the ontogenesis of children who underwent PP of the central nervous system of hypoxic-ischemic genesis of mild and moderate severity in the studied groups. All children were born full-term in the Federal State Budgetary Institution Research Institute of OMM of the Ministry of Health of the Russian Federation and maternity hospitals in Yekaterinburg, among them 73 girls (47.7%, n=119) and 80 boys (52.3%, n=119).
At the initial stage of the study, correlations of small and medium strength were established between mental disorders in children and perinatal factors (p <0.0001). These included: intrauterine hypoxia r=0.53; combined (prenatal and intrapartum) hypoxia of moderate severity – r=0.34; hypoxic-ischemic damage to the central nervous system of mild severity r = 0.42; moderate hypoxic-ischemic damage to the central nervous system r=0.36.
Subsequently, an analysis was carried out of the frequency and structure of complaints made by parents in connection with the health status of their children aged 3 years in the studied subgroups. The data is presented in Table 1.
Table 1.
Frequency and structure of complaints from parents in connection with the health and behavior of their children aged 3 years in the studied groups
| Index | Main group (n=119) | Control group (n=34) M±m,% | R | |||
| 1 subgroup, (n=88) M±m, % | 2nd subgroup, (n=31) M±m,% | P1-2 | P1-3 | R2-3 | ||
| Increased excitability | 51,0±5,0 | 32,0±9,0 | 6,0±4,0 | 0,035 | 0,0001 | 0,004 |
| Increased mobility | 30,0±5,0 | 13,0±6,0 | 6,0±4,0 | 0,034 | 0,004 | 0,188 |
| Meteosensitivity | 33,0±5,0 | 10,0±5,0 | — | 0,006 | 0.0001 | 0,037 |
| Disturbed sleep-wake pattern | 40,0±5,0 | 13,0±6,0 | — | 0,003 | 0,0001 | 0,018 |
| Night terrors | 17,0±4,0 | 3,0±3,0 | — | 0,027 | 0,006 | 0,157 |
| Bruxism | 15,0±4,0 | — | — | 0,012 | 0,011 | — |
| Eating disorders | 49,0±5,0 | 26,0±8,0 | 19,0±7,0 | 0,013 | 0,001 | 0,254 |
| Delayed speech development | 7,0±3,0 | 6,0±4,0 | — | 0,467 | 0,065 | 0,074 |
| Headache | 10,0±3,0 | — | — | 0,032 | 0,03 | — |
| Fears | 39,0±5,0 | 13,0±6,0 | 6,0±4,0 | 0,004 | 0,000 | 0,188 |
| Disobedience | 26,0±5,0 | 29,0±8,0 | 19,0±7,0 | 0,378 | 0,204 | 0,173 |
| Onychophagia | 14,0±4,0 | 6,0±4,0 | 6,0±4,0 | 0,145 | 0,134 | 0,487 |
| Allergic reactions | 38 (43±5) | 9 (29±8) | 6 (18±7) | 0,084 | 0,004 | 0,142 |
| ZRR | 23 (26±5) | 2 (6±4) | 2 (6±4) | 0,010 | 0,006 | 0,463 |
As follows from Table 1, the leading disorder in the studied groups was determined to be a nonspecific neuropathic symptom complex (congenital childhood nervousness syndrome, residual organic neuropathy syndrome according to S.S. Mnukhin). Its occurrence is due to the manifestation of brain dysfunction at the somatovegetative level of neuropsychic response. Its characteristic feature was an increased reaction to external stimuli with intolerance to sharp sounds, bright light, combined with tearfulness, increased moodiness, anxiety and suspiciousness. Among the somatovegetative disorders, dysfunctions of the digestive organs predominated (frequent regurgitation, vomiting, constipation, diarrhea, loss of appetite or its selectivity), as well as sweating, allergic reactions, thermoregulation disorders (tendency to causeless fluctuations in low-grade temperature), and meteosensitivity. Frequent sleep disturbances manifested themselves in paroxysmal forms in the form of night terrors, sleep talking, sleepwalking, and bruxism. Frequent respiratory diseases were noted, occurring in a “chain”, with one incomplete episode of “cold” followed by layers of the next.
The children's behavior was characterized by lethargy, passivity or general motor restlessness and fussiness. Such children had difficulty adapting to new conditions and regime, had increased sensitivity to any external influences, emotional excitability, impressionability, timidity, instability of mood, and a tendency to develop various fears, often vague in content and changeable. Manifestations of neuropathic syndrome were most typical in the first three years of life. Table 2 shows the structure of the neuropathic syndrome in children aged 3 years.
Table 2.
The structure of the neuropathic syndrome in children of the study groups at the age of 3 years
| Symptoms | Main group (n=119) M±m,% | Control(n=34) M±m,% | R | ||||
| 1 subgroup (n=88) | Subgroup 2 (n=31) | P1-2 | P1-3 | R2-3 | |||
| Increased excitability | 45 (51±5) | 10 (32±9) | 2 (6±4) | 0,035 | 0,0001 | 0,004 | |
| Sleep disorders | 35 (40±5) | 4 (13±6) | — | 0,003 | 0,0001 | 0,018 | |
| Meteosensitivity | 29 (33±5) | 3 (10±5) | — | 0,006 | 0,0001 | 0,037 | |
| Allergic reactions | 38 (43±5) | 9 (29±8) | 6 (18±7) | 0,084 | 0,004 | 0,142 | |
| ZRR | 23 (26±5) | 2 (6±4) | 2 (6±4) | 0,010 | 0,006 | 0,463 | |
| Aggressiveness | 15 (17±4) | 2 (6±4) | — | 0,072 | 0,006 | 0,074 | |
From Table 3 it follows that at the age of 3 years in children of the 1st subgroup, a neuropathic symptom complex, which included at least 4 symptoms in the presence of neurological signs, was detected significantly more often when compared with the second subgroup and the control group (p<0.05).
The structure of residual neurological signs indicating perinatal damage to the central nervous system in children at the age of three in the compared groups looked as follows (see Table 3).
Table 3.
The structure of neurological signs of residual organic cerebral insufficiency of perinatal origin in the compared groups at 3 years
| Signs | Main group (n=119) | Control (n=34) M±m, % | R | |||
| 1 subgroup (n=88) M±m, % | 2 subgroup (n=31) M±m, % | P1-2 | P1-3 | R2-3 | ||
| Neurologically healthy | 44 (51±5) | 25 (81±7) | 32 (94±4) | 0,002 | 0,0001 | 0,051 |
| Residual neurological signs | 56 (64±5) | 11 (36±9) | 6 (18±6) | 0,003 | 0,0001 | 0,053 |
| Myatonic syndrome | 21 (24±5) | 7 (23±8) | 4 (12±6) | 0,431 | 0,066 | 0,126 |
| Pyramid syndrome | 8 (9±3) | — | — | 0,041 | 0,034 | — |
| Vegetative-vascular disorders | 14 (16±4) | 4 (13±6) | 2 (6±4) | 0,329 | 0,067 | 0,168 |
From Table 3 it follows that in children of subgroup 1, neurological signs of residual organic cerebral insufficiency were recorded significantly more often (p<0.01). The cause of these neuropsychic disorders was hypoxia and cerebral ischemia in the pre- and perinatal period, which was documented. As a consequence, the development of a neuropathic symptom complex and residual organic psychosyndrome with phenomena of partial delay in mental and speech development at the somato-vegetative stage of the neuropsychic response [22]. The above disorders were characterized by non-progressive dynamics associated with the processes of repair, compensation and decompensation of impaired functions, and age-related maturation of brain systems. In the clinical picture, some children observed reverse development (regregency) and compensation. Decompensation of these disorders was observed at the age of 3 years, which was due to the first age-related critical period [16, 21].
Analysis of speech development based on data from an outpatient card and speech therapy study made it possible to judge the characteristics of speech development in children in the compared groups at the age of 3 years (see Table 3).
Table 4.
Features of speech development in compared groups of children aged 3 years
| Deviations in speech development | Main group (n=119) | Control (n=34) | R | ||||||
| 1 subgroup (n=88) | Subgroup 2 (n=31) | 1-2 | P1-3 | R2-3 | |||||
| Abs | M±m,% | Abs | M±m,% | Abs | M±m,% | ||||
| Delayed speech development | 11 | 13±4 | — | — | — | — | 0,018 | 0,016 | — |
| Impaired means of communication (phonetic-phonemic speech disorder) | 37 | 43±5 | 6 | 19±7 | 2 | 6±4 | 0,009 | 0,0001 | 0,056 |
| Stuttering | 7 | 8±3 | — | — | — | — | 0,052 | 0,046 | — |
| General speech underdevelopment (GSD) | |||||||||
| ONR level I | 3 | 3±2 | — | — | — | — | 0,151 | 0,140 | — |
| ONR level II | 14 | 16±4 | — | — | — | — | 0,009 | 0,007 | — |
| ONR level III | 8 | 9±3 | 2 | 6±4 | 2 | 6±4 | 0,326 | 0,283 | 0,463 |
From Table 4 it follows that children of subgroup 1 were significantly more likely to have delayed speech development, phonetic-phonemic speech underdevelopment and general speech underdevelopment (GSD) of levels I and II, as well as stuttering. In children of the 2nd subgroup without mental disorders, the state of speech development did not differ significantly from similar indicators in the control group, corresponding to the age norm (p <0.05). At the same time, general speech underdevelopment (GSD) of level II (moderately expressed speech development delay) was determined mainly in children of subgroup 1 (p <0.01).
Level 1 OSD (virtually no speech) was diagnosed only in 1 subgroup (p>0.05). Impaired means of communication in the form of phonetic-phonemic speech impairment is observed in all groups, but such children are predominantly observed in subgroup 1 (p1-2<0.01, p1-3<0.01). Phonetic-phonemic underdevelopment of speech is represented by disorders in which the leading factor is a violation of sound pronunciation with normal hearing and normal innervation of the speech apparatus, called functional dyslalia. With dyslalia, there is an inability to voluntarily accept and maintain certain positions of the articulatory organs necessary for pronouncing sounds. Dyslalia may be due to the inability to distinguish and differentiate phonemes. Quite often, isolated use of a sound may not be disrupted, but changed in spontaneous speech. Delayed speech development and general speech underdevelopment of levels I and II in the study were observed in children of subgroup 1 with mental disorders. Thus, in children aged 3 years without mental disorders (subgroups 2 and 3) there were no significant deviations in speech development, and delayed speech development and general underdevelopment of speech of levels I and II were observed only in children of subgroup 1 with mental disorders.
Residual organic psychosyndrome, in addition to symptoms of neuropathy, included cerebrasthenic complaints, delayed intellectual and speech development by the end of 1 year, attention disturbances in the form of increased distractibility, difficulty concentrating, neurological signs (disseminated neurological symptoms (see Table 5).
Table 5.
The structure of the psychoorganic syndrome at the age of three, identified in children of the 1st subgroup at the age of 3 years
| Index | 1 subgroup (n=88) | P1-2 | P1-3 | R2-3 | |
| Abs* | (M±m,%) | ||||
| Lack of intelligence by 1 epicrisis period | 11 | (13±4) | 0,020 | 0,018 | — |
| ZRR for 1 epicrisis period | 11 | (13±4) | 0,018 | 0,016 | — |
| Attention disorders detected during testing | 9 | (10±3) | 0,032 | 0,003 | — |
| Mood swings | 15 | (17±4) | 0,006 | 0,005 | — |
| Headache | 9 | (10±3) | 0,032 | 0,030 | — |
| Scattered neurological symptoms | 17 | (20±4) | 0,004 | 0,003 | — |
*The total number of observations does not correspond to 100% due to the identification of several symptoms in one patient.
As follows from Table 5, in subgroup 1, residual organic psychosyndrome was found in 17 children. This symptom complex was not diagnosed in the comparison groups (p<0.05).
Residual organic psychosyndrome was caused by the influence of pathogenic factors in the pre- and perinatal period (pathological pregnancy, birth trauma, brain asphyxia). The development of mental disorders as a result of hypoxic-ischemic brain damage was determined by the compensatory capabilities of the brain in the process of evolution. Residual organic psychosyndrome was characterized by mild to moderate delay in speech development, increased excitability, instability of emotional and autonomic reactions, sleep disturbances, and poor appetite. At the age of 3 years, children were characterized by increased excitability, importunity, lack of a sense of distance, mood swings, motor disinhibition, and weakness of active attention. Cerebroasthenia was the core symptom complex, which was dominated by persistent headaches, irritable weakness, increased fatigue, intolerance to any type of stress, from vestibular, thermal, to increased meteosensitivity.
Cognitive impairment was manifested by mild to moderate delay in the development of mental functions with a disorder of attention function, and a decrease in mental performance. There was a mild to moderate delay in speech development, manifested in the form of a poor vocabulary, a low level of performance on speech tasks compared to non-verbal tasks, weak expression of intellectual interests (for reading stories and fairy tales, for plot games, etc.), and difficulties in memorizing children's poems and songs, i.e. in the form of partial disorders. In addition, diffuse neurological symptoms of 5 or more neurological signs were detected.
The psychomotor level of neuropsychic response, from 3 to 10 years (according to V.V. Kovalev, 1995), determines the dynamics of mental disorders [22]. The change from the somatovegetative level to the psychomotor level causes the manifestation of psychomotor syndromes while maintaining the manifestations of the neuropathic symptom complex. These include, first of all, hyperkinetic (hyperdynamic) syndrome, systemic disorders of childhood (stuttering, tics, enuresis, etc.). Table 6 shows mental disorders at the age of 3.5 years in 1 subgroup.
Table 5.
The structure of mental disorders in children aged 3.5 years who underwent PCNSL
| Mental disorders | 1 subgroup (n=88) | P1-2 | P1-3 | |
| Abs | (M±m,%) | |||
| Neuropathic syndrome | 80 | (93±3) | 0,0001 | 0,0001 |
| Psychoorganic syndrome | 17 | (20±4) | 0,004 | 0,003 |
| Sleep disorders | 57 | (66±5) | 0,0001 | 0,0001 |
| Bruxism | 12 | (14±4) | 0,015 | 0,125 |
| Neurosis-like enuresis, mild course | 28 | (33±5) | 0,0001 | 0,0001 |
| Neurosis-like enuresis | 11 | (13±4) | 0,018 | 0,016 |
| Neurosis-like stuttering | 7 | (8±3) | 0,052 | 0,046 |
| Specific speech articulation disorders (SAD) | 37 | (43±5) | 0,009 | 0,0001 |
| Impaired activity and attention | 29 | (34±5) | 0,0001 | 0,001 |
| Mixed specific disorders of emotion and behavior | 15 | (17±4) | 0,006 | 0,005 |
| Hyperdynamic syndrome | 4 | (6±4) | 0,109 | 0,092 |
When studying correlation relationships, it was possible to establish that children with mental disorders were in significant need of treatment (r=0.77, p<0.0001). Mental disorders had a high correlation with neuropathic syndrome r=0.75 p<0.0001.
It should be noted that in subgroup 2 and control group 3, by the age of 3-3.5 years, neuropsychic disorders and deviations in mental development were not detected.
Mild psychoneurological disorders were compensated by timely and long-term neurometabolic therapy, speech therapy, pedagogical and psychological correction. Children were subject to social requirements appropriate to their age and abilities.
Conclusion
The pathogenic influence of intrauterine and intrapartum hypoxia of mild and moderate severity (hypoxic-ischemic damage to the central nervous system of mild and moderate severity) causes the formation of mental disorders in the form of a neuropathic symptom complex in children under 3 years of age.
Preventive measures to prevent the formation of these neuropsychiatric disorders include timely treatment of mothers during pregnancy to reduce fetal hypoxia, adequate management of childbirth, continuous monitoring of children by neurologists after birth for at least three years, further advisory supervision by a child psychiatrist of preschool age.
In the case of diagnosing these disorders as consequences of perinatal damage to the central nervous system, it is advisable to use multiprofessional intervention with the participation of a pediatrician, neurologist, psychiatrist, speech therapist, psychologist and psychotherapist.
L.V. Yusupova, K.Yu. Retyunsky
Ural Research Institute for Maternity and Infancy Protection, Ekaterinburg
Ural State Medical Academy, Ekaterinburg
Liliya Vagizovna Yusupova - correspondence graduate student, psychiatrist, junior researcher at the Department of Biophysical Research Methods of the Research Institute of Maternity and Infancy Protection
Literature:
1. Barashnev, Yu.I. Key problems of perinatal neurology / Yu.I. Barashnev // Obstetrics and gynecology. - 2007. - No. 5. - P. 51-54.
2. Haan, HH Experiments in perinatal brain injury: What have we learned? / HH Haan, AJ Gunn, PD Glukman // Prenatol. and Neonatol. Med. - 1996. - No. 1. - P. 16-25.
3. Schlighting, R. Defining the hypoxic threshold / R. Schlighting, MR Pinsky // Crit. Care Med. - 1991. - No. 2. - P. 147-149.
4. Romero, R. Prenatal medicine: the child is the father of the man / R. Romero // Prenatol. and Neonatol. Med. - 1996. - No. 1. - P. 8-11.
5. Longo, L.D. Hypoxia ischemia and the developing brain: Hypotheses regarding the pathophysiology of fetal neonatal brain damage / L.D. Longo, S. Pachianathon // Brit. J. Obstet. Gynaec. - 1997. - No. 104. - P. 652-662.
6. Volpe, JJ Brain injury in the premature infant current concepts / JJ Volpe // Prev. Med. - 1994. - No. 23. - P. 638-645.
7. Saxena, Sh. Prevention of mental and behavioral disorders: implications for policy and practice / Sh. Saxena, E. Jané-Llopis, Cl. Hosman // J. World Psychiatry (translated from English in the Review of Modern Psychiatry. - 2005. - No. 27. - 1. - P. 14). - 2006. - No. 5 (1). — P. 5-10.
8. Volodin, N.N. Perinatal medicine: problems, ways and conditions for their solution / N.N. Volodin // Pediatrics. - 2004. - No. 5. - P. 18-23.
9. Filkina, O.M. Perinatal lesions of the nervous system and their consequences in children: clinical picture, prognosis, diagnosis, prevention and correction, somatic health / O.M. Filkina, T.V. Bowl, N.Y. Sotnikova [et al.]. — Ivanovo: Ivanovo. - 2007. - 240 p.
10. Yatsyk, G.V. Rehabilitation of newborn children with perinatal pathology - prevention of health disorders in adolescence / G.V. Yatsyk, R.S. Zainiddinova // Russian Pediatric Journal. - 2011. - No. 5. - P. 4-7.
11. Goryunova, A.V. Approaches to diagnosing cognitive deficits in infants / A.V. Goryunova, O.I. Maslova, V.M. Studenikin [etc.] // Materials of the IX Congress of Russian Pediatricians “Current Problems of Pediatrics”. - Moscow, February 10-12, 2004. - T. 3 (Appendix 1). — P. 112.
12. Mikirtumov, B.E. Clinical psychiatry of early childhood / B.E. Mikirtumov, A.G. Koshchavtsev, S.V. Buckwheat. - SPb.: Peter. - 2001. - 256 p.
13. Bazhenova, O.V. On the prevention of mental pathology at an early age / O.V. Bazhenova, G.V. Kozlovskaya // Journal of Neurology and Psychiatry named after. S.S. Korsakov. - 1993. - No. 3 (93). — P. 35-37.
14. Mendelevich, B.D. Mental disorders and behavioral disorders of children in the Russian Federation / B.D. Mendelevich, R.N. Terletskaya // Russian Pediatric Journal. - 2009. - No. 5. - P. 41-45.
15. Gurovich, I.Ya. Mental health of the population and psychiatric care in Russia / I.Ya. Gurovich // XIII Congress of Psychiatrists of Russia (congress materials). - M., 2000. - P. 13-14.
16. Butorina, N.E. Residual organic psychosyndrome in clinical psychiatry of childhood and adolescence / N.E. Butorina. — Chelyabinsk: ATOXO. - 2008. - 192 p.
17. Butorina, N.E. General psychopathology in child and adolescent psychiatry (reference book) / N.E. Butorina. — Chelyabinsk: ATOXO. - 2007. - 210 p.
18. Dmitrieva, T.B. Mental health and societies: new challenges and threats. // Materials of the scientific and practical conference “Mental health and public safety” (Ekaterinburg, June 6, 2008) / T.B. Dmitrieva. - Ekaterinburg: IRA UTK, 2008. - P. 3-8.
19. Zvereva, Z.V. On the issue of neuropsychic health of young children. // Materials of the IX Congress of Pediatricians of Russia (Children's healthcare in Russia: development strategies, February 19-22, 2001, Moscow) / Z.V. Zvereva. - M., 2001. - P. 224.
20. Zabramnaya, S.D. Methodological recommendations for the manual “Practical material for conducting psychological and pedagogical examination of children” / S.D. Zabramnaya, O.V. Borovik. — M.: Vlados. - 2002. - 48 p.
21. Carlberg, C. Business analysis with Excel 2000. - Que Corporation, 1996. (Carlberg K. Business analysis with Excel 2000 / C. Carlberg // Textbook. - translated from English - M.: Williams, 2000. - 480 p.
22. Makarova, N.V. Statistics in Excel (textbook) / N.V. Makarova, V.Ya. Trofimets. - M., Finance and Statistics, 2002. - 368 p.
23. Guryeva, V.A. Psychogenic disorders in children and adolescents / V.A. Guryev. - M.: Kron-Press, 1996. - 208 p.
24. Kovalev, V.V. Childhood psychiatry: A guide for doctors: ed. 2nd, revised and additional / V.V. Kovalev. - M., Medicine. - 1995. - 560 p.
Causes of neuroses
The causes of neuroses can manifest themselves in childhood, when a birth injury occurred or an illness suffered in infancy. There can be several reasons for the manifestation of neuroses:
- Diseases of the nerves and psyche. This could be epilepsy with periodic seizures, schizophrenia, etc. A patient with such health problems is constantly treated and monitored by his doctor.
- Pathologies of brain development. These may be congenital disorders or acquired due to injury.
- Chronic infectious diseases. They, like nothing else, expose the nervous system to constant attacks. After all, when there are disturbances in the body, all functions suffer, making a lot of effort to get rid of the constant irritant.
- Diseases of the heart, blood vessels, gastrointestinal tract.
- Early drinking and smoking in adolescence. Often those people who in childhood indulged in alcohol and smoked around the corners of the school then suffer throughout their lives from neurotic attacks and unstable states of the nervous system, since it was disrupted during its most important period of development.
Therapy for TR
Treatment of TD in children and adolescents is based on an integrated approach using methods of psychotherapy (rational, cognitive-behavioral, family, play, etc.) and pharmacotherapy. An important role belongs to parents who, following the recommendations of a specialist, help their child cope with anxiety. When coping skills and courageous behavior are practiced and encouraged at home, children and adolescents learn to face their fears, take smart risks, and gain confidence in their own abilities.
In pharmacotherapy, drugs of several groups are used, including non-benzodiazepine tranquilizers (hydroxyzine), tranquilonotropics (aminophenylbutyric acid hydrochloride), drugs with sedative and vegetative-stabilizing effects (affinity-purified antibodies to the brain-specific protein S-100), selective serotonin reuptake inhibitors (fluvoxamine, sertraline), mild antipsychotic drugs (alimemazine), herbal medicines. It should be noted that there is a need for long-term medical supervision and long-term therapy.
For children and adolescents with various forms of TR, complex medications may be recommended, including neurometabolic agents, vitamins, macro- and microelements. Such a drug is “KidZ syrup with lemon balm and mint,” which is prescribed in courses of 2 weeks. in the following doses:
child from 3 to 7 years old - 5 ml 2 times a day;
child from 7 to 11 years old - 5 ml 3 times a day;
for a child over 11 years old - 10 ml 2 times a day.
The composition of the drug “KidZ syrup with lemon balm and mint” includes useful and safe components (B vitamins, amino acids, magnesium, zinc and plant extracts) that normalize the functioning of the nervous system, restoring the natural balance between the processes of excitation and inhibition:
lemon balm and mint in the form of extracts help eliminate nervous tension;
choline (a precursor to the neurotransmitter acetylcholine) is involved in the formation of components of brain tissue, helps improve memory and performance;
glycine has a beneficial effect on motor skills and speech, helps reduce psycho-emotional stress, aggressiveness, and conflict;
lysine protects brain cells from oxygen starvation, slows down excitation processes;
vitamin B1 (thiamine) ensures metabolic processes in the central nervous system (CNS), affects the functions of neurotransmitters (acetylcholine, GABA), the processes of nerve impulse conduction;
vitamin B3 (niacin, nicotinamide) ensures the occurrence of redox processes in the body and the normal functioning of the central nervous system;
vitamin B6 (pyridoxine) is involved in the biosynthesis of neurotransmitters (GABA, serotonin, catecholamines, etc.);
magnesium is a central element that maintains the balance of excitation and inhibition processes in the central nervous system. Magnesium is necessary to stabilize the activity of excitatory (glutamate) receptors. It is a cofactor of adenylate cyclases involved in signal transmission from dopamine, serotonin and adrenaline receptors to control intracellular cascades, as well as a cofactor of catechol-O-methyltransferase, which inactivates excess monoamine neurotransmitters;
magnesium and vitamin B6, when administered together, help improve behavior, reduce anxiety and aggressiveness, and increase concentration;
zinc is involved in ensuring mental processes, since it is part of all known classes of enzymes and is involved in the metabolism of proteins, fats, carbohydrates and nucleic acids. Zinc is necessary for the processes of neuroontogenesis, is part of brain metalloproteins that have neuroprotective properties, and is involved in the mechanisms of learning and memory.
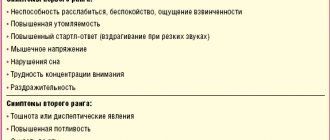
Symptoms
The symptoms of all neurotic conditions and stable neuroses are very similar, since they all manifest themselves in a similar way.
This may be emotional instability, when the mood “jumps” from plus to minus and vice versa. It is always strange to observe this in adults, which indicates the presence of a problem that needs to be treated with medication. Manifestation of anxiety, when everything is outwardly good and calm, irritability towards surrounding people and circumstances indicate a disorder of the nervous system. It becomes difficult for adults to control not only their internal feelings, but even their behavior, as unjustified aggression increasingly begins to manifest itself and take its place in life. These include fears, suspiciousness about health, the desire to cry for no reason. Physical symptoms include problems with the intestinal tract, constipation and diarrhea with a normal healthy diet. Reluctance to eat food, insomnia during night rest, daytime apathy and lethargy, vomiting, changes in pulse and blood pressure disturbances may also occur. It is not necessary to have all of these symptoms for a clear diagnosis to be made. It is enough to have several in intense manifestation.
Introduction
Anxiety disorders (AD) are one of the most common reasons for visiting doctors and are often encountered in the clinical practice of pediatricians and pediatric neurologists.
It should be noted that until now, some specialists in the process of monitoring children and adolescents with TD continue to use such formulations as “neurotic conditions”, “neurotic reactions”, “neurosis-like syndrome”, and often incorrectly use the concepts of “asthenia”, “neurasthenia” , "asthenic neurosis". The listed terms do not correspond to the definitions of TR in the classifications of recent years [1, 2], as well as to modern ideas about the nature of TR. According to epidemiological studies, the overall incidence of all TDs in children and adolescents varies from 9 to 32% and is characterized by an increase as children grow older [3]. In the majority of adult patients with emotional and affective disorders, the first symptoms manifested in childhood or adolescence, and these were manifestations of TD [4, 5]. Thus, the formation of the clinical picture of TR occurs gradually. However, in many children and adolescents, TR remains unidentified for a long time, which leads to a lack of specialized care and drug therapy, and subsequently, the chronicity of TR.
Let us dwell on the features of the manifestations of TD in children and adolescents. It should be noted that some patients may simultaneously experience symptoms of not one, but several forms of TR. In addition, TD can act as both an independent and concomitant condition in many diseases of the nervous system in children, including disorders of speech development and school skills, attention deficit hyperactivity disorder, primary headaches (especially tension headaches), epilepsy, consequences perinatal lesions of the nervous system, traumatic brain injuries, neuroinfections, autism spectrum disorder, etc.
TR is a group of syndromes of emotional disorders that are characterized by intense and prolonged anxiety, subjective feelings of anxiety, tension, gloomy forebodings, the experience of damage, as well as the appearance of unusually strong fear - irrational and not consistent with the content of the situations or objects that cause it [4, 6–9] .
How do neurosis-like conditions differ from neuroses?
Despite the fact that both neurosis-like conditions and neuroses are very similar to each other in manifestations and symptoms, they still differ.
And the differences lie in the reason for their appearance, since this is the whole point. Neuroses usually affect the nervous system after it has been completely exhausted by frequent blows to it, stressful situations and great physical and nervous strain. All moments and factors that exhaust a person and force him to work for wear, both physically and mentally, contribute to the manifestation of neuroses. After all, because of this, an anxious state appears, a violation of the autonomic system, and so on. Neurosis-like conditions usually do not manifest themselves due to psychological disorders. They do not have stress or problematic nervous breakdowns at their root. They usually appear due to internal organic diseases that can be established from the moment of development in the womb. It could even be a mild form of cerebral disorder, which gives rise to all the different types of syndromes during the life and functioning of the human body after birth. Sometimes neurosis-like conditions can be acquired and manifest themselves against the background of severe diseases that have an infectious nature and a chronic form.
Features of symptoms
A neurosis-like condition in children can be suspected if the following symptoms are present:
- hyperactivity, attention deficit, increased emotional excitability;
- nightmares, fears, phobias;
- attacks of aggression, tearfulness;
- decreased tone, weakness;
- tics, stuttering, enuresis;
- constipation or diarrhea;
- nausea, vomiting;
- increased sweating or dry skin.
In adults, the syndrome has the following symptoms:
- rapid mood changes, increased anxiety and irritability, predominance of negative emotions;
- the emergence of difficulties in controlling behavior, aggression, and temper;
- vomiting and nausea during stress;
- diarrhea and constipation;
- increased fatigue;
- drowsiness, insomnia, nightmares;
- lack of appetite;
- a sharp increase and decrease in heart rate and blood pressure;
- suspiciousness, anxiety, unreasonable fears;
- sweating and tearfulness;
- enuresis.
The patient does not have to have all the symptoms on the list. In each specific case, the number and intensity of symptoms differs.
Treatment methods
In order to effectively cure neurosis or a neurosis-like condition, you should avoid as much as possible everything that injures the nervous system and psyche. To begin with, a comprehensive diagnosis is carried out, which includes tomography, consultation with a neurologist, electroencephalogram, as well as examination by many specialists, such as a cardiologist, gastroenterologist and others. This is necessary in order to understand the true cause of the disease and find out whether it lies in diseases of other organs. Neuroses are treated with medication. They take sedatives, also those that affect blood pressure and normalize it. In addition to medications, physical procedures are necessary, without which general treatment may become ineffective. This is electrosleep, physiotherapy in the form of electrophoresis. Neurosis can be cured with the help of psychotherapy, in contrast to neurotic conditions, where treatment should all be aimed at physiology. It is definitely worth including therapeutic exercises, since without sports it is impossible to get rid of many problems even with the nervous system, not to mention diseases of the body. You shouldn’t overload yourself: you should follow the correct regime so that your rest is complete and constant. You should also eat healthy and forget about snacking. Sometimes it makes sense to go to a sanatorium for treatment, changing the environment, which will be very useful for the nervous system. It is advisable to protect yourself from stress and, if possible, quit an annoying job, change your social circle and forever forget about bad habits, which, like nothing else, negatively affect the nerves.
The influence of sport on the body during neurosis
There are many cases when people with neurosis are simply afraid to create sports activities for themselves, so as not to cause frightening symptoms and aggravate the course of the disease.
Usually they are frightened by physical signs, such as an accelerated pulse, rapid breathing, sweating, which in fact is a common occurrence in sports even in completely healthy people. But those who suffer from obsessions often mistake natural manifestations for signs of panic syndrome. Therefore, sport becomes a forbidden activity for neurotics. In fact, such a judgment is extremely wrong. Indeed, due to the absence of the slightest load, the body becomes weak and sluggish, the muscles lose their shape, and the nervous system becomes more vulnerable to various kinds of stress. Naturally, not every sport is beneficial for neurotics. Difficult, dangerous and overly active sports activities can damage the psyche and regularly create traumatic situations. The body will quickly wear out and be subject to stress. Therefore, it is worth engaging in such varieties that do not pose any danger, are simple and enjoyable loads. This includes cycling, skiing and skating, playing tennis, slow running, and also swimming and aerobics with a light program.
You shouldn’t immediately rush into big sports and overload yourself with exorbitant activities. This will only make the condition worse. To begin with, you can generally do ordinary exercises, but do the exercises every day so that a positive habit is developed, and the body can quickly feel the comfort of such a lifestyle.