Depression is one of the most common diseases. In terms of prevalence, it is second only to cardiovascular diseases. And of all those suffering from depression, only no more than 20% seek qualified help.
In this article we will tell you about all the drugs used to treat depression.
All medications with antidepressant effects can be divided into several groups:
- Antidepressants.
- Normotimic drugs.
- Neuroleptics.
- Tranquilizers.
- Nootropics and metabolic agents.
- Herbal remedies.
- Amino acids.
- Psychostimulants.
Normotimic drugs
Medicines in this group have an antidepressant effect only in cases where the depressive state is caused by chronic affective diseases, such as bipolar affective disorder (BD, manic-depressive psychosis), cyclothymia, dysthymia, schizoaffective disorder. Most commonly used medications:
- Carbamazepine (finlepsin)
- Depakine chrono
- Lamotrigine (Lamictal)
- Lithium carbonate
Side effects of antidepressants
The side effect profile of antidepressants depends on their chemical structure, mechanism of action, duration of treatment and dosage used. Common side effects of antidepressants when used in therapeutic dosages include:
- agitation or lethargy;
- insomnia or drowsiness;
- development of manic states;
- decreased concentration;
- hallucinations.
The side effects of antidepressants can be successfully controlled by prescribing mood stabilizers, antipsychotics, benzodiazepines and other medications. To avoid the non-core effects of antidepressants, it is necessary to follow the doctor’s recommendations for taking medications, as well as consult with him in a timely manner if the first signs of side effects occur. Since changing an antidepressant during its selection takes some time (usually 1–2 weeks), even the slightest signs of deterioration in health should not be ignored.
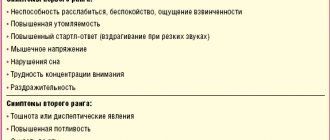
Rice. 3. Side effects of antidepressants.
Aggression and self-aggression
Antidepressants with stimulant effects can cause anxiety, irritability, aggression and insomnia. In particular, they increase the risk of auto-aggressive actions (self-harm, self-harm) and suicide. As a rule, SSRIs have such side effects, which occur in patients with suicidal tendencies.
Mania and hypomania
States of mania (up to the development of psychosis) and hypomania can occur in patients with unipolar depression, bipolar affective disorder (type I, II) and obsessive-compulsive disorder. Typically, affect inversion occurs when taking SSRIs, SSRIs, and TCAs. To relieve these side effects of antidepressants, mood stabilizers are used.
Withdrawal syndrome
Withdrawal syndrome can develop with abrupt withdrawal of TCAs, MAOIs, SSRIs taken over a period of 8 weeks. That is why it is strictly not recommended to interrupt treatment with antidepressants unilaterally, adjust the dosage yourself, or abandon them for a while.
In particular, signs of such withdrawal syndrome include:
- FLU symptoms;
- dizziness;
- headache;
- anxiety;
- nervousness;
- insomnia;
- nausea, vomiting;
- increased sweating;
- chills;
- muscle pain;
- sensory disorders;
- lethargy or hyperarousal;
- tremor of the limbs;
- gait instability.
Serotonin syndrome
Serotonin syndrome is life-threatening. It can occur when treated with several antidepressants at the same time. It is dose-dependent and requires increased attention on the part of the patient to symptoms that cause concern for the state of health. Partially, serotonin syndrome repeats the symptoms of withdrawal syndrome, but in a more pronounced version. At its peak, hallucinations, delirium, confusion, epileptic seizures, gastrointestinal and cardiovascular disorders may occur.
Decreased libido
Some antidepressants can cause a decrease in sexual activity and cause sexual dysfunction. The side effect is reversible, including by prescribing appropriate symptomatic pharmacotherapy.
Antidepressants are relatively safe drugs if taken as part of the prescribed treatment, in compliance with all recommendations of the attending physician. Taking thymoanaleptics requires the patient to take a responsible approach to treatment - monitoring themselves, making control and unscheduled visits when the first signs of side effects of antidepressants occur.
Neuroleptics
Despite the fact that most antipsychotic drugs depress the nervous system, among them there are drugs with antidepressant effects:
- Flupenthixol (fluanxol).
It has an antidepressant effect only when administered in small doses (less than 2 mg per day).
- Aripiprazole.
Effective for depression in bipolar affective disorder and schizitypal disorders.
- Levomepromazine (tizercin).
Prescribed for endogenous depression accompanied by insomnia.
Antidepressants
Of all psychiatric disorders, depression is considered the most underestimated. 10–20% of all people experience this disease at least once in their lives. Among the elderly, the prevalence of depression increases and reaches 15–25%. The main problem of depression is the insufficient development of its diagnosis and the lack of psychiatrists. Therefore, at first we considered it unnecessary to immediately burden you with the classification of antidepressants, but to pay attention to the pathogenesis of this disease. It is knowledge of the theory that helps to understand why groups of pharmaceutical drugs such as sedatives and anxiolytics are not effective enough in monotherapy.
For a long time, electroconvulsive therapy was actively used in the treatment of depression, the purpose of which was to enhance the metabolism of neurotransmitters in the brain. Surprisingly, 75% of patients actually experienced improvement in symptoms. For example, the famous pianist Vladimir Horowitz suffered from depression for years, and it was electroshock therapy that helped him return to the stage.
Vladimir Horowitz
From 15 to 30% of all depressive disorders tend to be chronic and have multiple relapses. That is why most treatment regimens are designed for a long period of time. Since some depressive disorders are associated with other diseases, it is necessary to pay special attention to the possibility of combining different groups of pharmaceuticals.
There can be several causes of depression. This condition is characterized by a number of physiological changes: the concentration of norepinephrine in the body tissues decreases, the number of serotonin receptors decreases, and their affinity for ligands decreases (5-HT 2A, 1B, 1A in the cerebral cortex - if you are not sure you can easily say, which receptor is responsible for what, we recommend re-reading our article about serotonin - https://goo.gl/iiUYKk), the activity of corticotropin and glucocorticoids increases, atrophy of the frontal and prefrontal cortex of the hippocampus is observed, there is also a decrease in the number of connections between neurons in the frontal cortex the number of blood vessels decreases, the concentration of melatonin decreases, which leads to sleep disorders . It is worth noting that depressive disorders are often inherited (40–50% of unipolar and 60–70% of bipolar disorders). However, genetic penetrance, as in the case of other mental diseases, is reduced. Therefore, 90% of patients do not have similar cases of the disease in their family. Disorders intensify depending on the duration of the disease.
In 1965, the American doctor Schildkraut suggested that depression may be based on processes leading to a decrease in the concentration of serotonin and norepinephrine in the synaptic cleft. In humans, in the posterior raphe nucleus and locus coeruleus of each cerebral hemisphere there are up to 165,000 noradrenergic and 55,000 serotonergic neurons. That is why even a slight decrease in the number of these neurons can already cause characteristic symptoms. Also, with depression, the production of presynaptically located alpha-2-adrenergic receptors increases. When norepinephrine acts on autoreceptors and serotonin acts on heteroreceptors (neurotransmitters are released from the same neuron), the entire process slows down according to the principle of negative feedback, which only increases the lack of these neurotransmitters in the synaptic cleft. Lack of adrenaline, in turn, leads to apathy and a feeling of fatigue.
Serotonin is credited with participating in the formation of contacts between neurons. Many indicators related to serotonin metabolism, such as, for example, decreased concentrations of serotonin and its receptors, mutations in genes encoding serotonin transport systems, and decreased production of serotonin-binding proteins such as p11, correlate with the severity of depressive disorder. It is assumed that a decrease in dopamine concentration also affects the development of depression, but is not its root cause.
Also, depressive disorders are characterized by a decrease in neurogenesis , mainly due to stress-induced hypercortisolism and dysfunction of the neurotrophic factor BDNF (brain derived neurotrophic factor). As a result of experiments, it was proven that increasing the synthesis of BDNF helped overcome the symptoms of depression caused by a deficiency of this factor. Scientists were able to prove that the transcription repressor GATA1 is able to reduce the number of synapses in the prefrontal cortex of animals and thus provoke the development of depressive symptoms in them. As we already wrote in our infographics (https://goo.gl/611CMc), the development of this disease is influenced by disruption of the hypothalamic-pituitary axis , as well as an increase in neuronal cholinergic transmission. Many pharmacological drugs, in turn, can cause depressive disorders (glucocorticoids, very high or low concentrations of gestagens, antipsychotics, anticonvulsants, as well as antihypertensive drugs, fluoroquinolones and interferons). Characteristic symptoms are also caused by withdrawal from opioids and benzodiazepines after long-term use.
Having analyzed these mechanisms, we can finally move on to the main thing and answer the question - what properties should drugs of this group have?
All antidepressants, except lithium and agomelatine, lead to increased concentrations of norepinephrine and/or serotonin in the synaptic cleft. This can be done in several ways: blocking the transport systems that carry these mediators back into the neuron, reducing the activity of alpha-2 adrenergic receptors (as mentioned above), reducing the activity of the enzyme responsible for the breakdown of serotonin and norepinephrine (MAO A, MAO A/B ), and also act on the serotonin 5-HT 2C receptor.
Norepinephrine enters the presynaptic terminal using a special highly selective transporter NET and partially through microglial cells using less selective transport systems. A small amount of norepinephrine can diffuse into the intercellular space, and from there directly into the blood. With depression, the concentration of norepinephrine decreases. Antidepressant drugs are able to displace norepinephrine from its connection with the receptor, which increases its concentration in the synaptic cleft and interaction with receptors. On the part of the adrenergic system, a number of changes are also observed during antidepressant therapy: the production of postsynaptic alpha-1 and beta receptors increases and the number of presynaptic alpha-2 receptors decreases. However, these changes are not typical for therapy with all types of antidepressants.
Serotonin is sent back into neurons using the SERT protein, which, as you might guess, can also be blocked to increase the amount of serotonin in the synaptic cleft. The effect of antidepressants on this system is not the same, since all receptors are very different in their structure and location. However, it can be said that under the influence of antidepressants, in general, the production of postsynaptic 5-HT2A receptors decreases, which correlates with the anxiolytic effect of these drugs, the production of presynaptic 5-HT1A receptors decreases (they have inhibitory potential according to the principle of negative feedback), and 5-HT2C is also blocked receptors, which leads to an anxiolytic effect and increased release of norepinephrine and dopamine in the prefrothal cortex.
Direct antagonists of presynaptic alpha-2-adrenergic receptors mianserin and mirtazapine block the processes of autoinhibition of norepinephrine release, which also leads to an increase in norepinephrine in the synaptic cleft. The number of presynaptic alpha-2 receptors decreases, and postsynaptic alpha-2 receptors begin to bind adrenaline more strongly.
Antidepressants, except buspirone, do not directly affect dopamine metabolism, so they do not have antipsychotic potential (except that trimipramine can block the dopamine D2 receptor). But, nevertheless, dopamine transmission increases under the influence of antidepressants. This is due to the fact that the norepinephrine transport protein NET is also able to bind to dopamine. The D2 receptor agonist pramipexole is approved for use in depressive disorders in Parkinson's disease.
It is worth noting that many mechanisms of action of antidepressants remain unexplored. For example, it is impossible to predict its strength of action based on the chemical structure of a particular antidepressant. The therapeutic effect of the drug hardly correlates with the strength of the blockade of the serotonin and norepinephrine transporter proteins. It was also not possible to note the relationship between the number of monoamine receptors and the severity of the clinical effects of antidepressants.
Side effects are mainly particularly pronounced in two groups of antidepressants - alpha-2-adrenergic receptor antagonists and tricyclic antidepressants. These two groups of drugs act not only on those receptors that were described in the previous post, but also on muscarinic, alpha-1-adrenergic and histamine receptors. It is because of their effect on these systems that many patients refuse to take medications from these groups, preferring selective serotonin and/or norepinephrine reuptake inhibitors.
Tricyclic antidepressants (eg, amitriptyline) and alpha-2 adrenergic receptor antagonists have a fairly high affinity for muscarinic acetylcholine receptors. By blocking them, these substances cause side effects similar to those of atropine: dry mouth (risk of developing caries when consuming chewing gum containing sugar), mydriasis and impaired eye accommodation (and, as a result, an increased risk of falls), increased intraocular pressure, constipation , impaired urination, confusion up to anticholinergic delirium with optical hallucinations, tachycardia (intensified by blockade of alpha-1-adrenergic receptors). In older people, taking drugs that cause xerostomia is especially problematic. They have to constantly drink water, increasingly replacing it with drinks high in sugar, which affects the metabolism of carbohydrates, leading to the development of tooth decay and weight gain. Dry mouth is a side effect of more than 500 medications, including mainly anticholinergics (tricyclic antidepressants, antipsychotics, histamine receptor antagonists type 1), as well as antihypertensive drugs (beta blockers and calcium channel inhibitors). By following the rules of oral hygiene and the recommendations of the dentist, you can successfully avoid this side effect. As you can guess, it is better not to combine drugs from these groups with other substances that cause atropine-like effects (neuroleptics, antiparkinsonian drugs, type 1 histamine receptor blockers).
Blockade of adrenergic alpha-1 receptors by tri- and tetracyclic antidepressants leads to vasodilation, which increases the risk of hypotension. Therefore, these groups of medications are not recommended to be taken at night. In case of heart failure and severe hypertension, orthostatic hypotension caused by antidepressants can be especially acute (in this case, therapy with sympathomimetics etilephrine and midodrine is recommended). There is also a risk of developing reflex tachycardia and rhythm disturbances, which can increase due to the simultaneous blockade of acetylcholine receptors and the resulting decrease in parasympathetic activity.
Tricyclic antidepressants and alpha-2 adrenergic receptor antagonists are capable of blocking type 1 histamine receptors almost as strongly as selective blockers of this group. This is due to the affinity of the domains that bind to these receptors: many substances that are antagonists of type 1 histamine receptors are also antagonists of the muscarinic acetylcholine receptor (this affinity is stronger than for the type 2 histamine receptor).
The main consequences of histamine type 1 receptor blockade are sedation and drowsiness. The sedative effect is sometimes considered not a side effect, but rather a desirable one, because patients often suffer from anxiety and insomnia, especially at the beginning of therapy. Negative effects, of course, will be disturbances in concentration and attention, which is very important if the patient needs to drive a vehicle.
Even the average person knows from the media another side effect of antidepressants - increased appetite and a tendency to gain weight. The fact is that type 1 histamine receptors are also located in the hypothalamus and are responsible for appetite. Signals from these receptors control satiety to the same extent as leptin. When they are blocked, accordingly, this signal weakens, which leads to the patient gaining weight. When blocking 5-HT2A receptors, this effect is especially pronounced. Sometimes patients gain 10 to 20 kilograms in weight, which, of course, affects self-esteem and thus the effectiveness of the therapy itself.
The purpose of taking antidepressants is to enhance the influence of norepinephrine, adrenaline and serotonin, which does not come without its side effects. Patients are prone to increased sweating, which is exacerbated by taking estrogens and the serotonergic opioid tramadol.
Norepinephrine increases the tone of the bladder sphincter, which leads to difficulty urinating. Serotonin causes nausea and diarrhea. Due to inappropriately strong release of antidiuretic hormone, hyponatremia (Parhon's syndrome) may develop when taking some antidepressants.
The use of antidepressants (in high concentrations) can lead to increased blood pressure. Also, when taking them, the development of anemia and agranulocytosis is possible. Some drugs, such as venlafaxine and mirtazapine, cause hair loss. There is a relationship between taking antidepressants and the development of restless legs syndrome.
Tri- and tetracyclic antidepressants
Drugs in this group are non-selective monoamine reuptake inhibitors. This complex name hides the very mechanism of action of these antidepressants.
This group of antidepressants is the only one that received its name due to the structure of the molecule. In 1957, the form of the tricyclic antipsychotic drug chlorpromazine was deciphered. This similarity in the structures of neuroleptics such as phenothiazine and thioxanthene explains the similarity of the effects of antidepressants and neuroleptics, such as trimipramine, which also has an antipsychotic effect.
Let us recall that drugs in this group inhibit the reuptake of norepinephrine and serotonin by neurons (with the uptake of the former predominant), inhibit the 5-HT-2A/C serotonin receptor (anxiolytic effect of clomipramine), and also block the histamine receptor type 1 (sedative effect). In small quantities, they also inhibit dopamine reuptake.
Tricyclic antidepressants have lipophilic properties, which allows them to easily cross the BBB. In their metabolism, a special role is played by the so-called first pass effect, which determines their low bioavailability. TCAs are metabolized in the liver, so if they are overdosed, forced diuresis does not bring results. Under the influence of CYP2D6, tertiary amines (amitriptyline, imipramine) are converted into secondary amines (desipramine, nortriptyline).
Depending on the type of parent compound, all TCAs are divided into three groups:
Imipramine type: imipramine and clomipramine. Amitriptyline type: amitriptyline, amitriptyline oxide, doxepin, opipramol, trimipramine. Desipramine type: desipramine, nortriptyline.
The effect of TCAs is not immediately noticeable. In the first week, the sedative component mainly predominates, in the second - the thimeric component, in the third week their thymoleptic effect is observed. This inhibition of the effects of TCAs makes it possible to assume that not all the mechanisms of action of these drugs have been studied, because the concentration of neurotransmitters in the synaptic cleft increases already on the first day of administration.
Amitriptyline is used for severe forms of depression. In low dosages (25–50 mg), amitriptyline is also used as a coanalgesic for neuropathic pain. Like many other drugs in this group, amitriptyline has a wide range of side effects (see part 2), which, however, weaken over time. Tricyclic antidepressants also inhibit adrenergic α1 receptors, muscarinic acetylcholine receptors and type 1 histamine receptors. Anticholinergic effects include dry mouth, diuresis disturbances, constipation, accommodation disturbances, visual disturbances, increased intraocular pressure, tachycardia and delirium (especially in elderly patients. TCAs are contraindicated in dementia). The development of seizures of central origin is possible. TCAs have cardiotoxic and negative inotropic effects, which lead to hypotension, an increase in the QRS complex and the development of cardiac arrhythmias. Due to the blockade of adrenergic α1 receptors, the development of orthostatic hypotension is observed. Due to the blockade of type 1 histamine receptors, patients experience dizziness, fatigue, weight gain and appetite. This is why taking TCAs is recommended before bed. TCAs also provoke the development of Parhon syndrome. Symptoms of TCA overdose are similar to those of serotonin syndrome: fever, extrasystole, tachycardia, confusion, mydriasis, hallucinations, visual impairment. It is recommended to treat this condition with physostigmine, as well as activated carbon, anticonvulsant drugs, sodium bicarbonate and infusion of isotonic solutions.
Nortriptyline is a metabolite of amitriptyline and is more suitable for combination therapy, primarily due to its weakened anticholinergic effect and cardiac side effects. However, desipramine-type drugs, which include nortriptyline, are characterized by a particularly pronounced thimeretic effect. Imipramine-type drugs are no different in this.
Imipramine is a highly potent norepinephrine transporter inhibitor. Because it only slightly inhibits type 1 antihistamine receptors, the sedative effect of imipramine is significantly reduced. Its anticholinergic side effects are much less pronounced. Trimipramine also inhibits the D2 receptor and is the only drug in this group that has an antipsychotic effect.
Clomipramine , on the contrary, differs in that it inhibits SERT quite strongly. Its associated anxiolytic effect is used in the treatment of obsessive-compulsive disorders.
Doxepin binds to H1 receptors, inhibiting them, which is used in the treatment of neurodermatitis (off label use), reducing the feeling of itching, and the sedative component helps to sleep. The drug is prescribed for alcohol withdrawal syndrome and opioid withdrawal.
Trimipramine , as noted earlier, is the only one of this group that has an antipsychotic effect, since it is an antagonist of dopamine D2 receptors.
Opipramol has the structure of a tricyclic antidepressant but is unable to inhibit either NET or SERT. Its main function is the blockade of type 1 histamine receptors, which causes a strong anxiolytic effect and promotes better sleep without causing dependence like benzodiazepines.
It is worth noting that sodium channel blockade (amitriptyline) promotes the development of heart rhythm disturbances with an increase in the QT interval (but provides an analgesic effect). Blockade of muscarinic acetylcholine receptors is fraught with the development of tachycardia and sympathomimetic effects: increased blood pressure and tremor.
An increase in norepinephrine tone contributes to the development of excited states of the central nervous system, up to a convulsive attack. Metabolism of tricyclic antidepressants in the liver entails an increase in the concentration of liver transaminases in the blood. It is logical to assume that drugs in this group are not prescribed to patients with epilepsy, cardiac arrhythmia in liver diseases, prostate hyperplasia and glaucoma.
TCAs are used mainly for endogenous depression, but at the moment, due to side effects, drugs in this group are more likely to be reserve drugs. Abrupt discontinuation of TCAs provokes the development of insomnia and flu-like symptoms, and there is a positive correlation of abrupt discontinuation of TCAs with the incidence of suicide.
Tetracyclic antidepressants are inhibitors of adrenergic α2 receptors. They are weak inhibitors of NET and SERT, and their ability to block type 1 histamine receptors is responsible for their sedative effect early in therapy. Therefore, these drugs have been used for agitated depression. Mianserin and maprotiline are derivatives of mirtazapine. S-(+)-enantiomers are able to block adrenergic α2 receptors and 5-HT2 receptors. R-(-)-enantiomers also inhibit 5-HT3 receptors. Mirtazapine does not block monoamine uptake. Due to its sedative effect in the absence of anticholinergic side effects and only minor emetic effects, mirtazapine is used in geriatrics mainly as a hypnotic that does not affect REM sleep. Mianserin can cause agranulocytosis and aplastic anemia, therefore, when using it, it is recommended to regularly do blood tests. Mirtazapine most often provokes restless leg syndrome and weight gain of up to 10 kg in just a few weeks. Like tricyclic antidepressants, tetracyclic antidepressants are contraindicated in epilepsy, renal failure and glaucoma.
Selective monoamine uptake inhibitors
Depending on which neurotransmitter is reuptaken, drugs in this group of drugs are divided into several types: SSRIs, SSRIs and SNRIs .
The side effects of these groups of drugs are significantly less than those of tricyclic antidepressants. Selective uptake inhibitors do not affect the activity of the cardiovascular system, and also do not have anticholinergic and proconvulsant effects. Severe side effects include serotonin syndrome (https://goo.gl/qWHHpM). Its symptoms are abdominal pain, fever, tachycardia with increased blood pressure, hyperreflexia and myoclonus. Possible death. The cause of the development of serotonin syndrome may be an overdose of drugs that enhance serotonergic effects, especially the combination of selective serotonin reuptake inhibitors with tramadol, triptans, moclobemide, MAO inhibitors and lithium preparations.
SSRI
Venlafaxine and duloxetine block the reuptake of both serotonin and norepinephrine, and both are substrates of CYP2D6.
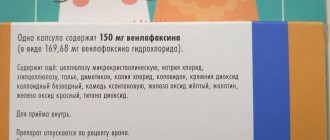
Venlafaxine (dosage 75-300 mg per day, half-life - 5 hours, active metabolite - desmethylvenflaxine) is characterized by low bioavailability (less than 20%) when taken orally. At low dosages, it is able to inhibit the reuptake of serotonin, and at high doses, norepinephrine, which, however, does not in any way affect its antidepressant potential. Venlafaxine is also capable of partially inhibiting dopamine reuptake.
Duloxetine (dosage 30–90 mg per day) blocks the reuptake of both neurotransmitters equally. As you can already guess, acting only on the reuptake of neurotransmitters, selective inhibitors of this group do not have atropinergic and sedating effects, unlike tricyclic antidepressants. Sometimes patients begin to complain of difficulty urinating, sweating and impaired potency, but this rarely leads to refusal to take medications. These drugs are contraindicated for liver disease, severe hypertension, epilepsy and glaucoma.
SSRI
Selective norepinephrine inhibitors (reboxetine, dosage 8–12 mg per day, half-life 13 hours, active metabolite desetylreboxetine) increase the concentration of norepinephrine in the synaptic cleft. Due to the numerous side effects associated with the influence of norepinephrine, SNRIs are used only for severe depressive episodes. Reboxetine is metabolized by CYP3A4, which limits its use in combination with drugs that affect the functioning of this cytochrome.
SSRIs
With selective blockade of only serotonin reuptake, the antidepressant effect of this group is better expressed. Drugs in this group include citalopram (dosage 10-60 mg per day, half-life - 33 hours, active metabolite - desmethylcitalopram), its more SERT-specific S-enantiomer escitalopram (dosage 5-20 mg per day), sertraline (dosage 50 -200 mg per day, half-life 24 hours, active metabolite - desmethyl sertraline), paroxetine (dosage 20-60 mg per day, half-life 8-30 hours), fluoxetine (dosage 10-60 mg per day, half-life 48- 96 hours, active metabolite - norfluoxetine) and fluvoxamine (dosage 50-300 mg per day). The last two drugs can also act on opioid receptors, producing an analgesic effect. Otherwise, the antidepressant effect of the above drugs is approximately the same. Also, their concentration does not change significantly in renal failure. According to many meta-analyses, escitalopram and sertraline have a better antidepressant effect, and citalopram has fewer side effects with good effectiveness. Escitalopram, depending on the dosage, can prolong the QT interval, which, unfortunately, does not allow the drug to achieve a better effect due to the need to reduce the dosage. Differences in the use of individual representatives of this group are presented in the table attached to the post. Fluoxetine and paroxetine are strong and citalopram and escitalopram are weak inhibitors of CYP2D6. Blocking this system increases the concentration of tricyclic antidepressants and antipsychotics in the blood, and the effect of tamoxifen (an estrogen antagonist, used in the treatment of breast cancer), on the contrary, decreases, since tamoxifen, being a prodrug, is activated in this system in the liver.
Blocking SERT itself causes a number of side effects, such as drowsiness and akathisia (internal restlessness due to serotonin 5HT2 receptors), especially at the beginning of therapy. Serotonin is also involved in platelet aggregation processes. The platelet membrane contains exactly the same serotonin transporter SERT as in neurons, therefore, due to a lack of serotonin, its vasoconstrictor effect on 5-HT-2A serotonin receptors is reduced. Therefore, drugs in this group should be used with caution if the patient has chronic inflammatory bowel diseases or is taking salicylic acid drugs (antiplatelet agents) or vitamin K antagonists (indirect anticoagulants). Due to increased stimulation of serotonin 5HT-2A receptors in the very posterior field (area postrema) and 5HT-3 receptors in the gastrointestinal tract, these drugs provoke vomiting, which can be stopped with 5-HT3 serotonin receptor blockers (ondansetron). It is precisely because of the feeling of nausea that drugs in this group at the beginning of therapy lead to a decrease in the patient’s weight. Due to increased secretion of antidiuretic hormone, fluid retention occurs in the body, which leads to a decrease in sodium concentration in the blood in the first 4-6 weeks after starting medication in 10-20% of patients. Impaired potency is also observed when taking this group of antidepressants.
Sertraline reversibly reduces sperm quality and causes ejaculation disorders. The reason for this is the indirect antagonism of dopamine receptors, which provokes hyperprolactinemia.
Dapoxetine is approved for use in the treatment of premature ejaculation. In this case, the drug received approval due to its side effects. However, in some cases, antidepressants of this group provoke reverse ejaculation (retrograde ejaculation of seminal fluid occurs proximally into the bladder, which can lead to inflammatory processes). Activation of serotonin receptors also affects the dopamine system: patients feel more tired (activation of 5-HT2C receptors reduces the release of dopamine). Excess serotonin provokes tremors, headaches and osteoporosis, as well as pseudocholinergic dry mouth and particularly severe sweating of the scalp. An interesting fact is the following: at one time it was observed that an increase in determination and thirst for action with drugs of this group increased the number of suicides. It was assumed that increased readiness to act led to the fact that patients with depression were more likely to decide to commit suicide. But later, one large British study refuted this statement, proving that self-abstinence from drugs increases the number of suicides.
Separately, it is worth noting the drug bupropion (dosage 150-300 mg per day, half-life 20-37 hours, active metabolites - hydroxybuproprion, threohydrobuproprion, erythrohydrobuproprion), which is mainly an inhibitor of the reuptake of norepinephrine and dopamine, but also affects other transmitter systems . It is worth noting that its use does not lead to weight gain and only slightly affects sexual functions. This drug is also approved for use in the treatment of nicotine addiction.
Sources
- Herdegen T. et al. Kurzlehrbuch Pharmakologie und Toxikologie. – Georg Thieme Verlag, 2013.
- Diener HC Klinische Pharmakologie. – Georg Thieme Verlag, 2011.
Tranquilizers
- Bromodihydrochlorophenylbenzodiazepine (phenazepam).
The drug of choice for neurotic conditions with depression and post-stress conditions. That is, in cases where short-term treatment is required.
- Clonazepam.
Strong anti-anxiety and sedative effect. When taken for a long time it causes dependence.
- Alprazolam.
Prescribed for anxiety and depression. Recommended for short courses (no more than 10 days) due to the risk of developing addiction and dependence.
Generations of antidepressants
Antidepressants are divided into five generations. Depending on the generation, their biochemical mechanism of therapeutic action differs, as well as the degree of reduction of non-core effects. However, there is no generally accepted classification of generations of antidepressants.
- TCAs, MAOIs;
- 1st SSRI, OIMAO, ChCA;
- SSRIs, SSRIs, MAOIs;
- SNRI;
- IMR.
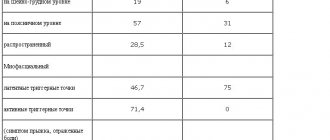
Rice. 1. Generations of antidepressants.
First generation of antidepressants
The first generation of antidepressants includes tricyclic antidepressants (Amitriptyline, Melipramine, Anafranil) and monoamine oxidase inhibitors (Nialamide, Phenelzine), synthesized between 1950 and 1960.
Second generation antidepressants
The second generation of antidepressants includes the first selective serotonin reuptake inhibitor (Fluoxetine), a reversible monoamine oxidase inhibitor (Pirlindole) and a quaternary monoamine reuptake inhibitor (Maprotiline), synthesized between 1970 and 1980.
Third generation antidepressants
The third generation of antidepressants, synthesized from 1980 to 1990, includes drugs that are widely used today - selective serotonin reuptake inhibitors (Fluvoxamine, Sertraline, Paroxetine, Citalopram, Escitalopram), selective serotonin reuptake stimulants (Tianeptine), reversible monoamine oxidase inhibitor (Maclobemide) .
Fourth generation of antidepressants
The fourth generation of antidepressants was synthesized between 1990 and 2000. It includes selective serotonin and norepinephrine reuptake inhibitors (Venlafaxine, Milnacipran, Duloxetine). Following the SSRIs, SNRIs have become widely used in clinical psychiatry.
Fifth generation of antidepressants
The latest generation of antidepressants include melatonin receptor inhibitors (Valdoxan). They have an improved therapeutic profile and do not have a negative effect on the cardiovascular, endocrine and reproductive systems; have no potential for abuse.
Nootropics and Metabolic Aids
The remedies in this group help to get out of a depressive state that has developed against the background of stress, overwork, encephalopathy, the consequences of injuries and poisoning. By improving the blood supply to neurons and energy metabolism within cells, they contribute to the activation of cognitive functions and memory. The most effective drugs in this group:
- Phenibut
- Mexidol
- Aminalon (GABA)
- Piracetam (nootropil)
- Picamilon
- Pyriditol (encephabol)
- B vitamins.
List of antidepressant drugs
The list of antidepressant drugs based on the classification of mechanism of action reflects the current trend in the clinical use of thymoanaleptics. It is not possible to provide a complete list of antidepressant drugs due to the fact that some of them are allowed for circulation within specific countries, and new names appear.
Monoamine oxidase inhibitors
Non-selective MAO inhibitors include GING derivatives (isonicotinic acid hydrazide) and amphetamine derivatives:
- nialamide;
- isocarboxazid;
- iproniazid (iprasid);
- tranylcypromine;
- pargyline.
Selective inhibitors
A list of antidepressant drugs that block either MAO-A or MAO-B includes:
- moclobemide;
- pyrazidol;
- inkazan;
- befol;
- selegiline.
Non-selective monoamine reuptake blockers
This group of antidepressants is represented by tricyclics (TCAs), including atypical, tertiary and secondary amines, heterocyclic (tetracyclic) drugs:
- desipramine;
- amitriptyline;
- imipramine;
- nortriptyline.
- clomipramine (anafranil);
- trimipramine (Gerfonal);
- doxepin;
- dotiepin (dosulepin);
- alprazolam (Xanax);
- amantadine (midatan);
- carbamazepine (finlepsin);
- thioridazine (Sonapax);
- levomepromazine (tisercin);
- alimemazine (teralen);
- chlorprothixene;
- flupentixol (fluanxol);
- clozapine (azaleptin, leponex);
- tianeptine (Coaxil);
- amineptine (survector);
- maprotiline (ludiomil);
- pirlindol (pyrazidol);
- metralindole;
- mirtazapine (Remeron);
- mianserin (lerivone).
Selective neuronal reuptake inhibitors
The list of SSRI antidepressant drugs includes:
- fluoxetine (Prozac, Portal, Prodep, Fontex, Seromex, Seronil, Sarafem);
- paroxetine (Paxil, Actaparoxetine, Rexetine, Paxetine, Seroxat, Aropax, Arquetis);
- citalopram (Celexa, cipramil, emokal, opra, sepram, cytagexal);
- escitalopram (Lexapro, Cipralex, Selectra, Ezopram);
- sertraline (Zoloft, Deprefolt, Lustral, Stimuloton, Sirlift, Asentra);
- fluvoxamine (fevarin, Luvox, favoxil, faverine, deprivox);
- vilazodone (viibrid);
- dapoxetine (Priligy).
Selective serotonin and norepinephrine reuptake inhibitors
The list of SSRI antidepressant drugs includes the following “double-action” thymoanaleptics:
- venlafaxine (Velaxin, Velafax, Venlaxor, Efevelon);
- duloxetine (Cymbalta);
- milnacipran (Ixel);
- levomilnacipran.
Selective norepinephrine reuptake inhibitors
Selective norepinephrine reuptake inhibitors (SNRIs) are represented by the following list of antidepressant drugs:
- reboxetine (edronax);
- atomoxetine (Strattera).
Selective norepinephrine and dopamine reuptake inhibitors
Today, the group of selective norepinephrine and dopamine reuptake inhibitors (SNRIs) includes the only antidepressant drug - bupropion (Wellbutrin, Zyban).
Noradrenergic and specific serotonergic antidepressants
The list of noradrenergic and specific serotonergic antidepressants (NaSSA), belonging to the group of monoamine receptor agonists, includes:
- mianserin (lerivon, bonserin);
- Mirtazapine (Remeron, Mirtazonal).
Specific serotonergic antidepressants
Specific serotonergic antidepressants (SSA) are represented by several drugs:
- trazodone (trittico);
- nefazodone (serzone).
Melatonergic antidepressant
Agomelatine (Valdoxan) is one of the newest antidepressants, differing in its mechanism of action from its predecessors.
Serotonin precursors
The list of serotonin precursors used both as monotherapy and in combination with other antidepressants includes:
- L-tryptophan;
- 5-hydroxytryptophan.
Are there non-drug treatments for depression?
In addition to medications, there are many non-drug treatments for depression. These are psychotherapy, biofeedback therapy, diet therapy, physical therapy, exercise therapy, reflexology, light and color therapy, sleep deprivation, etc. Most often, a combination of several methods is used to treat depression. For example: psychotherapy + drug treatment, biofeedback therapy + psychotherapy, medication + diet therapy, etc.
You cannot prescribe or use medications on your own. If you or your loved one is faced with the problem of depression, you need to see a psychiatrist or psychotherapist! Only according to his recommendations can you use drugs. Self-medication is life-threatening!