Hemorrhagic stroke (HI) is a clinical syndrome in which there is a sharp development of focal and/or cerebral neurological symptoms due to spontaneous hemorrhage into the substance of the brain or into intrathecal areas. The pathological process is triggered by factors of non-traumatic genesis. This type of hemorrhage has the highest disabling ability and is associated with the highest risk of early death.
Causes and mechanism of development of hemorrhagic stroke
The factors that cause rupture of the vascular wall and hemorrhage may be primary and secondary diseases of the cerebral arteries. Primary diseases initially develop in one or more vessels of the brain; they are not a consequence of any other diseases and often represent congenital changes. Secondary pathologies of the cerebral arteries appear against the background of other diseases, such as diabetes mellitus or systemic lupus erythematosus.
The most common primary factors may be:
- aneurysmal dilatation - an area where, due to the weakness of the vascular wall or the consequences of an injury, the artery becomes wider and adapts less well to increased blood pressure or other changes in vascular tone;
- vascular malformation is a congenital disorder of the structure of a vessel, which is manifested by the formation of “vascular glomeruli” with cavities of various sizes;
- other congenital anomalies of the arterial vessels of the brain.
Secondary causes that can lead to changes in cerebral vessels and their rupture include:
- arterial hypertension, especially difficult to treat;
- atherosclerotic damage to the vascular wall;
- vasculitis - inflammatory changes in the wall of blood vessels;
- thrombosis of intracranial veins, which lead to hemorrhage;
- diseases manifested by pathology of the coagulation system (blood and liver diseases);
- uncontrolled use of drugs that affect blood clotting (anticoagulants, antiplatelet agents, fibrinolytics);
- pronounced metabolic disorders that develop during long-term severe illnesses.
The most common cause of hemorrhagic stroke in elderly patients is arterial hypertension - this is about 80% of “vascular accidents”. The second place is occupied by atherosclerosis.
In age groups under 40 years, congenital local dilations of blood vessels (aneurysms) and malformations predominate among the causes of hemorrhagic stroke.
Due to the differences in the causes of the disease in different age groups, early and most accurate diagnosis of the pathology comes first. On our website you can find comprehensive information about methods for identifying risk factors for stroke, as well as find out in which centers they are carried out.
Etiology and pathogenesis
Hemorrhagic stroke usually develops suddenly, more often during the daytime in people whose age ranges from 35 to 60 years. In some cases, the disease can affect a person younger than the specified age if they use drugs.
The main causes of the occurrence and development of hemorrhagic stroke may be:
- hypertension stage 2 or 3;
- endocrine system disorders (thyroid disease, pituitary adenoma);
- systemic connective tissue diseases;
- blood diseases (hemophilia, thrombocytopenia);
- avitaminosis;
- intoxication;
- congenital angioma.
Against the background of these diseases, the endothelium (the walls of brain vessels) functions with disturbances that increase the permeability of brain vessels. As a result of high blood pressure, there is a greater load on the endothelium and the formation of aneurysms and microaneurysms (vasodilatation) is observed.
There are also risk factors against which a hemorrhagic stroke may develop. Among these factors:
- hypertension;
- abdominal obesity;
- dyslipidemia;
- low physical activity;
- smoking;
- long-term exhausting diets;
- diseases of the vegetative-vascular system;
- diabetes;
- alcohol abuse;
- nervous overstrain;
- stress or depression.
Types of intracranial hemorrhages
Depending on the location of the vessel from which the blood leaked, this type of stroke is divided into:
- parenchymal hemorrhage, characterized by the formation of a hematoma inside the brain or hemorrhagic impregnation of the nervous tissue;
- subarachnoid, which occurs when blood accumulates between the arachnoid and pia mater of the brain.
With parenchymal hemorrhage, depending on the caliber and location of the vessel, blood may break through into the ventricles of the brain. Such strokes are often characterized by an extremely severe course and loss of a relatively large amount of blood.
What happens during a stroke
Regardless of the cause of hemorrhagic stroke, the mechanism of damage to brain cells is the same. The pathological effect has several directions:
- Impaired tissue nutrition - due to the fact that the brain receives blood from several main vessels, this effect is partially compensated.
- Mechanical damage due to the fact that blood leaves the vessel under pressure and “pushes” the tissues apart.
In the case of parenchymal damage and hematoma formation, the second pathway is more pronounced, resulting in a disruption of communication between brain cells. Hemorrhagic permeation is a relatively uniform distribution of blood between the tissue structures of the brain, therefore the clinical course of such hemorrhage is more favorable.
In subarachnoid hemorrhage (SAH), there is a space where blood gets trapped. For this reason, mechanical damage is less than during the formation of a hematoma, but blood loss and malnutrition of brain tissue can be pronounced.
Cerebral hemorrhage (no matter how mild it may initially seem) is a condition that requires urgent diagnostic and therapeutic measures. Prescribing the correct treatment is possible only after neuroimaging, that is, magnetic resonance or computed tomography.
On our website you can get reliable information about the current discounts and promotions at various diagnostic centers for brain research this month. And also find out where it is possible to conduct an inspection at night, if necessary.
Causes
Many scientists compare the process of this stroke to an explosion in the cranial cavity. The volume of blood entering from the vessels (hemorrhage) reaches from 20 to 500 ml.
Stroke surgery
Surgery for stroke is one of the measures to save the life of the victim.
The most common reasons for this phenomenon are:
- Unbearable physical and psychological stress. This includes hard physical and mental work, frequent stressful situations, climbing to heights, and frequent plane flights.
- Genetic cause (hereditary) – abnormalities in the structure of blood vessels, disorders in the blood coagulation system.
The occurrence of a hemorrhagic stroke is characterized by impaired speech function, clouded consciousness, the person is not aware of reality, and an amnesic state.
Often, during recovery, the memory returns, and the person receives memories of how he felt just before the attack: blurred vision, dizziness, movement of surrounding objects.
Manifestations of hemorrhagic stroke
Symptoms and signs of hemorrhagic stroke are very diverse, they depend on:
- process localization;
- prevalence of the lesion;
- volume and duration of blood loss;
- the degree of swelling of brain tissue and increased intracranial pressure.
The shorter the period from the onset of the disease to the provision of qualified care to the patient, the fewer complications and the better the prognosis. In order not to waste time, you need to know the general signs of a stroke:
- sudden weakness in the arm/leg;
- numbness of half the face, arms/legs on one side;
- new facial asymmetry;
- speech disorder;
- a sharp decrease in vision in one eye or blindness;
- causeless loss of consciousness, especially in combination with previous symptoms.
If any of the symptoms occur against the background of complete well-being, it is necessary to carry out an accurate diagnosis as soon as possible in a specialized medical institution.
All available information about the nearest medical centers where urgent computer or magnetic resonance imaging of the brain can be performed can be obtained by calling 8 (812) 317-00-37.
Different types of hemorrhagic stroke may occur in different ways, but they also have common features. The disease is often characterized by:
- abrupt onset;
- rapid deterioration of the condition;
- loss of consciousness;
- development in the afternoon, at the peak of physical or emotional stress.
Taking into account the peculiarities of the course of the disease, the most important factor for a successful outcome is time. This means that you should not wait for the condition to improve; you should urgently seek qualified medical help.
It is possible to carry out a timely and accurate diagnosis of this disease by dialing a phone number. Our employees will help you quickly select a medical center that meets your needs: the nearest location, the qualifications of specialists, the quality of diagnostic equipment, the cost of the study and the availability of current promotions.
General cerebral symptoms
General cerebral symptoms include:
- Headache of great intensity, which occurs suddenly and is accompanied by dizziness. Some patients describe it as “a blow to the head.” It does not stop on its own and is not relieved by painkillers. Often SAH is accompanied only by this symptom.
- Vomiting without previous nausea, caused by cerebral edema and increased intracranial pressure.
- Loss of consciousness followed by the development of a coma. This symptom may be the only manifestation of a hemorrhagic stroke. It is important that there is a person with the patient who saw what happened.
- Stunnedness, causeless drowsiness. However, often at the initial stage of development of hemorrhagic stroke there is increased emotional and motor excitability, which is then replaced by inhibition.
- Signs of dysfunction of the autonomic nervous system: cold sweat, feeling hot, dry mouth.
- An increase in body temperature to high values can be observed in severe cases.
Focal symptoms
Focal manifestations are a group of symptoms characterized by a number of specific neurological signs that occur depending on the location of the lesion.
The most common focal manifestations are:
- weakness in the arm/leg/half of the body, up to paralysis;
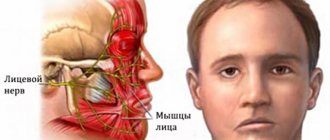
- violation of the movement of facial muscles, due to which the eyelid does not rise, the corner of the mouth drops and the cheek “sails” when exhaling;
- impaired skin sensitivity;
- pathology of speech, vision, hearing;
- exotropia;
- swallowing disorder;
- spatial disorientation of varying severity - staggering, tilting and turning to the side when walking, inability to assume a vertical body position.
Sometimes, based on characteristic focal manifestations, the localization of the pathology can be assumed:
- When the lesion is located in the frontal lobe, characteristic symptoms may be a forced rotation of the patient’s head and eyes in the direction of the hemorrhage. The so-called “frontal psyche” often develops, which manifests itself in an inadequate assessment of the state of health and a decrease in criticism of one’s actions.
- The localization of the hematoma in the temporal lobe may be indicated by early epileptic seizures.
- Hematomas of the parieto-occipital localization can sometimes have scant symptoms and are detected by chance during CT or MRI of the brain, which indicates the importance of neuroimaging methods.
- Hemorrhagic stroke in the brainstem often manifests as breathing and heartbeat disturbances.
- Damage to the cerebellum is characterized by loss of consciousness, vomiting, severe dizziness and loss of coordination.
It should be noted that these clinical manifestations can be seen with small hematomas. With its significant size, cerebral edema rapidly increases and the patient’s condition becomes so severe that it becomes impossible to determine focal symptoms.
Epileptic seizure
In some cases, the disease is preceded by an epileptic seizure, which is characterized by suddenness and spontaneity. The man screams, falls to the floor, throws his head back and convulses, wheezing. Foam may come from the mouth, sometimes even with blood (the presence of blood is explained by the fact that the patient may bite his tongue during a fall or convulsions). During convulsions, the patient’s gaze is directed towards the hemorrhage, on the same side the pupil is more dilated, sometimes there is strabismus, the eyeballs seem to float, the gaze “wanders”. On the side of the face opposite to the hemorrhage, a “sail” symptom is observed, when the corner of the mouth is relaxed and slightly lowered than the other, and the cheek does not hold air when exhaling. The upper eyelid is also drooping.
Meningeal symptoms
Signs of irritation of the meninges can occur with parenchymal hemorrhage due to cerebral edema, but they are more characteristic of subarachnoid hemorrhage.
The most typical sign is a stiff neck, when the patient is unable to press the chin to the chest when lying down.
If the patient bends his knees while checking for rigidity, this is another sign of irritation of the meninges, which is called Brudzinski's sign.
Stroke hemorrhagic right side
This type of stroke has a number of characteristic signs. The clinical picture characteristic of a right-sided stroke is formed from the following symptoms:
- Persistent motor disturbances on the side opposite to the lesion. Hemiparesis of the left upper and lower limbs is formed.
- Violation of all types of sensitivity of the skin (tactile, muscle-articular, pain, temperature and others).
- Muscle spasm with the formation of contractures or lack of muscle tone.
- Complex of meningeal symptoms: Brudzinski, Kernig, oculofacial phenomenon and
other.
Complications of hemorrhagic stroke
The most common complication of non-traumatic hemorrhage is epileptic seizures. They are divided into early, which arose in the first week after a stroke, and late, which developed 7 days after a cerebrovascular accident.
To a serious life-threatening illness, the human body responds with a systemic inflammatory response - an increase in body temperature, changes in blood tests. Such a complication may indicate a deterioration in the patient’s condition. Then the doctor assumes an increase in the source of hemorrhage or the addition of an infection.
The consequence of maintaining a recumbent position may be the development of deep vein thrombosis of the legs, which will entail the development of other, no less dangerous, diseases.
Complications also include cardiac decompensation, which can manifest itself in the development of various arrhythmias, cardiomyopathies, and congestive pneumonia.
Due to damage to brain tissue, memory and mental performance may be impaired.
Diagnosis of hemorrhagic stroke
In order for a person without medical education to be able to promptly suspect the initial signs of a stroke in a relative or friend, special recommendations have been developed.
The “Face-Hand-Speech” test involves detecting the most typical signs of pathology:
- Detection of facial asymmetry.
- The patient needs to extend both arms in front of him. If one of them involuntarily descends, then there is a possibility of a vascular accident.
- The patient is asked to give his full name, address, time of year to determine speech impairment and the person’s orientation in space and time.
There are simplified versions of the tests, for example, UZP - smile, speak and raise your hands. If there are noticeable deviations in these actions, emergency measures should be taken to transport the patient to the hospital, that is, call an ambulance.
Before providing effective treatment, the doctor must answer two questions:
- Is there a stroke?
- If yes, what type of stroke developed?
Determining the nature of brain damage is only possible using CT or MRI - without these highly accurate research methods, the diagnosis of stroke is incomplete.
There are signs that are more likely to indicate the occurrence of a hemorrhagic stroke:
- The patient was previously diagnosed with arterial hypertension. In this case, the medications did not have the desired effect or the person did not take them.
- Deterioration of the condition is associated with a peak in physical activity or emotional stress.
- A sharp and significant deterioration in health with pronounced cerebral and focal symptoms.
For subarachnoid hemorrhage, slightly different signs have been identified, including:
- Young age of patients.
- Often the primary symptom is a severe headache.
- Insignificant severity of focal symptoms.
Often an important distinguishing feature of hemorrhagic stroke from ischemic stroke is the increase in impairment of consciousness with unchanged motor and sensory pathology. This may be a sign of an enlarged hematoma.
Differential diagnosis is vital because treatment for different types of stroke can vary dramatically.
Clinical manifestations of stroke
Precursors may indicate that a person will soon develop a stroke, but such signs do not always appear. These include impaired coordination of movements, slurred speech, pain in the eyes, numbness of the limbs, headaches on the right and left sides. 50% of patients have hemorrhagic stroke
appears suddenly, without warning symptoms; in a number of patients the same symptoms develop into a transient ischemic attack, an ischemic stroke.
Thrombophlebitis may be a consequence of chemical therapy. Therefore, many people are interested in whether it is possible to carry out chemotherapy for thrombophlebitis. What is thrombophlebitis Thrombophlebitis is a pathology of blood vessels in which thrombi (blood clots) form and the lumen of the vein closes. Read more in the article: “Is it possible to carry out chemotherapy for thrombophlebitis?”
The pathology clinic is based on spontaneous hemorrhage and, as a rule, includes the feeling of a strong blow to the head or sudden severe pain. After such a blow, many lose consciousness, a number of patients fall into a coma or die (usually with a massive stroke). Those who are conscious experience the following signs of illness:
Advertising:
- throbbing headache;
- nausea;
- vomit;
- strong heartbeat;
- facial redness;
- increased sweating;
- convulsions;
- increasing drowsiness;
- inability to answer a simple question;
- speech disorder;
- decreased tone of the limbs;
- strabismus;
- paralysis and paresis;
- swallowing disorder.
Most symptoms on the left side of the body indicate the development of a right-sided stroke, and vice versa.
Instrumental diagnostics
Computed tomography is the gold standard for detecting cerebral hemorrhage. This study is distinguished by its accessibility, information content and short scanning time.
A CT scan performed in the first hours of the disease will help the doctor establish an accurate diagnosis and prescribe the correct treatment.
If the cause of the vessel damage is a malformation, then to identify it using CT, it is necessary to administer a contrast agent. Magnetic resonance scanning without any problems will allow you to localize pathologically altered vessels without paramagnetic enhancement.
MRI is more sensitive to small foci of hemorrhage and helps to more accurately determine the stage of the process. However, in order to clarify the hemorrhagic nature of the stroke, an MRI scan should be done 24 hours after the onset of the disease. Even many years after a vascular accident, an MRI of the brain will reveal pathology.
Since MRI shows the structures of the brain in more detail, this type of tomography is preferable to determine the root cause of a hemorrhagic stroke.
Each method has its own advantages and disadvantages, so before using them, it is recommended to examine a specialist - a neurologist.
Since the patient’s further well-being depends on the time of initiation of treatment, the primary diagnosis is carried out using computed tomography. Later, after starting the necessary therapy or surgical treatment, an MRI will help clarify the cause of the stroke.
Diagnosis of pathology
The main methods used to diagnose stroke are CT, MRI of the brain, and radiography
. They allow you to determine the location and type of hemorrhage, its size. The patient may also undergo emergency angiography and spinal puncture.
Differential diagnosis is made with various diseases accompanied by a similar clinical picture, based on the following characteristics:
Advertising:
| Pathology | Differences from hemorrhagic stroke |
| Ischemic stroke | Gradual increase in symptoms, absence of meningeal signs, during lumbar puncture there is no blood in the cerebrospinal fluid. |
| Hemorrhage into a brain tumor | Less vivid manifestations, extremely rare development of coma, the person is more often conscious. |
| Brain abscess | An increase in body temperature, often the disease is preceded by epileptiform seizures. |
| Epilepsy | A history of seizures, foaming at the mouth, biting the tongue. |
| Traumatic brain injury | A history of trauma. |
| Uremic coma | Slow increase in symptoms - weakness, insomnia, dyspepsia, edema, pain in the kidney area. |
| Diabetic coma | The presence of diabetes mellitus, the development of a precomatose state with thirst, abdominal pain, vomiting, and the smell of acetone in the mouth. |
Complications of right-sided stroke
If a hemorrhagic stroke occurs on the right side, the consequences, how long they live, are the first questions that interest the patient’s relatives. With the right-sided type of pathology, the following signs are noted:
- difficulty abducting the left eye;
- sagging left cheek;
- decreased pain sensitivity on the left;
- dilation of the left pupil, etc.
Often, paralysis occurs immediately after the development of the pathology, and the inability to move and bend the left leg is more often observed. The most common complications of damage to the right side in left-handers are speech deviations; in right-handers these are usually absent. Some of the most severe complications are cerebral swelling and coma, which can last up to several weeks.
Other possible complications of right-sided hemorrhagic stroke are:
Advertising:
- paralysis of the left side of the face, glossopharyngeal, optic nerve;
- feeling of body alienation;
- serious disorders of memory, hearing, perception of the world, orientation in space;
- deterioration of brain activity and behavior;
- depression, passivity;
- psychical deviations.
Complications of left-sided stroke
When did a hemorrhagic stroke on the left side develop, how long do they live, what are the consequences? Typically, damage to the left hemisphere is observed more often ( 65% of cases
). Since this part of the brain is responsible for speech and logical thinking, these functions are most affected. Speech disorders include unclearness, slurred pronunciation, misunderstanding of someone else's speech, and speaking in fragments of phrases. Also, a person cannot think or read normally, his articulation is impaired.
Paralysis of the right side of the face, right leg and arm is no less common. Characterized by synkinesis
- when raising the healthy arm, the patient involuntarily rises. Failures in acts of defecation and urination are recorded.
Often, with this type of hemorrhage, epilepsy subsequently develops and regular severe headaches appear.
Treatment of hemorrhagic stroke
After identifying signs of a stroke, relatives or friends need to provide emergency assistance to the victim, which consists of:
- positioning the person on the right side (especially when vomiting) to prevent stomach contents from entering the respiratory tract;
- raising the upper half of the body by approximately 30 degrees;
- measuring blood pressure and helping to take medication for high blood pressure (in this case, you should not give medications that need to be washed down with water, because a stroke may be accompanied by a swallowing disorder);
- organizing optimal air access, that is, loosening the collar, tie, belt and freeing from restrictive clothing.
Upon arrival of the ambulance team, any information about the disease will help in correct diagnosis. To do this, you need to tell doctors about:
- time of onset of the disease;
- the nature of the development of the pathology: the condition worsened sharply or gradually;
- the symptoms with which the disease began;
- signs of a stroke that occurred later;
- chronic diseases (especially those that could be the cause of the development of a vascular accident);
- constant use of medications;
- blood pressure numbers (if it was measured).
The medical professional should tell everything that happened to the victim.
General principles of treatment
After admission to the hospital, the neurologist assesses the severity of the condition, and then determines whether the patient needs to be operated on or whether it is better to treat him conservatively.
Many doctors agree that the most dangerous are the 3rd day after a vascular accident, and stabilization of the condition occurs on days 5-7-14, depending on the severity of the pathology.
Regardless of the type of stroke, treatment begins with:
- Bed rest.
- Elimination of any physical stress. For this purpose, laxatives and other symptomatic drugs may be prescribed, for example, antitussives for severe dry cough.
- Organization of patient care for the prevention of infectious complications and bedsores.
- Adequate nutrition depending on the level of consciousness: if the patient can swallow on his own, he eats gentle food through the mouth, if he cannot, through a tube.
- Prescription of drugs that regulate blood clotting. This is necessary to stop bleeding or prevent its recurrence.
- The use of neuroprotectors - medications that reduce the “suffering” of brain cells from oxygen starvation.
Medicines are prescribed only when they are necessary and not contraindicated.
Management of patients with subarachnoid hemorrhage
If the diagnosis of subarachnoid hemorrhage is confirmed, the patient must remain in the hospital for at least a month. Treatment consists of:
- Monitor blood pressure and lower it with medications if necessary.
- Prescriptions of drugs that relieve headaches and agitation.
- Normalization of breathing and metabolic disorders.
- Reduce intracranial pressure by administering osmotic diuretics and elevating the head of the bed for several weeks.
- Carrying out therapeutic measures to prevent complications in the form of spasm of cerebral vessels, that is, the prevention of ischemic disorders.
The danger of SAH lies in the fact that many patients consult a doctor only some time after the onset of the pathology. Therefore, treatment may be less effective.
Symptoms
When several small hemorrhages occur, when vital areas of the brain are not affected, the symptoms are often unclear. However, then such hemorrhages tend to merge into one, resulting in a large lesion that is characterized by severe headache, dizziness and nausea.
Such symptoms greatly complicate diagnosis. The patient is in no hurry to see a doctor, trying to independently remove such signs using painkillers. This type of stroke is considered mild because important areas of the brain are not damaged.
When large vessels rupture, significant damage to the left hemisphere is observed. This is expressed by the following symptoms:
- Loss of consciousness.
- Severe, growing headache .
- Nausea and vomiting.
- Feeling of throbbing in the head.
- problems .
- Pain in the eyes in the light and when they move.
- "Floaters" and circles before the eyes.
- Rare pulse.
- Pale face because blood flow is worse.
Rehabilitation after stroke
Even a mild stroke can cause serious damage to health - speech and memory are impaired, and motor functions are lost.
A number of symptoms have also been identified that can become irreversible and lead to disability of the patient:
- Speech is impaired : the patient speaks poorly, sometimes speaks only nouns (easier form), sometimes only sounds, and does not understand speech well.
- The right side of the face changes: the eyebrow, corner of the lips and eyes droop, the facial muscles are paralyzed and it seems that the right side of the face is sagging.
- paralysis or paresis appears
- The gaze is not fixed on a specific object, the pupils rotate.
In addition, the patient may often break into a sweat; with strong flushes of blood, he cannot bend his head to touch his chin. When lying down, the legs are bent because they do not extend at the knee. Symptoms increase quickly.
Why can our articles be trusted?
We make health information clear, accessible and relevant.
- All articles are checked by practicing doctors.
- We take scientific literature and the latest research as a basis.
- We publish detailed articles that answer all questions.
Sometimes stupor or coma may occur. The patient may behave inappropriately: gets irritated, constantly moves, shows aggression (can become dangerous not only for others, but also for himself).
An attack similar to epilepsy is often observed: a person falls, throws his head back, foam comes out of the mouth, and the body is seized with severe convulsions. In this case, one must not allow one to bite one’s tongue and do everything possible to prevent the person from suffocating or choking on his own blood and vomit.
If such symptoms appear, you should immediately consult a doctor, since the patient may die or remain disabled for life.
Management of patients with intracerebral hemorrhage
Hemorrhagic stroke is a condition that requires emergency diagnosis, adequate treatment and observation.
To do this you need:
- Conduct constant monitoring of the patient’s condition, especially in the first days after the onset of the disease: monitoring breathing and indicators of the state of the cardiovascular system.
- Monitor blood pressure numbers. They are often not reduced to normal levels, so as not to impair blood supply to the brain and provoke vasospasm.
- Prescription of hypoglycemic drugs - in almost half of patients, blood glucose levels increase.
- Use of antipyretic drugs. An increase in body temperature entails worsening cerebral edema, increased intracranial pressure and can lead to a significant deterioration in the patient’s general condition.
- Carrying out symptomatic therapy and treatment of complications.
Rehabilitation after hemorrhagic stroke
Recovery of post-stroke patients is an important stage in improving a person’s quality of life. Carrying out these activities helps eliminate existing movement and sensitivity disorders.
Medical rehabilitation should be:
- individual - developed for a specific patient;
- timely - start as early as possible;
- adequate - depend on the patient’s condition and his capabilities;
- staged - gradual, slow complication of exercises and an increase in the variety of rehabilitation methods;
- long-term;
- comprehensive - for greater efficiency, the maximum possible rehabilitation methods are used to influence the human body from different angles;
- successive - when a patient moves from one medical institution to another, recovery measures must continue each other.
The main criterion for starting rehabilitation measures for hemorrhagic stroke is not only normal hemodynamics (blood pressure, heart rate), but also the reverse development of changes in the brain (for example, signs of a decrease in cerebral edema).
The most important factor influencing the quality of recovery is the active participation of the patient in the rehabilitation process.
The transition to more complex exercises is made only if the condition of the patient’s cardiovascular and respiratory systems is monitored.
Forecast
In contrast to ischemic brain damage, the prognosis for hemorrhagic cerebral stroke is much more serious. In approximately 60-80% of cases, the prognosis is unfavorable for life, and the outcome of a vascular accident is the death of the patient. Fatal outcomes are especially common in hemorrhagic stroke localized in the brain stem, blood breakthrough into the ventricular system of the brain. When aggravated by decompensated somatic pathology and extensive hemorrhage, death occurs in almost one hundred percent of cases. The prognosis for work ability is also unfavorable. Although, in general, the prognosis for functional restoration is better than for ischemic stroke. With speech disorders, severe paresis of the limbs due to hemorrhagic stroke, patients become disabled in most cases. Only in small areas of hemorrhage that do not affect important speech and motor areas does the patient return to work after long-term rehabilitation. I would especially like to touch upon the issue of patients in a coma. The prognosis for a hemorrhagic stroke in a comatose patient is very difficult to predict. Coma is not at all an indicator that a person will die. Attention should be paid to the state of hemodynamics, electrolyte metabolism, renal and pulmonary functions. If blood saturation reaches 95-96%, creatinine clearance is normal, and the patient’s blood pressure and heart rate are adequate without hardware support, then the prognosis is generally satisfactory. The prognosis worsens when artificial ventilation is required, air oxygenation with humidified oxygen is required, and the acid-base balance is unstable.
Rehabilitation in the intensive care unit
12-24 hours after a vascular accident, it is already possible to carry out restoration measures. Before they begin, a test is performed to assess independent swallowing, after which the patient’s feeding method is selected.
The following rehabilitation methods are used during the acute period of a stroke:
- Treatment by position. The position of the patient's head/arms/legs should be changed approximately every two to three hours, as well as turned to the side (if the condition allows it). In order to hold a person in a certain position, bolsters or pillows are used.
- Verticalization - giving the patient an upright position. This can happen passively (with the help of a functional bed or table), passive-active and active. However, to carry out this rehabilitation method, it is necessary to ensure the stability of the circulatory system. More often, verticalization begins in the neurological department.
- Breathing exercises can be carried out in various ways depending on the patient’s condition: vibration with the hands while exhaling, in a position that facilitates breathing, contact breathing (stimulation by touching the hands to the chest) and others.
- Therapeutic gymnastics includes assistance in restoring not only the large muscles of the limbs, but also the muscles of the neck and eyes. At the initial stage, passive gymnastics is performed, when flexion/extension of the patient’s fingers, arms and legs is performed by a qualified physical therapy nurse.
Also during this period, physiotherapeutic treatment is actively used: magnetic therapy, magnetic laser therapy, reflexology, electrical stimulation, darsonvalization and other methods.
Recovery in a rehabilitation center
The most effective assistance in rehabilitation is provided in specialized medical centers. It includes the following methods:
- kinesitherapy – training in walking and everyday skills;
- electrical stimulation of peripheral nerves and muscles;
- physiotherapy and massage;
- classes with a speech therapist-aphasiologist to restore speech;
- use of neurotrophic medications (Cerebrolysin, Piracetam, Semax);
- psychotherapy;
- biofeedback sessions;
- acupuncture;
- occupational therapy.
- Stroke on the left side: consequences and features of recovery. How long do people live with this diagnosis?
If the patient ends up at home, the possibilities for rehabilitation are reduced.
Rehabilitation in the acute period
At this stage (from 24 hours to 3 weeks), maintaining the achieved effect and improving exercise tolerance plays a significant role. For this purpose, methods such as:
- treatment by position;
- massage, which is equivalent to passive gymnastics;
- breathing exercises;
- active verticalization in the absence of contraindications (if necessary, using additional support);
- mechanotherapy;
- training on cyclic simulators.
During this recovery period, active correction of speech disorders is carried out with the involvement of speech therapists.
Additional Research
MRI of the brain
- Cost: 14,000 rub.
More details
The initial diagnosis is established after examination by a neurologist, but instrumental diagnostics are always required to clarify the boundaries of the lesion. The most informative method is computed tomography, which allows a good examination of the brain matter. MRI is used for the same purpose if there is time for it.
Angiography gives excellent results, this is a study of blood vessels with contrast. It identifies malformations, dissections (dissections) and other vascular pathology. The important thing is that this study can be conducted in healthy people at risk. This is the best prevention of stroke if research is supplemented with treatment.
Lumbar puncture is used for diagnostic and therapeutic purposes.
Rehabilitation in the early recovery period
This stage begins 21 days from the onset of the disease and lasts up to six months.
Early recovery can take place in rehabilitation centers, clinics or at home. Self-execution of exercises is possible only if they are performed correctly and there is no need for constant monitoring of the patient. Therefore, all exercises at home are selected strictly individually.
The period of early rehabilitation should be a continuation of the inpatient recovery phase. Nowadays, more attention is paid to everyday skills: renewing them or teaching possible alternatives. Equally important is assistance in a person’s social adaptation.
Life after a stroke - rehabilitation and prevention of recurrent stroke
For a person who has suffered a hemorrhagic stroke, treatment and rehabilitation are vital. A range of treatments can help people cope with the different effects of a stroke, including the specific physical, mental, social and emotional problems they may face. This may include relearning skills, adapting to changes, and rethinking your life.
Today, for the sake of effective rehabilitation, it is not necessary to go to a special medical center or sanatorium; recovery can be done on an outpatient basis and at home, without compromising the quality of rehabilitation, but, on the contrary, more effectively, because a person is in a familiar and comfortable place, close to loved ones. Read more about how comprehensive rehabilitation at home works here:
Stages of rehabilitation
Recovery after a hemorrhagic stroke will depend on which functions are impaired and the severity of the impairment. Functional changes after a stroke will depend on which part of the brain was damaged and how severely.
Rehabilitation objectives:
- maximum restoration of motor and speech functions;
- physical and psychological adaptation of a person to changed living conditions.
Each patient recovers differently from a hemorrhagic stroke. This depends on the volume of brain cells affected, age, chronic diseases and other factors. Recovery after a stroke is divided into several periods:
- early stage - thanks to early rehabilitation in the hospital, it is possible to significantly improve the restoration of lost functions;
- stage after discharge - the patient continues to restore lost functions on an outpatient basis or at home.
Rehabilitation in the late recovery period
This stage lasts from six months to a year after the stroke, and sometimes longer (with persistent changes). Rehabilitation in the late recovery period involves preparing the patient for the maximum independence that he can achieve.
In addition to physical rehabilitation, work continues on social adaptation and restoration of professional skills or reorientation.
Most experts point to the positive effects of occupational therapy, especially work related to the earth.
During this period, a person may need psychological support, so psychotherapeutic consultations are carried out.