Hospitalization and treatment under the compulsory medical insurance quota. More details after viewing the pictures.
Brain tumors can be benign or malignant; the latter are aggressive in nature and pose a significant threat to life. Neoplasms form inside the skull due to abnormal disturbances in the cellular genetic apparatus, which leads to uncontrolled growth of tissue structures. Atypical cells are formed from normal ones as a result of mutations, exposure to physical, chemical or other factors. These can be various cells of brain tissue, for example, neurons, glial cells and others. Often, metastasizing cells formed from cancer of other organs enter the brain, which leads to the formation of secondary malignant tumors. The main treatment involves surgical removal of pathological foci, additionally radiation and chemotherapy are prescribed, as well as drugs to relieve negative clinical manifestations.
What is a craniotomy?
Sometimes accessing a brain tumor is more difficult than removing it. Therefore, some additional steps must be added to help the surgeon access the cancer in the brain. One such method is craniotomy surgery, which involves the removal of bone in addition to the levels of other brain surgeries.
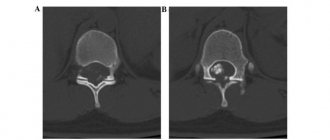
In a craniotomy, a neurosurgeon removes part of the skull bone to gain access to the tumor. Skull resection may require computer assistance and imaging to find and reach the exact location of the cancer. Naturally, magnetic resonance imaging (MRI) or computed tomography (CT) are the methods that come first.
The removed portion of the skull bone is called a “bone flap,” which is placed in place after craniotomy excision of the tumor. Typically, the bone flap is replaced at the end of the procedure with tiny plates and screws. There are cases where the bone flap does not come back, but this is another brain surgery called a "craniectomy", which will be discussed further in the FIT article.
The name of the craniotomy operation comes from the cranium (skull) to be removed. The size and complexity of the craniotomy depends on the patient's problem, which can range from brain swelling to removing foreign objects such as bullets.
What you need to know about brain cancer
Brain cancer still remains an incompletely understood and extremely dangerous disease. Based on the mechanism of formation, tumors are divided into primary and secondary. Primary ones are formed from brain cells or tissues around it. Such a tumor, if it has not yet spread further and is concentrated in only one place, has a good prognosis and the possibility of surgical removal. A secondary (metastatic) tumor grows into brain tissue from other organs and systems, so it is much more difficult to treat. In addition, you need to take into account that the brain is responsible for the proper functioning of the entire body, which means that problems in it can lead to disruptions in other functions.
Reasons for performing a craniotomy
Why does a person need to have a craniotomy and cranial resection? As briefly mentioned above, reasons for craniotomy surgery vary and include, but are not limited to:
- Access to the treatment site for diagnosis or removal of tumors
- Reducing intracranial pressure by eliminating damaged or swollen areas of the brain may be caused by traumatic injuries or strokes
- Implantation of a device for purposes such as treating movement disorders such as Parkinson's disease or dystonia (a type of movement disorder), or refractive epilepsy
- Aneurysm clipping or repair
- Removing blood or blood clots from leaky blood vessels
- Draining a brain abscess (an abscess is an infected pocket of pus in the tissue)
- Repair of skull fractures
- Repairing a tear in the membrane lining the brain (dura mater)
- Removing a foreign object, such as a bullet.
Craniotomy and resection are not only used for tumors, as explained above. Whenever the brain is under too much pressure, such as when it is swollen, has blood clots, or has an abscess, craniotomy surgery is the choice. If a craniotomy to remove a tumor, blood clots, a bullet in the head, or for any other reason is a treatment, how should the patient prepare?
Modern surgical treatment for hemorrhagic stroke
Only in specialized centers is it possible to conduct a thorough diagnosis and adequate surgical or therapeutic treatment of hemorrhagic acute stroke. However, most often a free ambulance will take the victim to the nearest city hospital, where first aid will be provided, limited by the capabilities of the institution. And surgical treatment of stroke, unfortunately, can not be performed in all hospitals.
Therefore, relatives of patients are increasingly turning to specialized advisory services that can provide:
- safe transportation;
- rapid hospitalization;
- expert monitoring of victims in intensive care units and departments of medical institutions.
Only in highly qualified centers will they conduct the necessary research, assess all the risks, and then choose the necessary treatment tactics.
Another important point that affects the patient’s further capacity is rehabilitation and care after surgical treatment of hemorrhagic stroke. The success of postoperative therapy largely depends on the experience of specialists and the availability of modern equipment.
Preparation for craniotomy
Before craniectomy surgery, the patient should stop taking any non-steroidal anti-inflammatory drugs and blood thinners for at least a week beforehand. However, if there are medications explicitly prescribed for surgery, they must be carefully taken as scheduled. In addition, the patient should not eat or drink the night before surgery.
Smoking and drinking alcohol are also prohibited from one week to two weeks after surgery. If an MRI or CT scan is required, fiducials may be placed on the patient's forehead and behind the ears to help align the preoperative MRI with the image guidance system. In many cases, the doctor must perform blood tests to make sure the patient is healthy.
Skull resection is performed under general anesthesia, regardless of the type of operation. Signing the consent form is mandatory and the patient must read the pathway carefully and know what they are experiencing. They should also know the risks associated with such brain surgeries.
Brain surgery for epilepsy
Approximately 30% of patients with epilepsy continue to suffer from seizures despite taking medications due to so-called. pharmacoresistance. In these cases, the appropriateness of neurosurgery should be considered.
Surgery removes the part of the brain where seizures occur without affecting surrounding areas. The success of the therapeutic method depends on the surgical site. After a procedure in the temporal region, up to 70% of patients get rid of seizures; with surgery in other areas, the success rate is lower.
There are patients whose illness is serious and whose attacks are severe, often associated with falls and injuries. However, sometimes it is not possible to perform surgery to eliminate them. In other cases, a surgical technique can be used to interrupt the pathways that carry seizures from one hemisphere of the brain to the other, which can change the course of the seizures.
In particularly severe cases of epilepsy, where there is no hope of controlling the disease with antiepileptic drugs or surgery, vagus nerve stimulation can be used. This is the 10th cephalic nerve, affecting the functioning of several organs of the abdominal and thoracic cavities, transmitting sensations from the intestines to the brain. Vagus nerve stimulation is performed using a device similar to a pacemaker. It is placed under the skin under the left collarbone.
Vagus nerve stimulation is only effective for some patients whose disease cannot be treated. The method helps reduce the number of attacks or shorten their duration.
Unique stereotactic surgery
A unique treatment option for epilepsy is the treatment of medial temporal epilepsy (seizures spreading from the internal structures of the temporal lobe) using a stereotactic method. The most common cause of this type of epilepsy is hippocampal sclerosis. The disease occurs as a result of brain damage in childhood, for example, during long periods of fever, meningitis.
Stereotactic surgery is intended for patients with clearly defined, localized epileptic seizures, where removal of the lesion means treatment of the disease. This is an intervention using a special electrode, through which the surgeon performs targeted thermal destruction of the tissue that is the cause of epilepsy. The results of this method are comparable to those of open neurosurgery, but with minimal burden to the patient.
Risks of craniotomy
After tumor removal or craniotomy for other reasons, the patient may experience swelling and bruising of the face or around the eyes, headache, dizziness, and problems with memory, speech, or vision. Thus, the neurosurgeon determines how many days the patient should spend in the intensive care unit (ICU), where heart rate, blood pressure, and nerve signs are constantly monitored. Despite all these precautions, the patient may still be exposed to postoperative risks.
Common post-operative risks are also present here: bleeding, infection, blood clots and reactions to anesthesia. In the case of craniotomy surgery, some other dangers are also added, depending on the type of procedure:
- Strikes
- Convulsions
- Brain swelling
- Nerve damage
- CSF or cerebrospinal fluid leak, which is the fluid that surrounds and protects the brain
- Loss of some mental functions
- Pneumonia, which is a type of lung infection
- Unstable blood pressure
- Muscle weakness
Additionally, some risks are technique-specific and do not occur in all craniotomy patients. These depend on the severity and complexity of the problem and include:
- Memory problem
- Difficulty with speech
- Paralysis
- Impaired balance or coordination
- Coma
Post-operative care can prevent or reduce some risks, but usually the patient must make a compromise and undergo surgery knowing that this may happen. In many cases, it is a matter of life or death, and the patient has no other choice.
Clinical manifestations
Symptoms are usually divided into general and focal. In the latter case, the symptoms depend on where the tumor forms.
General symptoms
The clinical picture is caused by an increase in pressure inside the skull and the toxic effect of metabolites of pathogenic cells on healthy tissue. Common signs include:
- headache not relieved by conventional analgesics;
- various visual impairments, for example, fog, doubling, glare, decreased visual acuity and others;
- loss of appetite, poor health, nausea and vomiting that are not caused by food poisoning;
- changes in the usual emotional state: mood swings, depression or aggressiveness, and others;
- symptoms of an epileptic nature;
- weakening of the brain: it is difficult for a person to concentrate, mental activity is disrupted, there is a loss of concentration, memory problems, etc.
Important. Early signs of cancer are often misunderstood by sick people. They seek help when clinical signs significantly impair quality of life. In this case, the brain tumor is diagnosed late, which significantly complicates treatment and worsens the prognosis.
Focal symptoms
Signs of this type arise due to changes in the functioning of cerebral structures, so the clinic depends on the location of the neoplasm:
- when the hemispheres are damaged, tactile sensitivity decreases, muscles in the opposite part of the body weaken (in the presence of pathogenesis in the right hemisphere, problems arise on the left side);
- disease in the temporal lobe leads to a deterioration in the ability to speak, memory suffers, and the perception of smells changes;
- pathological changes in the cerebellum lead to disturbances in gait and coordination of movements;
- damage to the frontal lobe causes mental and cognitive changes;
- neoplasia in the parietal lobe changes tactile sensations and fine motor skills;
- damage to the occipital zone negatively affects vision, and hallucinations are possible.
Important. The presence of these signs (of any type and intensity) is a good reason to seek medical advice. Early detection of pathologies improves the prognosis of treatment.
Different types of craniotomy
Like any other type of brain surgery, craniotomy also has different types, ranging from right frontal craniotomy for tumor resection to translabyrinthine craniotomy. The model is selected based on the patient's condition, the purpose of the operation and overall benefits. Some of the main types of craniotomy are as follows:
Extended Bifrontal Craniotomy When minimally invasive approaches do not meet surgical needs, the surgeon may choose an extended bifrontal craniotomy. Here an incision is made on the scalp behind the hairline and the bone that forms the outline of the orbits, and the forehead is removed.
The most common goal is to reach complex tumors in the front of the brain. This is a traditional approach to the base of the skull with the core belief that removing excess bone is safer than unnecessary manipulation of the mind. Typically, meningiomas, esthesioneuroblastomas, and malignant tumors of the skull base are treated with extended bifrontal craniotomy. Eventually the bone flap is replaced.
Minimally Invasive Supraorbital» Brow» Craniotomy
A supraorbital craniotomy, commonly known as a brow craniotomy, is another procedure for removing brain tumors. As the name suggests, this is a minimally invasive approach and involves making a small incision in the eyebrow to access tumors at the front of the brain. Rathke's cleft cysts, skull base tumors, and some pituitary tumors can also be treated with this method.
Because it is a minimally invasive procedure, it may be less painful than an open craniotomy. The recovery period may be shorter and there will not be a large scar at the surgical site.
Retrosigmoid" Keyhole" Craniotomy
A retrosigmoid craniotomy, often known as a “keyhole” craniotomy, is another minimally invasive surgical procedure for removing brain tumors. After a small incision behind the ear provides access to the cerebellum and brain stem, the surgeon can remove the tumor from the base of the skull. Meningiomas, acoustic neuromas, and metastatic tumors of the brain or spine are other targets for keyhole craniotomy.
Like other minimally invasive approaches, retrosigmoid craniotomy also requires less recovery time, while it leaves a minimal surgical scar and less pain compared to various types of brain surgeries.
Orbitozygomatic Craniotomy
Orbitozygomatic craniotomy is the second traditional approach to the skull base presented in our article. Like extended bifrontal craniotomy, orbitozygomatic craniotomy is also used to access and operate on complex tumors and aneurysms. This approach is based on the same belief as extended bifrontal craniotomy: removing excess bone is safer than unnecessary manipulation of the brain.
When minimally invasive approaches fail, the bone that forms the outline of the orbit and cheek is removed for replacement at the end for the purpose of craniotomy excision of the tumor. Some cases that can be treated with this type of surgery include craniopharyngiomas, pituitary tumors, and meningiomas. The neurosurgeon can reach deeper and access hard-to-reach areas of the brain, minimizing serious brain damage .
translabyrinthine craniotomy
In a translabyrinthine craniotomy, an incision is made in the scalp behind the ear to remove the mastoid bone and part of the inner ear bone. The significant portion of the inner ear bone that is removed here are the semicircular canals containing receptors for balance. Sometimes the entire tumor cannot be removed due to the severe damage that the removal procedure can create. However, neurosurgeons usually try to remove all or as much of the tumor as possible.
The biggest problem with this method is hearing loss. When the semicircular canals are removed, hearing is sacrificed for access and tumor removal. However, the risk of facial nerve damage may be reduced.
In all of these methods, the removed bone flap is replaced and held in place with screws and plates. This does not always happen with a bone graft, and sometimes the surgeon does not replace the bone.
Brain Operations
The risk of neurosurgical therapy does not depend on the type of organ, but on the severity, type and stage of the disease. Even today, death can result from, for example, advanced inflammation of the appendix. On the other hand, a well-prepared complex operation on the brain in its deep structures, where a “millimeter error” popular among unknowing people can lead to lifelong consequences, usually goes quite well.
Brain injuries
This is a serious socioeconomic problem, and the increase in traumatic brain injuries requires improvements in both diagnostic and therapeutic procedures. This is a group of diseases that includes both fatal injuries and damage to the nervous system requiring immediate surgical intervention. Most often, brain injuries are caused by a high-energy mechanism (road accidents, falls, dangerous sports, etc.). To prevent head injuries, we recommend using protective equipment (helmets, seat belts, child seats).
Types of TBI and related types of brain surgery:
- Concussion. The mildest type of TBI, characterized by a short-term disorder of consciousness and the inability to remember events during the injury. Vomiting is often associated with difficulty concentrating. The condition does not require surgery.
- Skull fracture. Fracture is divided into 2 types: simple fracture, which usually does not cause serious problems;
- a depressed fracture requiring surgery to straighten the cranial bone.
Brain tumors
Brain tumors (Latin: tumor), tumors, arise from a population of cells that have lost control over their division and growth. Tumors are divided into:
- benign – meningiomas, low-grade glial tumors, cysts, etc.;
- malignant – anaplastic astrocytoma, glioblastoma.
Treatment of brain tumors is complex, requiring cooperation between a neurosurgeon, oncologist, histologist, neurologist, and rehabilitation specialist.
The first step is to remove part of the skull bone. It is necessary to remove all or part of the tumor. Today, modern methods are used for these purposes (magnetic resonance, neuronavigation, modern surgical microscopy), and argon coagulation is used to stop bleeding. For some deep-rooted tumors, a biopsy is performed (taking a sample of tumor tissue for histological examination, which is important for determining the correct cancer treatment). Malignant tumors after the work of a surgeon require treatment by an oncologist. Subsequent chemotherapy reduces the risk of developing new tumors.
The purpose of the surgery is to reduce or remove the tumor that is causing pressure on the brain. On the morning of the operation, the head is shaved (partial shaving can be done). During the procedure, part of the bone is exposed; the hole serves as a path to penetrate the area where the tumor is located. After its removal, the surgical wound is restored. The procedure lasts about 4 hours.
There is a risk of cerebral edema, bleeding (about 3%), rarely - inflammation. These complications may be related to limb movement disorders or general complications (eg, pneumonia, bleeding disorders). After the intervention, the patient is treated in the intensive care unit. After discharge from the hospital, the patient undergoes outpatient and home treatment.
An alternative to surgical treatment is, in exceptional cases, irradiation of the tumor.
Metastases
Metastases, as a secondary type of tumor, are the most common intracranial tumor. They occur in 20-40% of adult patients with malignant diseases; in sectional material their share is up to 50%. About 20% of cancer patients die due to metastases. Mostly breast cancer, lung cancer, melanoma, and Gravitz tumor metastasize to the brain.
Treatment of patients with metastases is complex and multidisciplinary. Neurosurgical operations on the head are an important part of it. Correct technical execution is essential for the success of surgical therapy. An important role is played by the patient’s clinical condition, prognosis of the underlying disease, type of primary tumor, and radiological data.
Surgical resection is recommended for patients with solitary brain metastases in an accessible location, especially those with a larger tumor causing significant pressure on the surrounding area or with controlled extracranial disease.
The therapeutic procedure for patients with multiple metastases is individual, and treatment is usually controversial. Surgical therapy is considered in patients with radiosensitive primary tumors. The advantage of resection is cytoreduction or even complete removal of the tumor, reduction of ICP, obtaining material for histological and molecular diagnostics, and the possibility of additional targeted treatment.
Resection of brain metastases is performed using an operating microscope with proper MRI-based preoperative procedural planning. In these cases, standard procedures are supplemented with functional magnetic resonance or diffusion tensors. Intraoperative electrophysiology is also used to monitor important structures, or preoperative imaging, such as ultrasound.
Hydrocephalus
The brain chambers are usually filled with cerebrospinal fluid. Cerebrospinal fluid (CSF) circulates in the brain chambers and spinal canal and is constantly renewed. Under certain conditions, a barrier to fluid flow may occur, and its production itself may be increased. This leads to an increase in the volume of the brain chambers, the appearance of symptoms of high intracranial pressure (headache, vomiting, confusion).
Brain surgery is aimed at eliminating the cause of the block. One option is artificial drainage (insertion of a drainage tube into the brain chambers with an outlet in the abdominal cavity).
The type of drainage depends on the cause and magnitude of hydrocephalus (obstruction in the natural flow of fluid, impaired intracranial absorption). In children, most often (in 98% of cases) fluid is removed from the intracranial area into the abdominal cavity using various types of ventriculoperitoneal drainage. For obstructive types of hydrocephalus, minimally invasive endoscopic surgery can be used.
The operation is performed under general anesthesia and takes about 1 hour. Complications may be biological or technical in nature.
- The most serious biological complications are infections (3-20%), which according to severity are divided into several types - from local to general septic conditions. Other complications include epilepsy, subdural hematoma (4-20% in adults, 3-6% in children).
- Technical complications of drainage are represented by obstruction, disconnection of the connector, kink or rupture of catheters, etc.
The success of therapy depends on the correct diagnosis and indications (especially for normal pressure hydrocephalus in adults).
For active types of hydrocephalus, conservative treatment is ineffective; drainage operations are the only possible and often life-saving solution.
Surgical treatment does not have an equally effective alternative.
Transnasal surgery for pituitary adenoma
The transnasal approach used in most pituitary adenoma operations is aimed at eliminating or at least shortening the process in the area of the sella turcica. Intervention into the brain is carried out from the right nostril. After the procedure, a tampon is inserted into the patient’s nose for 48 hours (you have to breathe through your mouth). Sometimes a spinal puncture is necessary. After treatment, the patient usually spends 1 day in the intensive care unit.
Transnasal surgery is considered a relatively safe intervention, the most acceptable for a person in terms of time and cosmetics. Possible complications, which occur in a minimal percentage (up to 5%) of cases, include inflammation of the nasal cavity, postoperative bleeding or leakage of cerebrospinal fluid from the nose. In addition, hormonal dysfunction of the pituitary gland may occur. Less commonly, the eyes are damaged (visual impairment).
An alternative to surgical treatment is, in exceptional cases, irradiation of the pituitary adenoma.
Plastic surgery of damaged meninges
The goal of the intervention is to prevent the risk of post-traumatic inflammation of the meninges in the future. During the procedure, part of the bone tissue of the skull is removed to allow penetration into the affected area. The operation lasts approximately 4 hours.
Risks include swelling, bleeding, inflammation, and olfactory disturbance. Surgical treatment has no alternative, equally effective, replacement.
Surgery for aneurysm, malformation and other vascular problems
The procedure for vascular brain surgery depends on the type of problem.
Vessel bulge (aneurysm)
The wall of a cerebral vessel can weaken under the influence of external or internal factors. The site of weakening is susceptible to the formation of bulges (aneurysms). The risk of an aneurysm is that it may burst, causing intracranial bleeding (hemorrhagic stroke). This creates a condition that poses a direct threat to human life. It is necessary to quickly determine the location and size of the bulge and choose the optimal treatment.
The principle of therapy is to eliminate the bulge from the blood circulation, i.e. in preventing further bleeding from it. This can be done in 2 ways.
- Method 1 – surgical installation of a clip. This is a kind of “clothespin” located at the base of the aneurysm, so that it cannot burst.
- The 2nd method - endovascular - involves filling the bulge with spirals, ensuring its closure. This method is suitable for the treatment of aneurysms whose location is inaccessible to direct surgical intervention. The coils are inserted into the bulge using a special device inserted into the vascular system through a vessel in the groin.
Arteriovenous malformations
This is an abnormal collection of blood vessels between a cerebral artery and a vein. Its danger lies in the risk of bleeding, which can have serious consequences for a person. The goal of surgical and endovascular treatment is to eliminate abnormal blood vessels from the bloodstream.
During the intervention, the skull is opened, penetration into the area where the vascular anomaly is located, the vascular anomaly is closed or removed, thereby preventing possible bleeding. After the procedure, the surgical wound is restored. The operation lasts about 4-6 hours.
An alternative to surgical treatment is an endovascular procedure.
Carotid endarterectomy
Over the course of a person's life, atherosclerotic deposits and plaques form in the blood vessels, gradually closing the vessels. If this occurs in the area of the cervical (carotid) artery, the blood supply to the brain is compromised. The next complication is the risk of tearing off part of the plaque blocking the arteries of the brain, which causes an ischemic stroke.
Carotid endarterectomy involves opening the artery, removing the plaque and restoring its patency. It is recommended not only for patients with a history of stroke, but also as a preventive measure. The procedure is performed using a microscope under local anesthesia, i.e. the patient is conscious. In some cases, general anesthesia is appropriate; in this case, continuous monitoring of the patient's neurological function (also called electrophysiological evoked potential monitoring) and cerebral artery patency is necessary.
Carotid endarterectomy may be performed as an emergency treatment in the event of sudden cranial artery occlusion. This will help prevent serious injury or death.
Microvascular decompression of the cephalic nerves
Vascular pressure on the brain nerves can cause problems that develop with age. As a rule, we are talking about trigeminal neuralgia (acute pain in the center of the face) or facial hemispasm (uncontrollable jerking in half of the face). Microvascular decompression of the head nerves consists of removing the nerve contact with the vessel, which is deviated, fixed in a new position with special glue.
Extra-intracranial anastomoses
This is a microsurgical procedure aimed at improving blood supply to the brain, usually when the cervical artery is closed with subsequent insufficient blood supply to the brain. Indications are based on a study of cerebrovascular reserve. The intervention itself consists of connecting the artery supplying the soft tissues of the head with the cerebral artery, providing “new” blood flow to the organ.
Endoscopic therapy of the brain
Brain endoscopy is an intervention in which an endoscope, an instrument with a camera, is inserted into the brain to see structures and perform therapeutic procedures. Purpose of endoscopy:
- visualization of the state inside the brain;
- performing a biopsy - taking a tissue sample for further examination;
- creating an opening for the outflow of cerebrospinal fluid.
The endoscope is inserted through a drilled hole in the skull. The intervention lasts about 2 hours and is performed under general anesthesia. The head is usually not completely shaved; shaving near the endoscope insertion site is sufficient.
Complications are rare and are mainly represented by bleeding at the insertion site of the endoscope. After surgery, you may experience headaches that are responsive to painkillers. Sometimes dizziness occurs. The hospital stay after the procedure is usually 7 days until the stitches are removed.
Surgical treatment has no effective alternative.
Stereotactic brain surgery
Stereotaxis is a therapeutic method when the doctor does not directly see the structures on which he performs the operation. The brain structure is pre-focused mainly according to planning magnetic resonance; the exact target is achieved using a computer and a stereotactic device.
The purpose of stereotaxis is to perform a biopsy, drainage of fluid (blood, pus), and insert an electrode or therapeutic substance into the brain. In the case of treatment of movement disorders by inserting an electrode, the operation is performed with local anesthesia, because the patient must cooperate. It takes 1-2 hours. There is no need to completely shave your head, just shave around the electrode insertion point.
Complications may include sampling failure (i.e. failure to make a diagnosis) or bleeding during lead insertion. After the intervention, headache responsive to analgesics is possible. Postoperative hospitalization is approximately 7 days, usually until sutures are removed or biopsy results are obtained.
Craniotomy, Craniectomy and Cranioplasty
Craniotomy, craniectomy and cranioplasty sound similar, but are three different methods of brain surgery. As the names suggest, the cranium (skull) is involved in all three methods. As mentioned earlier, in a craniotomy, part of the head is temporarily removed to allow access to deeper parts of the brain to remove tumors, blood clots, brain tumors, foreign bodies and treat some other problems as mentioned in previous sections of the article. The bone flap is placed in place at the end of the operation and secured with titanium plates and screws.
On the other hand, with a craniectomy, the bone flap is not replaced immediately. Typically, neurosurgeons prefer this method when the problem is traumatic brain injury and other head injuries that involve swelling. The removed portion of the skull is kept away to relieve pressure and compression on certain areas of the brain.
In the third technique, cranioplasty, a bone flap is removed, just like the previous two methods. However, it never reattaches because the removed part of the skull itself has problems: it is damaged or cancerous. Thus, the removed part is replaced with titanium, acrylic or a synthetic bone substitute. Installation of the new part must also be performed by a neurosurgeon.
Relieving pressure in an emergency is one of the main advantages and specific characteristics of cranioplasty. It can save lives with this particular benefit. Another specific benefit of cranioplasty is that the new piece of bone can help restore the natural contour of the skull. Sometimes the removed part distorts the skull, but cranioplasty can help restore the natural shape. Titanium implants are especially preferred for cranioplasty due to their many benefits.
Indications and contraindications for surgery
The operation is indicated in the following cases:
- actively developing tumor;
- a tumor that does not tend to grow, but has a negative effect on parts of the brain, i.e., it compresses and blocks blood vessels, nerve trunks, and receptors;
- the tumor is located in an easily accessible segment of the brain and the likelihood of developing complications after surgery is minimal;
- a benign tumor, the development of which increases the chance of its degeneration into a malignant form.
Despite the fact that only conservative treatment is fatal in almost 100% of cases, sometimes doctors refuse to operate on a patient.
This decision is made in cases where surgical intervention is dangerous due to the presence of background pathologies:
- elderly patient;
- general exhaustion of the body;
- metastases to surrounding tissues;
- the tumor is located in a hard-to-reach place;
- the prognosis for survival after removal is lower than the prognosis for survival with a neoplasm.
Use of titanium implants in Cranioplasty
As mentioned in the previous section, with cranioplasty, the removed part of the skull cannot be put back. It is either damaged, malignant, or has other problems and should not be replaced. Therefore, it is necessary to use an implant made of titanium, PEEK, acrylic or a synthetic bone substitute.
Titanium is one of the most common materials used for surgical purposes and implants. It is also becoming increasingly popular in cranioplasty as it prevents cosmetic deformity, reduces the vulnerability of exposed brain tissue, and minimizes the risks and costs associated with additional surgeries and procedures. .
Brain surgery can be a minimally invasive approach such as a brow craniotomy, a right frontal craniotomy for tumor resection, or cranioplasty, where part of the skull is discarded and a piece of titanium or other materials replaces it. However, the patient should know enough about the operation, its preparation and its risks to minimize post-operative dangers as much as possible. .
Modern operating rooms
In order to provide the highest quality treatment, the operating rooms of neurosurgery centers are equipped with the latest advances in modern medicine. For the treatment of tumors and vascular diseases, an operating microscope is used, which is capable of performing fluorescent procedures that increase the accuracy of operations. This is the latest generation device with three-dimensional image transmission, thanks to which it is possible to perform complex interventions on the brain and spinal cord without complications.
Neuronavigation is used to conduct safe interventions. This computer system allows neurosurgeons to perform precise manipulations without the slightest damage to vital structures. And to eliminate hydrocephalus, neurosurgery centers perform special neuroendoscopy.
In addition to hardware equipment for surgical procedures, brain and spinal cord neurosurgery centers in Germany actively use intraoperative diagnostics (intraoperative ultrasound and x-ray examination). In addition, neuromonitoring and functional analysis are used to identify dysfunctions of the nervous system during surgery and correct them immediately.
Treatment approaches
The patient requires urgent hospitalization and medical care. After normalization of health, it is necessary to undergo in-depth diagnostics (computed tomography and MRI, cerebrospinal fluid sampling). After consultation with a neurosurgeon, treatment is prescribed.
There are two treatment options for the disease:
- Conservative. The neurologist prescribes treatment, taking into account the individual characteristics of the body and the diagnostic results. Conservative treatment consists of taking medications. The patient is prescribed drugs to regulate intracranial pressure and cerebral edema, antispasmodics, antihypertensive drugs, calcium antagonists. Intensive use of medications is necessary in the acute stage of hemorrhagic stroke. The patient also needs to be observed by a doctor to diagnose a decrease in cerebral edema.
- Surgical treatment of hemorrhagic stroke. Before performing an operation, doctors must exclude contraindications, stabilize the patient’s condition, and study the results of neuroimaging in detail. Surgical treatment of stroke cannot be avoided if a hemorrhage of medium or large volume occurs. Specialists choose the type of intervention.