home
/
Branches and centers
/
Headache Treatment Center
/
Headache due to neuralgia of the greater occipital nerve
Branches and centers
Treatment methods
Diagnostic methods
Diseases and symptoms
Headache caused by neuralgia of the greater occipital nerve occurs in 40% of patients. This is a signal from the body about the presence and development of serious problems. Unpleasant sensations suffered are often confused with migraine attacks, and when diagnosing, it is sometimes quite difficult for doctors to differentiate the original source of the problem. Without timely identification of a harmful process and competent treatment, significant progress of the pathology and deterioration of the condition is observed.
Important information
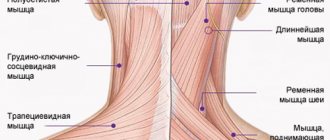
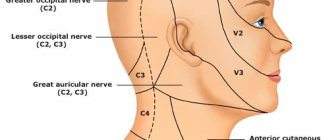
Unpleasant, often debilitating symptoms begin in the occipital area, since 2 large occipital nerves provide innervation to this particular segment.
These nerves begin to form from branches of the posterior region of the spinal nerve (C2). The nerve fibers are located first around the inferior oblique muscle of the head, and then pass through the semispinalis muscle along with the trapezius tendon and, as a result, break up into several branches in the skin of the occipital region of the head, partially affecting the parietal region.
How not to confuse the cause of a headache?
Sufferers complain of unilateral or bilateral jerking and shooting pains that easily spread from the back of the head to the crown, sometimes reaching the forearms and shoulder blades. The duration of unpleasant symptoms varies: from a few seconds to several minutes. The number of such attacks is also individual, usually increasing with the development of pathology. Also noticed are persistent dull pains, which are replaced by attacks of sharp, twitching pain.
The torment intensifies when pressure is applied to the highest nuchal line, at the highest point of attachment of the muscles of the back and occipital bone. This deterioration is due to the fact that the greater occipital nerve passes in the area bordering the larynx.
Some patients complain of a throbbing, burning pain in the scalp, while others note a loss of sensitivity in the problem area.
Stress, prolonged mental and physical stress lead to an increase in such pain, and the trapezius muscle often contracts.
Shooting pain in the head is a symptom of neuralgia
Shooting pain in the head is a common symptom of cranial neuralgia. The most common neuralgia is the trigeminal nerve, which has three large branches going to the upper, middle and lower parts of the face. According to the damage to one of the branches, the symptoms will differ:
- Pain in the forehead, eyes - when the first branch is affected.
- Pain in the cheek and temple area is the second branch.
- Pain in the lower jaw, ear, temple - the third branch.
In practice, symptoms can be combined, since the innervation zones of the branches of the trigeminal nerve overlap slightly. The pain always occurs on one side - left or right, never moving to the opposite side.
The causes of neuralgia can be hypothermia, trauma to the nerve, or pinching of it at the point where it exits the skull. Neuralgia is often combined with herpetic rashes on the skin in the area of pain, which indicates penetration of the herpes virus into the ganglion of the trigeminal nerve.
Shoots in the head with neuralgia suddenly, without any warning signs. Usually it is provoked by hypothermia of the face in the cold, cold wind, washing with cold water, shaving, chewing. Along with pain, sensitivity may decrease, numbness and “pins and needles” appear, which usually indicates involvement of a nerve ganglion in the process.
Causes
This type of headache occurs due to neuralgia of the greater occipital nerve. This symptom appears due to immediate primary (idiopathic) neuralgia, when nerve fibers are pinched without obvious reason. The most common problem is the consequences of pathologies:
- degenerative changes in the spine in the cervical region (osteochondrosis, intervertebral hernia, protrusion);
- injuries;
- poor circulation in this area;
- malignant and benign neoplasms;
- presence of infectious agents;
- endocrine system disorders.
Also, such a headache often begins due to hypothermia, low activity and heavy physical exertion.
Headache due to neurosis and neurasthenia: treatment with psychotherapeutic techniques
A special group that requires special treatment are headaches due to neurosis and neurasthenia. The nature of neurotic pain is very diverse and presents some difficulties in diagnosis. Patients describe a wide variety of complaints, which sometimes mislead the doctor.
Treatment of headache symptoms due to neurosis and neurasthenia, in addition to drug therapy, necessarily includes techniques aimed at working through the initial neurotic conflict. In this case, both psychotherapeutic methods and psychoanalytic practice can be used to help relieve neurotic tension and identify the causes of the painful accumulation of such tension.
Our specialists have all the necessary knowledge and extensive experience to help provide effective treatment for neurological headaches in the shortest possible time! Just dial +7(495) 798-30-80!
The text was checked by expert doctors: Head of the socio-psychological service of the Alkoklinik MC, psychologist Yu.P. Baranova, L.A. Serova, a psychiatrist-narcologist.
CAN'T FIND THE ANSWER?
Consult a specialist
Or call: +7 (495) 798-30-80
Call! We work around the clock!
Objective examination of patients
The greatest challenge in diagnosis is the exclusion of problems in the third occipital nerve, since the innervating areas are close. However, in a situation with neuralgia of the greater occipital nerve, unpleasant sensations are observed closer to the center of the occipital region.
Diagnosis begins with examination and palpation. If a patient complains of vague or obvious discomfort when pressing on the occipital region, as well as the area behind the ears and the mandibular fossa, neurologists immediately assume occipital neuralgia. Also, thickening in the area of the C2-C3 facet joints can confirm the diagnosis.
Increased sensitivity of the occipital nerve is confirmed by a kind of test: the doctor moves his finger with a gentle movement in an area 2-3 cm from the external occipital protrusion.
The following diagnostic tests are also prescribed:
- MRI or CT;
- X-ray;
- Ultrasound.
Using such methods, it is possible to recognize existing pathologies of the cervical spine.
The patient's blood is taken for testing to look for infections and other problems.
TREATMENT OF MIGRAINE AND SOME FORMS OF PAROXYSMAL MIGRAINE-LIKE HEADACHE OF VASCULAR GENESIS
The paper describes treatment policy for migraine, cluster headache, chronic paroxysmal hemicrania, lower facial and cervical migraine is described. Each section outlines the characteristic clinical signs of different types of migraine and other paroxysmal vascular headaches. V.N. Shtok - Doctor of Medical Sciences, Prof., Head. Department of Neurology, Russian Medical Academy of Postgraduate Education
VN Shtok - prof., MD, Head, Department of Neurology, Russian Medical Academy of Postgraduate Training
TO
The group of paroxysmal headaches of vascular origin includes various forms of migraine proper, cluster headache, chronic paroxysmal hemicrenia, migraine of the lower half of the face. In all these cases, the pathogenesis is based on hereditary or congenital inferiority of neurohumoral regulation and/or endocrine homeostasis. “Cervical migraine” of vertebrogenic origin stands apart.
Migraine
Migraine is manifested by attacks of pain (often pulsating) in the frontotemporo-orbital region, spreading to half the head (hemicrania). It begins more often in the time interval from puberty to the beginning of the third decade of life. The further course is unpredictable: attacks can end with the end of puberty or continue with varying frequencies throughout life. In the latter case, the frequency of attacks is influenced by various factors: unhealthy lifestyle, household or work stress, changes in habitual climatic conditions, food, medicinal and other allergens. The following symptoms are characteristic of different types of migraine: localization of pain, often unilateral, attack duration is several hours, photo- or phonophobia, the appearance of nausea or vomiting at the height of the attack. During an attack, the patient is unable to work, and usual household activities are reduced. The patient seeks to retire, go to bed, and fall asleep. It is necessary to emphasize the individual stereotypic nature of the course of the attack in each patient. According to the proposals of the international commission of experts on the classification and diagnosis of headaches, within the framework of migraine itself, migraine without aura and migraine with aura are distinguished. Migraine without aura
(former name - simple, ordinary) is characterized by the onset of an attack without any pronounced disorders immediately before its onset.
However, patients may experience dysphoria, irritability, changes in appetite, and water retention for several hours before the attack (women often pay attention to this). The combination of these symptoms is called precursors. Migraine with aura
is characterized by the occurrence of an aura, often before, less often simultaneously or against the background of a full-blown attack of pain.
This type includes migraine, previously called classical (ophthalmic), in which the aura manifests itself either as sparkling dots, zigzags or partial loss in any quadrant or half of both visual fields, which indicates discirculation in the cortical branches of the posterior cerebral artery supplying the visual analyzer . Retinal (retinal) migraine
is distinguished from the ophthalmic type , in which visual impairment in one eye (vision in the other eye is usually not impaired) is manifested by blurring, the impression of falling flakes or the movement of black flies.
These disorders are caused by discirculation in the central retinal artery. Usually the visual aura in both cases precedes an attack of pain. The duration of the aura is individual - from several seconds to several minutes. Sometimes after the end of the aura there is a short “light” interval before the onset of pain. Another form of aura (formerly called associated migraine) is distinguished by the occurrence before or at the beginning of a painful attack of various neurological disorders - hemiparesis, hemidysesthesia, aphasia, vestibulocerebellar symptoms, mental (dysphrenia), which indicates dyscirculation in different areas of the cortex or brain stem, or the appearance somatic symptoms (pain in the chest or abdomen) as signs of transient dysregulation of the function of internal organs. Attacks that repeat without a break for 2-5 days are called status migraine
.
If the associated symptoms are observed within a few days or hours after the attack, they are said to have a complicated migraine. In such cases, a more in-depth examination is necessary to exclude arterial or arteriovenous aneurysm of the cerebral vessels. If all or most of the attacks occur during menstruation, such migraine is called catamineal (menstrual). Treatment for a migraine attack.
The most effective drugs are 5-HT1-serotonin receptor agonists -
sumatriptan
, zolmitriptan.
During an attack, sumatriptan is prescribed orally in tablets of 0.1 g no more than twice a day, or 6 mg of the drug is administered subcutaneously (in an ampoule 6 mg of sumatriptan succinic salt dissolved in 0.5 ml of distilled water) also no more than twice a day. Sumatriptan is not used orally or by injection at the same time, and it is not combined with ergotamine medications. The drug is contraindicated in pregnancy, angina pectoris and intermittent claudication. Another effective remedy is ergotamine hydrotartrate
, which has a vasoconstrictor effect.
A single dose should not be prescribed more than 2 mg of the drug orally or 4 mg in a suppository (no more than 8-10 mg/day). With the rapid development of the pain phase, 0.25-0.5 ml of a 0.05% ergotamine solution is injected into a muscle or vein. Overdose leads to the development of ergotism. Ergotamine is part of such drugs as ginergin, gynofort, neogynofort, ergomar, secabrevin, belloid, acliman. Among the ready-made drugs, caffeine, a combination of ergotamine and caffeine, has proven itself well. The drugs should be taken when the first signs of an attack appear, since gastric stasis later develops, and drugs taken orally are not absorbed. Metoclopramide (intramuscularly, orally or in suppositories a few minutes before taking an analgesic or ergotamine) accelerates gastric emptying and absorption of the analgesic. The attack can be stopped with dihydroergotamine
- 5-20 drops of a 0.2% solution orally (0.002 g in 1 ml), or subcutaneously 0.25-0.5 ml of a 0.1% solution (0.001 g in 1 ml) 1-2 times a day, or nasal spray (1 dose in each nostril - maximum 4 doses during an attack).
You can add antihistamines, sedatives and sleeping pills. When individually selecting effective drugs for the treatment of an attack, the following combinations of ergotamine with analgesics are recommended: ergotamine + amidopyrine + acetylsalicylic acid; ergotamine + caffeine + indomethacin; ergotamine + paracetamol + codeine phosphate + caffeine. In such combinations, each drug is prescribed in half the average therapeutic single dose. Treatment for status migraine
is carried out in a neurological hospital.
50-75 mg of a soluble prednisolone preparation - prednisolone hemisuccinate - is administered intravenously (drip) (ampoule contents - 0.025 g - dissolved in 5 ml of water for injection, preheated to 35-37 ° C; for drip administration, the resulting solution is diluted in 250-500 ml isotonic sodium chloride solution, 5% glucose solution or polyglucin), dihydroergotamine or injectable acetylsalicylic acid aspisol (contains 1 g of dry matter in 1 ampoule - 0.9 g of lysine monoacetylsalicylate, 0.1 g of aminoacetic acid and corresponds in activity to 0.5 g acetylsalicylic acid, in another ampoule 5 ml of solvent - water for injection). A freshly prepared aspisol solution is injected slowly into a vein or deep into a muscle. For drip intravenous infusion, this solution is diluted with 250 ml of isotonic sodium chloride solution or in a 5% solution of glucose or polyglucin. Sumatriptan or ergotamine is prescribed (avoid overdose!). Dehydrating agents (furosemide), neuroleptics (aminazine, haloperidol, thioridazine), diazepam, antihistamines, hypnotics and antiemetics are used. For local anesthesia, a 0.25% solution of bupivacaine hydrochloride (0.1-0.2 mg/kg) in a 10% glucose solution (over 30 minutes) is offered into a vein. Good results are obtained by a combination of intravenous injections of aminophylline with glucose, dehydrating and antihistamines. Due to the increase in the level of lactate in the cerebrospinal fluid during migraine status, drip infusions of sodium bicarbonate are recommended. Narcotic analgesics usually have no effect, but often increase vomiting. Interictal treatment of migraine
is prescribed for frequent (at least 1 per week) and severe attacks leading to temporary disability.
The most widely recognized are the so-called antiserotonin drugs.
One of these drugs - cyproheptadine (12 mg/day), pizotifen (1.5 mg/day), methysergide (6 mg/day) or iprazochrome (7.5 mg/day) - is prescribed daily.
It is advisable to start treatment on interictal days. The duration of the course is 3-6 months, depending on the effectiveness, presence and severity of adverse reactions. Cessation or a sharp decrease in the frequency and severity of attacks is observed in 50-70% of patients. Antidepressants have serotonergic properties. The doses of amitriptyline recommended for course treatment range from 10 to 175 mg/day. Monoamine oxidase inhibitors are not used for prolonged courses due to toxicity and adverse reactions. β-blockers are effective: treatment with propranolol at a dose of 120-240 mg/day reduces the frequency and severity of attacks in 80% of patients. The b-blocker nadolol can be taken once a day (20-80 mg). The effectiveness of oxprenolol and pindolol is significantly lower than that of propranolol. Selective b-blockers are usually ineffective. The effectiveness of propranolol increases when used in combination with pizotifen, and the dose of each drug can be halved. Given that b-blockers and ergotamine cause peripheral vasoconstriction, they should not be prescribed simultaneously. The action of clonidine is similar to that of b-blockers. During a course of treatment, clonidine at a dose of 0.150-0.235 mg/day reduces the frequency and severity of attacks in 52-61% of patients. Treatment with b-blockers and clonidine is advisable to use in patients with hypertension. For interictal treatment, non-steroidal anti-inflammatory drugs (NSAIDs) are used - acetylsalicylic acid (15 mg/kg per day), ketoprofen (100-200 mg/day), piroxicam (20 mg/day), naproxen (550 mg/day), mefenam, flufenamic and tolfenamic acids (250-500, 400 and 300 mg/day, respectively); dihydrogenated ergot derivatives - dihydroergotamine (1 mg/day), dihydroergotoxin at a dose of 4.5 mg/day, nicergoline - 15 mg/day orally for 2-3 months; calcium antagonists: cinnarizine (225 mg/day), flunarizine (9 mg/day), verapamil (80-160 mg/day), diltiazem (180 mg/day), nimodipine (120 mg/day). Course duration is 8-15 weeks. For menstrual migraine,
treatment with NSAIDs in the above doses or bromocriptine (2.5-5 mg/day) gives a good effect 3-5 days before the start of menstruation. Bromocriptine is contraindicated in patients with syncopal migraine. If such treatment is ineffective, gestagenic drugs are used: 2.5% solution of progesterone in oil, 1 ml per muscle every other day 10-14 days before menstruation or 6.5% (12.5, 25%) oil solution of oxyprogesterone capronate with prolonged action 1 ml per muscle 1 time 10 days before menstruation. Sometimes taking pregnin 0.01 g 2 times a day for 6-7 days is effective. In resistant cases, testosterone propionate is prescribed 0.05 g 2 times a day. Patients in whom interictal migraine treatment does not have an effect should undergo electroencephalography. When epileptiform activity is detected on the EEG, anticonvulsants are used for interictal treatment: finlepsin 0.2 g 2 times a day or phenobarbital 0.05 g 2 times a day, sodium valproate 0.6 g 2 times a day (optimal plasma concentration 700 mmol/l). The choice of drugs for interictal treatment should be determined by pharmacotherapeutic logic. Thus, young patients suffering only from migraine are prescribed pizotifen or iprazochrome; in the presence of orthostatic episodes and arterial hypotension, dihydroergotamine is prescribed; with concomitant arterial hypertension - clonidine or b-blockers, dihydroergotoxin, calcium antagonists; for depressive syndromes - antidepressants, for menstrual migraine - NSAIDs or bromocriptine (especially with an increase in plasma prolactin levels); for paroxysmal changes in the EEG - anticonvulsants (phenobarbital, carbamazepine). The condition of patients in the interictal period can be different: from almost complete health to almost daily manifestations of certain forms of vegetative-vascular dystonia. Among the latter, the most common headache is venous insufficiency - a bursting pain (heaviness) in the back of the head or the entire head, which requires the prescription of xanthine drugs. The choice of drugs for the treatment of interictal manifestations of vegetative-vascular dystonia is determined individually. In most cases, it is advisable to combine them with tranquilizers. In all cases, for successful relief of attacks and interictal treatment, it is necessary that the patient maintain a healthy lifestyle, avoid mental and physical stress, as well as exposure to provoking factors.
Cluster headache
From the previous names - Horton's syndrome, erythromegalgia of the head, group attacks of pain - a more accurate description of the symptom complex can be considered Harris' periodic migraine neuralgia. The disease most often begins between the ages of 25 and 30 years. About 70% of patients are men. An attack of pain occurs suddenly in the periorbital region and behind the eye (“the eye bulges”), radiates to the frontotemporal, zygomatic region, sometimes along the entire half of the face, to the neck; the pain is burning, cutting, bursting. Patients scream, moan, cry, and experience psychomotor agitation. On the side of pain, the skin of the face turns red, injection of scleral vessels, Horner's sign are noted, the eye is watery, half of the nose is stuffy. There are no harbingers or auras. The duration of the attack ranges from 15 to 30 minutes, usually does not exceed 2 hours. There are several attacks during the day, at least one at night. Periods of exacerbation occur mainly in spring or autumn. The duration of an exacerbation ranges from 4 to 10 weeks, after which it passes spontaneously. Light intervals between exacerbations range from six months to several years. During such intervals, patients are practically healthy. Attacks can be triggered by any factor that causes vasodilation. Cases of chronic cluster pain without light intervals have been described, although it is possible that in these cases we are talking about an intermediate form, close to chronic paroxysmal hemicrania (see below). To treat attacks during periods of exacerbation, inhalation of 100% oxygen (7 l/min for 3-5 minutes) is prescribed in combination with 2 mg of ergotamine orally and local anesthesia of the pterygopalatine ganglion with a 4% lidocaine solution or a 5-10% cocaine hydrochloride solution. For a course of treatment of episodic attacks, it is advisable to use prednisolone (0.02-0.04 g) and pizotifen in combination with a single dose of 2 mg of ergotamine at night. For frequent attacks, a combination of lithium carbonate (0.3 - 0.6 g/day) with prednisolone is preferable; The H2 receptor blocker cimetidine is also used (0.6 - 1.2 g/day). There is evidence of the effectiveness of ketotifen prescribed at 3 mg/day for 8 weeks, as well as a combination of cofergot (caffeine + ergotamine) with triamcinolone (4 mg). This combination of drugs is prescribed 3-4 times a day, after a week the dose of triamcipolone is gradually reduced over the course of a week, and for the next week the patient takes only ergotamine with caffeine. The use of interictal treatment for ordinary migraine (see above) gives rare, but sometimes amazing results; the exacerbation can be stopped on the 5-7th day. In some cases, for treatment it is necessary to try all the remedies recommended for the treatment of status migraine (see above). One way or another, after the individual period of exacerbation, which is quite specific in duration, has passed, cluster pain goes away spontaneously. The patient must be informed about this feature, which calms him to a certain extent.
Chronic paroxysmal hemicrania
Chronic paroxysmal hemicrania is distinguished by the fact that attacks resembling a simple migraine are usually short-lived (up to 40-60 minutes), but are repeated many times a day and occur daily for many months. There is a high sensitivity to treatment with indomethacin. Hence the name “indomethacin-sensitive headache (hemicrania).” Sometimes chronic hemicrania, which lasts for months, resolves after 1-2 days of treatment with indomethacin. The drug is prescribed 25 mg 3 times a day. After the attacks stop, switch to a maintenance dose of 12.5-25 mg/day. In the absence of contraindications to the use of NSAIDs, multi-month treatment is recommended, since after short-term courses attacks recur. The question of the “transitional” form between cluster periodic pain and chronic paroxysmal pain - chronic cluster pain - remains controversial. For treatment, indomethacin is first prescribed, and if the effect is insufficient, it is necessary to use drugs for the treatment of cluster headaches.
Migraine of the lower half of the face
Migraine of the lower half of the face (carotidynia, caroticotemporal syndrome, facial angioneuralgia) is manifested by attacks of pulsating pain in the lower half of the face with irradiation to the orbital area, temple, and neck. The carotid artery in the neck is painful on palpation. The duration of the attack is from several hours to 3 days. It can appear in two forms. In young and middle-aged patients, the disease begins acutely. It is believed that this form of infectious-allergic etiology, although the effectiveness of steroids and antihistamines in these cases has not been confirmed. Analgesics are prescribed. Another form occurs in the elderly and is very similar to simple migraine. Antimigraine drugs are effective. Differential diagnosis with different forms of facial pain (prosopalgia) - cranial neuralgia and/or ganglioneuralgia - can be difficult. In these cases, the use of drugs prescribed for neuralgia is justified: antiepileptics (carbamazepine, ethosuxemide, trimethine, clonazepam, morpholep) in combination with neuroleptics or tranquilizers, as well as analgesics.
Cervical migraine
Other names for this form: posterior cervical sympathetic syndrome, vertebral artery syndrome, Barré-Lieu syndrome. The syndrome is caused by irritation of the sympathetic plexus of the vertebral artery passing in the canal formed by holes in the transverse processes of the cervical vertebrae, by a pathologically altered cervical spine with its osteochondrosis and deforming spondylosis, as well as by excessive mobility (pathological instability) of the cervical vertebrae even in the absence of osteochondrosis. These changes are revealed by radiography, in particular on lateral radiographs during flexion and extension of the head. The name “migraine” is due to the hemicranial localization of an attack of throbbing pain, starting from the cervical-occipital region and spreading to the entire half of the head. Retro-orbital pain is characteristic, and visual disturbances may resemble the aura of ophthalmic migraine. These disorders, as well as concomitant cochleovestibular and cerebellar disorders (hearing loss, noise and ringing in the ears, systemic and non-systemic dizziness, staggering when walking) are caused by discirculation in the vertebrobasilar zone. Attacks can be short-term (“small”), lasting several minutes, and long-term (“large”), lasting several hours. The structure of subjective and objective symptoms varies widely individually. Seizures are triggered by bending or straightening the head. An awkward position of the head and neck in bed causes night attacks that wake the patient (“alarm clock” headache). In the treatment of vertebrogenic cervical migraine, orthopedic measures are of great importance: wearing removable collars, using special orthopedic pillows for night sleep, careful massage and therapeutic exercises that strengthen the “muscle corset” in the cervical region. Drug treatment includes tranquilizers to relieve psycho-emotional stress and muscle relaxation, antidepressants to correct depression. For frequent attacks, a combination of indomethacin is prescribed to inhibit pathological impulses from the structures of the cervical spine and an a-blocker (nicergoline or dihydroergotoxin). The drugs are prescribed 1 tablet 3 times a day. If the effect is insufficient, other vasoactive drugs are successively tried: vinpocetine, cinnarizine, calcium antagonist nimodipine. For pathological “stagnant” muscle tension in the cervical-occipital region, local blockades with novocaine (5-10 ml of 0.5-1% solution) and hydrocortisone are recommended. As the exacerbation and frequency of attacks subsides, physiotherapeutic procedures are prescribed: ultraviolet irradiation, ultrasound, sinusoidal and diadynamic currents, mud applications (35-36°C) to the paravertebral zones of the neck. If a stable orthopedic defect (subluxation of the cervical vertebra) is identified, manual therapy is carried out with great care, involving a highly qualified specialist. Surgical treatment with decompression of the vertebral artery is indicated in cases where the progression of the disease leads to disability of the patient, and conservative treatment is ineffective.
Literature:
1. Olesen J. Diagnosis of headache // Neurological journal. - 1996. - No. 3. — P. 4-11. 2. Shtok V.N. Headache. M.: Medicine, 1987, 303 p. 3. Shtok V.N. Pharmacotherapy in neurology. M., 1995. - pp. 110-113, 200. 4. Classification Committee of International Headache Society. Classification and Diagnostic Criteria for Headache disorders, Cranial Neuralgia and Facial Pain. Cefalgia 8 (Suppl. 1.7.):1-98.
Effective treatments
Only a complex of therapeutic techniques can help in getting rid of headaches caused by neuralgia of the greater occipital nerve.
In Samara, competent specialists from First Neurology are successfully coping with the problem. To eliminate pain, the patient is offered:
- Drug blockade of the exit points of the branches of the greater occipital nerve. In this case, minimal injections of analgesics are used throughout the problem area. Medicines are chosen depending on the individual characteristics of the patient.
- Transcranial magnetic stimulation (TMS). The cerebral cortex is exposed to short magnetic pulses. As a result, not only does the pain go away, but brain function also improves.
- Dosing traction of the cervical spine. The procedure is necessary for obvious decreases in the clearance between the vertebrae, which appear as a result of osteochondrosis and other degenerative problems.
A successful result appears thanks to the German Zimmer physiotherapeutic equipment, which allows you to combine several effective techniques at once:
- Ultrasound therapy;
- Electrophonophoresis using analgesic and anti-inflammatory medications
- Vacuum massage.
If you are tired of incessant headaches in the back of your head, contact the First Neurology clinic.
Treatment of occipital neuralgia
Sympathetic blockade
- Cost: 8,200 rub.
- Duration: 15-30 minutes
- Hospitalization: 2 hours in hospital
More details
At the CELT Pain Clinic, medical and surgical treatment methods are used to treat occipital neuralgia:
Drug treatment
Drug treatment methods are aimed at reducing pain. For this purpose, anticonvulsants and muscle relaxants are prescribed. In addition, massage and rest are prescribed.
A procedure called nerve block has proven itself well in our Pain Clinic. It consists of injecting the drug directly into the affected area, thereby achieving a long-lasting pain relief effect.
Surgery
If pain lasts a long time, is pronounced, or if conservative treatment does not bring the desired result, our specialists will recommend the following:
- pulsed radiofrequency ablation of the occipital nerves;
- stimulation of the occipital nerves - involves conducting electrical impulses through the nerves that block pain;
- microvascular decompression - involves the use of microsurgical techniques that eliminate compression of the nerves, and therefore the pain itself.
It is worth noting that occipital nerve stimulation is a minimally invasive method that does not have similar effects and is absolutely painless.
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
Our specialists
Tarasova Svetlana Vitalievna
Expert No. 1 in the treatment of headaches and migraines. Head of the Center for the Treatment of Pain and Multiple Sclerosis.
Somnologist.
Epileptologist. Botulinum therapist. The doctor is a neurologist of the highest category. Physiotherapist. Doctor of Medical Sciences.
Experience: 23 years.Derevianko Leonid Sergeevich
Head of the Center for Diagnostics and Treatment of Sleep Disorders.
The doctor is a neurologist of the highest category. Vertebrologist. Somnologist. Epileptologist. Botulinum therapist. Physiotherapist. Experience: 23 years.
Bezgina Elena Vladimirovna
The doctor is a neurologist of the highest category. Botulinum therapist. Physiotherapist. Experience: 24 years.
Palagin Maxim Anatolievich
The doctor is a neurologist. Somnologist. Epileptologist. Botulinum therapist. Physiotherapist. Experience: 6 years.
Mizonov Sergey Vladimirovich
The doctor is a neurologist. Chiropractor. Osteopath. Physiotherapist. Experience: 8 years.
Drozdova Lyubov Vladimirovna
The doctor is a neurologist. Vertebroneurologist. Ozone therapist. Physiotherapist. Experience: 17 years.
Zhuravleva Nadezhda Vladimirovna
Head of the center for diagnosis and treatment of myasthenia gravis.
The doctor is a neurologist of the highest category. Physiotherapist. Experience: 16 years.
Read also
Tension headache
Tension headache (TTH) is one of the most common types of headache that periodically occurs in anyone, even an absolutely healthy person.
It does not pose a serious threat to... Read more
Overuse headache (Headache caused by excessive medication)
Frequent headaches are a good reason to immediately contact a neurologist. Otherwise, you can miss the onset of a serious illness or lead yourself to the formation of an abusive headache...
More details
Headache treatment
Tarasova Svetlana Vitalievna. Expert No. 1 in the treatment of headaches and migraines. Head of the Multiple Sclerosis Center. Neurologist of the highest category. Doctor of Medical Sciences Migraine is one...
More details
Migraine
Migraine or headache seriously worsens a person's condition, especially with frequent attacks - chronic migraine. At the same time, people often do not take migraine seriously, not even thinking about seeing a doctor.…
More details
Monoclonal antibodies against migraine
About 11% of people in the world suffer from migraines, and a third of them are forced to stay in bed during attacks. This significantly reduces the quality of life: it interferes with work, communicating with friends and engaging in hobbies.…
More details
Acupuncture and laser therapy used in medical treatment for various types of headaches
Acupuncture and laser acupuncture are among the most important reflexology techniques. Thanks to their effect, pain impulses are suppressed and the threshold of excitability of pain receptors increases, caused by the normalization of the balance of pain modulators and mediators: norepinephrine, opiates, serotonin. In addition, the effect on biologically active points inhibits pathological processes that contribute to the development of headaches of various etiologies: with its help it is possible to relieve pathological tension in the head muscles, dystonia of extracranial and cerebral vessels, and reduce other pathogenic processes. Acupuncture and laser acupuncture are great for:
- migraine;
- vascular headache with cerebral angiodystonia, vegetative-vascular dystonia, regional cerebral hypotension, venous hypotension, hypertension, atherosclerosis;
- muscle tension headache;
- facial pain in psychopathy.
Get a free consultation
+7(495) 798-30-80