DlyaSerdca → Drugs → Afobazole or Novopassit – what to choose?
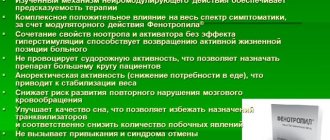
Afobazole is a simple daytime psychotropic drug characterized by an activating and anti-anxiety effect.
Unlike other analogues, neither physical nor psychological dependence is formed on it, and after the end of the course of treatment, withdrawal syndrome does not appear.
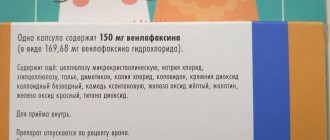
The active substance in Afobazole is morpholinoethylthioethoxybenzimidazole dihydrochloride - an anxiolytic that relieves tension, anxiety, neuroses and irritating weakness.
Allows you to escape from the oppressive feeling of threat and adapt to a new team. A distinctive feature is that it does not cause drowsiness or delayed reactions. On the contrary, when taking Afobazole, a life-giving effect is felt.
Efficacy of the drug
Each human body is an individual integral system of biochemical relationships. And the effectiveness of individual medications will be different for each patient. Afobazol will help some more, Novopassit will help others. No one can accurately predict what will be better. But with all this, it is this indicator that will be most important for most patients.
That is why, unfortunately, we find it difficult to give an unambiguous answer to this question. Everyone chooses for themselves from these medicines, taking into account the above arguments in favor of both medicines. We should only add - do not take these and other medications without the supervision of a doctor. After all, it is very rare that a person will be able to identify contraindications to the prescription of a particular drug, as well as determine the optimal dose of the drug.
Experience of using Afobazole in the treatment of pathological anxiety in patients with general somatic practice
AGAMAMEDOVA I.N.
Ph.D.,
NIKITINA T.E.
Candidate of Medical Sciences,
Moscow Research Institute of Psychiatry, Ministry of Health of the Russian Federation
The effectiveness of Afobazole in a daily dose of 30 mg was studied in 35 patients (26 women and 9 men) aged 18 to 60 years (average age - 44.7 years) with pathological anxiety. By the end of the 4th week of treatment, therapeutic remission was observed in 68.6% of patients: marked improvement in 22.9% of patients, moderate improvement in 45.7% of patients. Therapy with Afobazol was practically not accompanied by side effects, no sedation was observed, which allowed patients to maintain their usual activity and contributed to high adherence to treatment.
Anxiety disorders are one of the most frequently identified psychopathological disorders in patients in general somatic practice. Clinical manifestations of pathological anxiety are varied. It can be paroxysmal in nature (panic disorder, somatoform autonomic dysfunction, agoraphobia, social phobia, specific phobia) or be almost constant (generalized anxiety disorder, adaptation disorders in the form of a mixed, anxious and depressive reaction, stress disorders). Most authors consider long-term pharmacotherapy to be the most justified strategy for the treatment of anxiety disorders [7, 9, 10].
Antidepressants (selective serotonin reuptake inhibitors, selective serotonin and norepinephrine reuptake inhibitors) and benzodiazepine tranquilizers are currently widely used for the treatment of anxiety disorders. Antidepressants are especially effective for a combination of anxiety and depressive symptoms [4, 8], but their significant drawback is the delayed therapeutic effect. One of the distinctive properties of benzodiazepines is the rapidity of development and severity of the anxiolytic effect. However, side effects (sedation, muscle weakness), as well as a high risk of abuse, addiction and dependence, limit the use of benzodiazepines to 2–4 weeks, which is certainly not enough for effective treatment of anxiety disorders [2, 3].
The search for selective anxiolytics devoid of such side effects led to the creation of the domestic drug Afobazol, which was developed by specialists from the Research Institute of Pharmacology of the Russian Academy of Medical Sciences. According to the chemical structure, the drug belongs to mercaptobenzimidazole derivatives, not being an agonist of benzodiazepine receptors. Afobazole restores the structure of the GABA-benzodiazepine receptor complex through the “neuron repair kit” system - sigma-1 receptors, which leads to normalization of the binding of GABA to the receptors. In experimental studies, it was shown that the drug exhibits an anxiolytic effect in animals with a “passive” phenotype of emotional stress response and, unlike benzodiazepines, does not cause a sedative effect in animals with active behavior under emotionally stressful conditions. According to experimental studies, Afobazole has an anxiolytic effect, which is not accompanied by sedative effects, muscle weakness and a negative effect on memory in a wide range of doses. Afobazole is a “short-lived” drug, the half-life is 0.82 ± 0.54 hours, and the retention of the drug in the body is on average 1.6 ± 0.86 hours. With long-term use, Afobazole does not accumulate in the body and is not addictive and dependencies. The results of randomized comparative clinical studies showed that Afobazol is an effective anxiolytic and is not inferior in effectiveness to diazepam and oxazepam [1, 5, 6]. At the same time, Afobazole, unlike benzodiazepines, is characterized by good tolerability and the absence of “withdrawal syndrome”. Also, studies have shown that there is no negative impact on the effectiveness and safety of therapy for concomitant somatic diseases.
The research presented in this article was carried out on the basis of branch No. 2 of the Moscow multidisciplinary medical rehabilitation clinic. The purpose of this work was to study the therapeutic effectiveness of Afobazole in the treatment of pathological anxiety in somatic patients.
Patients and research methods
The study included 35 patients aged 18 to 60 years (26 women and 9 men; mean age 44.7 years). In accordance with the ICD-10 criteria, their condition is assessed as: F06.4 - organic anxiety disorder, F43.2 - prolonged anxiety reaction caused by (adjustment disorder), F45.3 - somatoform autonomic dysfunction, F41.1 - generalized anxiety disorder. The spectrum of comorbid somatic pathology and the distribution of patients according to ICD-10 are reflected in Table. Itzach 1 and 2.
Diagnosis of anxiety syndrome began with screening questions: “During the last 4 weeks, have you felt restless, tense, or anxious most of the time? Do you often experience tension, irritability and sleep disturbances? Questions were asked by the attending physician during the initial examination of patients admitted to the hospital. Negative answers to both questions excluded the presence of pathological anxiety; with a positive answer to at least one of them, patients were sent for further examination to a psychotherapeutic office.
The study did not include patients with a complex structure of anxiety syndrome - with phobic, depersonalization, hypochondriacal disorders, as well as alcohol abusers and patients with severe sleep disorders.
The main examination methods are clinical and psychopathological using psychometric scales: Hamilton Anxiety Scale (HARS), Clinical Global Impression (CGI) and the Multilateral Personality Study (MMIL). In patients included in the study, the average HARS score was 32.5 ± 7.7 points.
Afobazole was prescribed in a daily dose of 30 mg as monotherapy to patients with an anxiety level of more than 20 points on the HARS. For night sleep disturbances, short-term (2 to 5 days) administration of doxylamine (Donormil) at a dose of 15 mg at night was allowed. For the treatment of somatic diseases, drugs that do not have psychotropic activity were used. The dynamics of the condition were recorded during 4 visits: visit 1 - initial assessment, visit 2 - assessment of the condition after 1 week, visit 3 - assessment of the condition after 2 weeks, final visit 4 - after 4 weeks of therapy before discharge from the hospital (patients were on treatment of somatic disease).
The criteria for treatment effectiveness were a decrease of 50% or more from the initial values of the average HARS score (therapeutic remission??), indicators of “significant improvement” and “moderate improvement” according to the CGI, as well as a significant decrease in indicators for 1 (somatization of anxiety) and 7 (fixation of anxiety and restrictive behavior) to the MMIL scales.
Results and its discussion
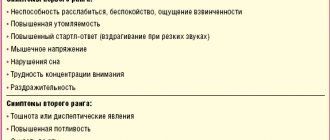
The therapeutic effect of Afobazole began to appear at the end of the first week of treatment. Patients began to “cope” with anxiety, the feeling of tension and irritability decreased. In the 2nd week of therapy, concentration and nighttime sleep improved, and vegetative manifestations lost their painful nature. At the same time, cognitive manifestations of anxiety were reduced more intensively than vegetative ones. By the end of the 4th week of the study, 24 (68.6%) patients achieved the level of therapeutic remission (a decrease in the total HARS score below 20 points and a “significant” or “moderate” improvement on the Clinical Global Impression scale). Analysis of the dynamics of HARS indicators in these patients showed that all of them underwent a significant reduction during treatment with Afobazole. The total HARS score decreased by 54.1% over 4 weeks of therapy, the mental anxiety score – by 53.5%, and the somatic anxiety score – by 55.9% (Fig. 1). Afobazole acted equally on both mental and somatic components of anxiety, while its positive effect was significantly (p < 0.05) manifested after 2 weeks and became more pronounced with further therapy with continuous improvement in indicators until the last 4 weeks. th week (p < 0.01).
When assessing the dynamics of the condition on the Clinical General Impression scale, by the time the study was completed, a pronounced improvement on the CGI scale was observed in 8 (22.9%) patients, a moderate improvement in 16 (45.7%) patients (Fig. 2). Somatovegetative indicators and interpersonal communication were normalized, which was reflected in the dynamics of the average MMIL profile (Fig. 3). By the end of the 4th week, the values on the 1st scale (somatization of anxiety, p < 0.01), 7th (fixation of anxiety and restrictive behavior, p < 0.05) and 0th (interpersonal contacts, p <0.05). In almost half (45.7%) of these patients, before discharge from the hospital, only questioning revealed elements of mental exhaustion, increased concern for health with a feeling of internal tension. Reduced ability to work and concentration remained relevant.
Therapy with Afobazole was not accompanied by side effects. The patients had no sedative symptoms, which allowed them to maintain their usual activity and contributed to high adherence to treatment.
In 11 patients (31.4%) receiving Afobazole, no positive dynamics were recorded in any of the anxiety symptoms. 6 patients (17.1%) did not note any changes in their condition, and 5 (14.3%) patients felt varying degrees of deterioration: sleep disorders became more pronounced, anxiety, headaches and irritability increased. By the end of the 4th week, patients did not note improvements in socio-psychological functioning; they experienced fears and doubts about the possibility of solving professional, everyday, family and other interpersonal problems.
Thus, our results indicate that Afobazole is an effective drug for the treatment of pathological anxiety in patients with general somatic practice, which is consistent with the data of other authors [1, 5, 6]. The drug has a fairly rapid effect: a clinically significant reduction of psychopathological disorders, along with an improvement in well-being, begins from the 2nd week of therapy. Afobazole is characterized by good tolerability, a simple regimen of administration, the absence of sedation and a positive effect equally on the mental and somatic components of anxiety.
Literature
1. Avedisova A.S., Chakhava V.O., Less Yu.E., Malygin Ya.V. New anxiolytic “Afobazol” in the treatment of generalized anxiety disorder (results of a comparative study with diazepam) // Psychiatry and psychopharmacotherapy. – M., 2006. – T. 8, No. 3, pp. 16-19. 2. Borodin V.I. Side effects of tranquilizers and their role in borderline psychiatry // Psychiatry and psychopharmacology. 2000. No. 3. P. 72–74. 3. Lawrence D.R., Benitt P.N. Side effects of drugs. Clinical pharmacology: in 2 volumes / Transl. from English M., 1993. T. 1. P. 254–94. T. 2. pp. 54–80. 4. Mosolov S.N. Clinical use of modern antidepressants. St. Petersburg, 1995. 565 p. 5. Neznamov G.G., Syunyakov S.A., Chumakov D.V., Mametova L.E. A new selective anxiolytic afobazole // Journal of Neurology and Psychiatry named after. S.S. Korsakov. –2005. – No. 4. – pp. 48–54. 6. Smulevich A.B., Andryushchenko A.V., Romanov D.V. Psychopharmacotherapy of borderline anxiety disorders (a comparative study of the anxiolytic effect of afobazole and oxazepam in patients with adaptation disorders and generalized anxiety disorder) // Russian Medical Journal. –2006. –No. 9. – P. 725–729. 7. Cottraux J. Recent developments in the research on generalized anxiety disorder. // Curr Opin Psychiatry 2004;17: 49–52. 8. Rickels K, Downing R, Schweizer E, et al. Antidepressants for the treatment of generalized anxiety disorder. A placebo-controlled comparison of imipramine, trazodone, and diazepam. // Arch Gen Psychiatry 1993;50:884–95. 9. Rouillon F. Long term therapy of generalized anxiety disorder. Eur J Psychiatry 2004;19(2):96–101. 10. Roy-Byrne PP, Katon W. Generalized anxiety disorder in primary care: the precursor/modifier pathway to increased health care utilization. // J Clin Psychiatry 1997; 58(Suppl. 3):34–38.
Novopassit
Novopassit is a complex product that contains exclusively natural (herbal) ingredients. Prescribed for disorders of the nervous system.
Novopassit helps:
- Restore mental balance;
- Relieve anxiety;
- Eliminate the problem of fears and nightmares;
- Improve mood.
Novopassit is sold without a prescription, as it has a mild sedative effect and relieves emotional stress.
Bottom line
Based on a detailed analysis of the two drugs, we can conclude that they are different in composition and therapeutic effect. The active substance Afobazole promotes the regeneration of damaged nerve cells. Novopassit triggers inhibition reactions in the brain, which leads to decreased attention.
Both drugs are well tolerated and have minimal contraindications. The advantage of Afobazole is the preservation of the therapeutic effect for 1-2 weeks after the end of the course of therapy.
It is better to choose the right drug for nervous disorders after consulting a doctor. Only a doctor will make the correct diagnosis and prescribe adequate therapy. Self-medication can worsen the patient's condition.
Comparative analysis
Having considered the main indicators and characteristics of Novopassit and Afobazol, you can conduct an analysis that will help you choose exactly the drug that will suit you best.
| Novopassit | Afobazole | |
| Composition (active components) | Valerian, lemon balm, St. John's wort, hawthorn, hops, elderberry | Morpholinoethylthioethoxybenzimidazole dihydrochloride |
| Dosage | Orally 5 (10) ml three times a day after or during meals | Orally after meals, 10 mg (daily dose – 30 mg) |
| Restrictions | Myasthenia gravis, epilepsy, bradycardia, up to 12 years | Pregnancy, lactation, individual intolerance, up to 18 years of age |
| Side effects | Allergy | Allergies, headache (rare) |
| price, rub. | 174,00-208,00 | 259,00-412,00 |