Medulloblastoma is a malignant brain tumor located in the cerebellar hemispheres, but most often the location of medulloblastoma is the cerebellar vermis.
It primarily affects children under 10 years of age; there are rare cases of this tumor in adults.
Features of medulloblastoma: in children it is a common tumor among brain cancers; childhood medulloblastoma is characterized by rapid growth and metastasis. Medulloblastoma is more often diagnosed in boys. In adults, when medulloblastoma is detected, the tumor is usually small in size and practically does not metastasize. A tumor in patients over 20 years of age is a rare occurrence. Perhaps due to the absence of any symptoms.
The causes of this tumor are unknown, but certain risk factors have been identified that increase the likelihood of developing medulloblastoma:
- Viral infections (herpes virus, cytomegalovirus, infectious mononucleosis).
- Genetic diseases that often accompany medulloblastoma (Gorlin-Goltz syndrome, Maffucci syndrome, Turcot syndrome, Cowden disease).
- Ionizing radiation.
- Carcinogens (food, household).
Symptoms
With further growth, the tumor grows into the cavity of the fourth ventricle, which can lead to closure of the spinal canal and disrupt the outflow of cerebrospinal fluid. When growing into the brain stem, the medulla oblongata, where the corresponding centers that regulate many functions in the body are located, the tumor leads to a clear clinical picture, which depends on which structures the tumor affects.
This may be developed strabismus in a child, nystagmus, severe headaches, nausea, vomiting, and swallowing problems. Depending on the growth of the tumor, the presence of metastases and closure of the spinal canal, the symptoms of medulloblastoma are characterized by hydrocephalus or hydrocephalus of the brain. In infants and children of the first year of life, due to these processes, the size of the head increases.
One of the first signs of medulloblastoma may be ataxia (cerebellar disorder), that is, imbalance when walking, unsteadiness of gait. Small children may refuse to walk, crawl, or ask to be held.
According to modern views, medulloblastoma is a heterogeneous group of diseases characterized by clinical, histological and molecular features in patients of different ages [3, 11, 12, 14, 21-23, 31]. A special group of medulloblastomas consists of tumors in children under 3 years of age due to limitations in the possibility of radiation treatment [2, 10].
In the period from 2000 to 2010, in the Department of Pathological Anatomy of the Federal State Budgetary Institution Research Institute of Neurosurgery named after. acad. N.N. Burdenko" RAMS diagnosed 51 cases of primary medulloblastoma in children under 3 years of age. The number of cases increased annually: from 1 in 2000 to 14 medulloblastomas operated on in 2010, which is most likely due to improved diagnosis of these tumors in the early stages by outpatient pediatricians, improvement of neurosurgical techniques and increased qualifications of neurosurgeons [1]. The first symptom of the disease, due to age, was the loss of previously acquired skills. Symptoms of hydrocephalus were also often observed; the period between the first manifestations of the disease and diagnosis averaged 2-3 months. In more than half of the cases, the tumor occurred in children aged 2-3 years, most often affecting boys.
Material and methods
Clinical characteristics of the patients are presented in Table. 1.
To exclude an atypical teratoid rhabdoid tumor, an immunohistochemical study was performed in all cases with the Anti-BAF47 antibody BD Transduction Laboratories clone 25/BAF47 at a dilution of 1:200. An immunohistochemical study was also performed with the BD Transduction Laboratories Anti-β-catenin antibody at a dilution of 1:100. To investigate possible quantitative changes on chromosomes, fluorescent in situ hybridization was performed with the following commercial Vysis Abbott Molecular probes: Vysis LSI MYC Dual Color Break Apart Rearrangement Probe, Vysis LSI N-MYC (2p24) Spectrum Green/CEP 2 Spectrum Orange Probe, Vysis Miller -Dieker Region/Isolated Lissencephaly Probe LSI LIS1 Spectrum Orange/LSI RARA Spectrum Green, Vysis LSI MYB Spectrum Aqua Probe, Vysis LSI BCR/ABL + 9q34 Tricolor, Dual Fusion Translocation Probe.
Data on molecular group membership (groups SHH[], WNT[], C and D [31]), determined by the “four antibody” immunohistochemical method [23], were kindly provided by Prof. A.G. Korshunov (Department of Neuropathology, University of Heidelberg, Heidelberg, Germany). Molecular group data are known for 47 patients.
results
The predominant histological variant in the age group under 3 years was desmoplastic/nodular medulloblastoma (Fig. 1),
Figure 1. Desmoplastic/nodular medulloblastoma. Here and in Fig. 2 and 3: hematoxylin and eosin staining. ×200. which occurred in 24 (57%) children.
We also observed 5 cases of medulloblastoma with increased nodularity (Fig. 2),
Figure 2. Medulloblastoma with increased nodularity. occurring exclusively in the age group under 3 years.
The second most common type after the desmoplastic/nodular type was classical medulloblastoma, observed in 15 (29%) cases (Fig. 3),
Figure 3. Classic type medulloblastoma.
and in 7 (14%) children, medulloblastoma demonstrated large cell/anaplastic histology (Fig. 4).
Figure 4. Large cell/anaplastic medulloblastoma.
Fluorescent in situ hybridization performed in all cases revealed two amplifications of the MYC oncogene (Fig. 5),
Figure 5. Amplification (increase in copy number) of the MYC oncogene.
Red signals are MYC (8q24 locus), green signals are the centromeric probe of chromosome 8 (CEP8). amplification of the MYCN oncogene (Fig. 6)
Figure 6. Amplification (increase in copy number) of the MYCN oncogene.
Green signals - MYCN (locus 2p24) red signals - centromere probe chromosome 2 (CEP2). in 4 patients, isochromosome 17q (Fig. 7)
Figure 7. Isochromosome 17q - increase in the number of copies of 17q and simultaneous loss of one copy of 17p.
Green signals are 17q, red signals are 17p. in 8. We also observed a deletion of 9q (Fig.
Figure 8. 9q deletion (loss of one copy of 9q) - one confluent red-blue signal from 9q. Red and blue signals are 9q, green signals are 22q. in four desmoplastic/nodular medulloblastomas.
Information on identified aberrations on chromosomes 2p, 8q, 9q and 17q is presented in Table. 2.
Kaplan-Meier analysis of the survival of medulloblastomas in children under 3 years of age showed that desmoplastic/nodular medulloblastoma has a favorable prognostic value only for relapse-free survival (Fig. 9),
Figure 9. Impact of histologic type of medulloblastoma on disease-free survival in children <3 years of age.
which was confirmed by the regression model Cox (Fig. 10).
Figure 10. Impact of histological type of medulloblastoma on disease-free survival in children under 3 years of age (Cox regression model).
It was also revealed that medulloblastomas belonging to the molecular group SHH demonstrate the most favorable rates of overall and relapse-free survival (Fig. 11, 12),
Figure 11. Effect of medulloblastoma molecular group on disease-free survival in children <3 years of age.
Figure 12. Impact of medulloblastoma molecular group on overall survival in children <3 years of age.
regression model Cox (Fig. 13)
Figure 13. The influence of the molecular group of medulloblastoma on relapse-free survival in children under 3 years of age (regression model Cox). confirmed data only for disease-free survival.
The influence of clinical factors (gender, age of the patient, tumor location, degree of resection and M status) and genetic aberrations on survival rates was unreliable.
We analyzed lethal outcomes depending on molecular group membership (Fig. 14)
Figure 14. Analysis of mortality in children under 3 years of age with medulloblastomas depending on molecular group.
and clinical and morphological factors (data are summarized in Table 3).
It turned out that group C showed the most unfavorable indicators - the mortality rate in it was 50%, in group D - 17%, and the most favorable prognosis was the SHH group with the lowest mortality rate - 13%.
Discussion
Our cohort of medulloblastomas in children under 3 years of age consisted of 51 tumors collected over a 10-year period at the Federal State Budgetary Institution Research Institute of Neurosurgery of the Russian Academy of Medical Sciences, which is one of the largest series of such tumors described in the literature. The largest series of 96 medulloblastomas, described by D. Johnston et al. [10], is a panel of 17 Canadian medical centers from 1990 to 2005.
According to our data, the predominant histological variant of medulloblastoma in young children is desmoplastic/nodular medulloblastoma, which is characterized by aberrant regulation of the SHH signaling pathway and can develop from progenitor cells of the external granular layer of the cerebellum [8], as well as from the cochlear nucleus of the brain stem [9 ]. Some authors [8] emphasize the direct connection between the desmoplastic/nodular histological type and the localization of the tumor in the cerebellar hemisphere, but in our series, in the vast majority of cases, we encountered midline localization of the tumor, less often the tumor affected the vermis and the cerebellar hemisphere, and pure localization of medulloblastoma in the hemisphere cerebellum was observed in only 8% of cases, despite the fact that desmoplastic/nodular histology occurred in 57%.
We also observed 2 unique cases of metastasis of desmoplastic/nodular medulloblastoma at similar times (approximately 1 year after tumor removal) in boys of the same age (about 2 years), one of them died 20 months after surgery from disease progression.
The frequency of aberrations we identified (amplification of MYC or MYCN oncogenes, isochromosome 17q) in the group of medulloblastomas in children under 3 years of age, according to the literature [21, 24], is not very different from the detected quantitative changes on chromosomes in older children with medulloblastomas. A strict correlation with a fatal outcome was shown by the combination of large cell/anaplastic medulloblastoma with amplification of the MYC oncogene and isochromosome 17q detected in 4% of cases - both patients died after 6 and 18 months, respectively, from disease progression.
Amplification of the MYCN oncogene was 2 times more common in 8% of cases and was also combined with isochromosome 17q, but such tumors more often showed desmoplastic/nodular histology and a relatively favorable outcome. The prognostic value of MYCN oncogene amplification has not yet been determined, A. Korshunov et al. [13] showed the biological heterogeneity of medulloblastomas with MYCN oncogene amplification that do not belong to the SHH subgroup, identifying favorable (a combination of MYCN oncogene amplification and 10q deletion) and unfavorable (only MYCN oncogene amplification with a balanced 10q profile) subgroups.
The 9q deletion occurs exclusively in desmoplastic/nodular medulloblastomas with its distinctive feature being the deletion of the PTCH1 gene (9q locus). This aberration is found in 8% of cases, although some researchers [21] describe an incidence of more than 50%.
Among 51 medulloblastomas, we were not able to detect 6q deletion or nuclear expression of β-catenin in any case, which is consistent with the data of M. Kool [11] and M. Taylor [31] on the absence of the WNT group in children of different ages.
Summarizing all of the above, it becomes clear that the desmoplastic/nodular histological type is the most common variant of medulloblastoma in young children, on the one hand, it suggests a good result [16, 28] - the 5-year relapse-free survival rate in our series was 76%. For the most favorable prognostic variant of a desmoplastic/nodular tumor—medulloblastoma with increased nodularity—the possibility of maturation into well-differentiated ganglion tumors has been described [6, 7], but on the other hand, it is desmoplastic/nodular medulloblastomas that arise in Li-Fraumeni syndrome [17, 18 , 25], they describe the phenomena of chromothripsis, characterized by multiple amplifications of oncogenes such as MYCN, GLI2 and CDK6 [25]. Also, desmoplastic/nodular medulloblastomas can occur with Gorlin syndrome [18, 30]. Radiation therapy for such tumors is complicated by the development of secondary nevoid basal cell carcinoma at the site of previous irradiation [29].
Children under 3 years of age are considered to have poorer survival rates than older children. And the reason is either the more aggressive biology of medulloblastoma in very young children, or the fact that radiation therapy is not included in the treatment protocol [19, 20] due to its ability to cause neuroendocrine disorders (growth hormone deficiency, gonadal damage, hyper- and hypofunction of the thyroid gland , nodules in the thyroid gland, hyperprolactinemia, adrenocorticotropic hormone deficiency, osteopenia, osteoporosis, obesity, lipid metabolism disorders and metabolic syndrome) and neurocognitive consequences (decrease in IQ, ability to master oral language, reading, writing and mathematics, disorders short-term and long-term memory), as well as hearing impairment, visual impairment, kyphosis, vertebral demineralization and secondary tumors, especially in Turcot and Gorlin syndromes [15, 20, 26].
For the treatment of desmoplastic/nodular medulloblastoma without metastases at the time of diagnosis in children under 3 years of age, according to studies by S. Leary et al. [16] and S. Rutkowski [27], a fairly intensive chemotherapy regimen without the use of radiation therapy, methotrexate or high-dose chemotherapy with stem cell support.
Patients with anaplastic/large cell medulloblastoma and initial metastatic disease should receive high-dose chemotherapy and craniospinal irradiation [20].
Although, according to some authors [4, 10], young children who received radiation therapy demonstrate higher survival compared to children treated without the use of this modality. Against this background, the development of modern radiation therapy regimens looks promising [5].
Conclusion
The present study clearly demonstrated that desmoplastic/nodular medulloblastoma predominates in children <3 years of age and has a favorable prognostic value only for disease-free survival. Radiation therapy for desmoplastic/nodular medulloblastoma in children under 3 years of age can only be used to treat relapses.
Another biological feature of medulloblastomas in children under 3 years of age is their lack of nuclear accumulation of β-catenin and deletion of chromosome 6q. Medulloblastomas with MYCN oncogene amplification more often demonstrate desmoplastic/nodular histology and a relatively favorable outcome. The most unfavorable prognosis is the detection of amplification of the MYC oncogene; such tumors should be included in the “high-risk” protocol.
A comment
This article is interesting primarily because it analyzes the relationship of the histological and genetic types of medulloblastomas in children under 3 years of age with follow-up data, primarily with relapse-free survival of patients. Of course, it has been known for a very long time that different histological types of medulloblastomas behave differently and have different prognoses. Recently, works have begun to appear devoted to the study of genetic groups of medulloblastomas, their relationship with the clinical course, as well as the identification of unfavorable and relatively favorable genetic anomalies. In particular, a detailed study of the molecular genetic features of medulloblastomas was carried out in the dissertation work of M.V. Ryzhova, the author of this article. The correlation of genetic groups, histological types and follow-up data in the study of medulloblastomas has not yet been reflected in the domestic periodical scientific literature. And although the connection between genetic damage, histological picture and clinical course is not always obvious (some mutations are detected in different histological groups, often in combination, etc.), in most cases a clear relationship is determined between the identified molecular group and the prognosis. Thus, the SHH group, according to the authors, showed the best result in both overall and disease-free survival.
In addition, I would like to note a truly very large group of medulloblastomas studied in young children. An interesting fact is that, according to the results of this work, the predominant type of medulloblastoma is desmoplastic/nodular, while according to various modern literature data, the variant with increased nodularity prevails in children under the age of 2-3 years.
I think that this article will be very useful for specialists, primarily neuro-oncologists and neuropathologists, as it contains fairly concentrated information about the genetics and pathohistology of medulloblastomas in young children and their connection with patient survival.
A.N. Kislyakov
(Moscow)
[]SHH - Sonic Hedgehog. The name Sonic Hedgehog is a joke among molecular geneticists; the molecular cascade is named after a computer game character.
[]WNT is a combination of Wg (wingless) and Int. The Drosophila wingless gene was originally identified by a recessive mutation that suppresses the development of wings in the fly. The homologous vertebrate gene Int1 (Integration1) was first studied due to the presence of several sites of integration of the mouse mammary cancer virus genome in its locus.
Differential diagnosis
It is most common among tumors in children, but before making a final diagnosis, it is necessary to exclude diseases that are similar to medulloblastoma.
Among pediatric pathologies this may be:
- Brain ependymoma is a benign tumor that develops from the cells lining the ventricles of the brain and the spinal cord canal.
- hairy astrocytoma.
- Choroid papilloma.
In adults, these may be cerebellar metastases, ependymoma, choroidpapilloma and hemangioblastoma.
Diagnostics
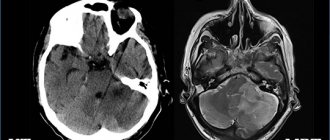
If a brain tumor is suspected, a general blood test and biochemistry, consultation with an ophthalmologist with a mandatory fundus examination, neurosonography (NSG) or ultrasound of the brain for infants, children under 3 years of age, CT or MRI to detail the size and location of the brain tumor are mandatory. brain, as well as the spinal cord to exclude metastasis, positron emission tomography (PET) to identify regional and distant metastases.
Carrying out a stereotactic biopsy will help to make a final diagnosis, determine the type of medulloblastoma and develop further, but individual, treatment tactics.
Stereotactic biopsy is performed under general anesthesia and is applied using a stereotactic frame or using neuronavigation. If a stereotactic frame is used, a CT or MRI scan is performed during the operation.
With neuronavigation, MRI and CT are done before surgery, and then at the time of biopsy, a 3D image is made from the pictures. The needle used for biopsy is equipped with a microvideo camera. Everything is done in order to take the desired piece of tissue as accurately as possible and minimize complications after the biopsy. Stereotactic biopsy is a complex operation that requires experience from the doctor.
Diagnosis of medulloblastoma in Israel: accurately, quickly, competently
The most important point in successful treatment is an accurate diagnosis. Diagnostic procedures take only a few days at the Assuta clinic.
The first day of diagnosis - meeting the doctor
The attending physician examines the patient on the first day of the patient's arrival at the clinic. After filling out all the necessary documents for treatment, as well as studying the medical history, the doctor sends the patient for a comprehensive examination.
The second day of diagnosis - undergoing procedures
To diagnose medulloblastoma, the Assuta Clinic in Israel carries out the following diagnostic measures:
- general blood test, as well as biochemistry;
- Analysis of urine;
- CT scans in combination with MRI provide a complete picture of the location of the tumor, as well as the presence of metastases in the body;
- biopsy. To make an accurate diagnosis, this analysis is simply irreplaceable at the Assuta clinic. A small area of the affected tissue undergoes histological examination in the clinic laboratory. However, patients do not always undergo a biopsy within the walls of an Israeli clinic: some patients come to Israel with biopsy slides performed in their homeland. If Israeli doctors recognize the results as adequate, a repeat biopsy is not performed.
Third day of diagnosis - results
As soon as all the results are ready, doctors begin to study them. Oncologists, neurosurgeons and even psychologists collectively decide on a treatment regimen. In the future, these specialists carefully monitor the treatment process, having the opportunity to adjust it if necessary.
Thousands of people from all over the world who have already undergone treatment for medulloblastoma in Israel within the walls of the Assuta clinic are immensely grateful to Israeli doctors. This is confirmed by the huge number of reviews left by former patients of the Assuta clinic. In their reviews, people write not only about the quality of treatment provided, but also about the excellent attitude of the medical staff towards patients, and the excellent living conditions in the clinic. Indeed, the level of medical care at the Assuta clinic reaches the highest levels. Therefore, even patients from developed countries come to Israel for treatment of medulloblastoma.
Treatment of medulloblastoma
The surgical treatment method aims to completely remove the tumor; stage-by-stage removal is possible (in several operations or in stages if it was not possible to immediately remove the entire tumor focus). This is what a neurosurgeon does.
After the operation, the child is transferred to oncologists who carry out radiation therapy and chemotherapy. Radiation therapy is carried out for children over 3 years of age; the brain and spinal cord are irradiated to prevent the development of metastases. Chemotherapy is used in complex treatment with other methods, as well as for palliative (making life easier) for the patient.
The approach to each patient is individual and depends on many factors.