If you want to get advice on treatment in Moscow. Fill out the form below:
We are often asked for advice with this question. Indeed, relatives and the patient himself are often left to their own devices. As such, there is no state rehabilitation program yet. Moreover, we also do not have a universal answer.
One thing we know for sure is that all patients and their relatives have the same goal: a speedy restoration of function and a return to normal life. The goal is one, but the paths to it are different, often long and, sadly, dead-end...
When treating a stroke, the situation very often develops as follows. A man is admitted to the hospital. The life of family and friends changes dramatically. Anxiety for a loved one, changes in work schedule, financial costs for medications, caregivers and consultations. And when you get discharged, it turns out that everything is just beginning: equipping an apartment, hiring caregivers, or temporarily stopping work for one of your relatives. And the prices for rehabilitation make you feel uneasy...
Yes, everyone’s financial capabilities are different! Yes, many people have to rely only on themselves! Yes, there are no clear and understandable government programs, for example, for a heart attack!
- Well, no, no trial!
Let's try to calculate everything ourselves and make the right decision.
Americans, for example, are a mercantile people and far from stupid. They once calculated that every dollar invested in treatment, without further rehabilitation, turns into 17 dollars spent in the future. Let's just count in money. It is important. Just numbers Average monthly drug treatment for stroke: from 2 to 7 thousand rubles.
Depending on the degree of dysfunction, complications and concomitant pathologies. Let's add to this a nurse or the financial losses of relatives if they are present and caring for the patient. Another 20-30 thousand monthly. All methods of motor and speech rehabilitation cannot be implemented on your own. Whatever one may say, at the first stages you will have to invite specialists. Preferably at least. There are a lot of subtleties, no matter what they write on the Internet. This is also money. Now all that remains is to add up all these numbers and multiply by the number of months. At 6 for example...or at 12...
The numbers may, of course, vary. There are different types of strokes. And if you don’t look at the numbers, but think about the time for effective rehabilitation, which we already have little of. In the end, we need to put our loved one back on his feet. Return to society, learn to drive a car again. And this is possible in modern conditions. So it turns out that the amounts are ultimately comparable, but the effects and results are radically different.
If you have read this far and haven’t given up on this idea without taking our word for it, let’s look for solutions and minimize costs.
If you or your loved ones need medical assistance, contact us. The site’s specialists will recommend a clinic where you can get effective treatment:
The first way. Rehabilitation center after stroke
Even before discharge from the hospital, select a rehabilitation center based on the functional equipment, capabilities of the center and the patient’s condition. Many centers do not accept bedridden patients. This is a fact that must be taken into account.
Also, you can count on rehabilitation according to the so-called quota .
They don’t take seriously ill or bedridden patients, but if their condition allows it, it’s worth “fighting” for the quota. Naturally, commercial rehabilitation centers working according to European methods do not work according to quotas. But the approach, to put it mildly, varies. A distinctive feature of good centers is an individual approach, round-the-clock care and fast rehabilitation times with the maximum possible restoration of functions. There are also worthy centers among government institutions, but you won’t get away from the continuous approach.
What to bring to the hospital
Relatives do not always know what can be brought to the hospital after a stroke and often forget necessary things and bring prohibited food.
You can bring to the hospital:
- Toilet supplies (soap, toothbrush, comb).
- Change of clothes.
- Diapers. Even if a person with a stroke goes to the bathroom on their own, at night, due to the inability to quickly get out of bed, an annoying nuisance can occur. This usually occurs in older people.
- Convenient dishes. It is difficult for a patient after a stroke to drink from a glass, and a drinking cup can improve the comfort of self-service.
- Homemade food. People with hemorrhagic stroke or after acute ischemia need to follow a diet. But, despite the fact that the hospital provides adequate food, homemade food seems tastier. From food you are allowed to bring boiled cutlets, vegetable and fruit purees, stewed meat and fish without spices.
If the patient is bedridden, it is recommended to bring large wet wipes. This will make it easier to carry out hygienic treatment when changing diapers.
The second way. Combined approach
If you are denied a quota due to the patient's condition. In this case, you can combine the approach, and thereby, in fact, save the patient’s life. A short course of rehabilitation in a good paid center, and then rehabilitation under a quota. By the way! Even if you initially cannot pay for paid rehabilitation, be sure to visit good centers.
Show medical documentation, get advice from highly qualified specialists. At the very least, this will help you navigate the deadlines and outline a further rehabilitation plan. It is at least unreasonable to miss such an opportunity!
Where is the patient transferred from ARC?
Relatives of a stroke patient are interested in where they are transferred after resuscitation in order to be able to visit the person and provide moral support. It depends on the severity of the brain damage:
- uncomplicated cases are treated in hospital for 3 weeks, then follow-up treatment and rehabilitation are carried out on an outpatient basis;
- in case of a severe attack, the patient is transferred from the intensive care ward to the neurological department, where he can stay for a month or longer.
If the risk of a recurrent stroke attack remains or vital signs are not stable, then the patient remains in the anesthesiology and intensive care unit (ARO).
The third way. Recovery after a stroke at home
If this is the case, study as much information as possible. Information that is objective and adequate. You should not do the exercises “in a hurry.” An arm, then a leg. This is where the biggest mistake lies. Rehabilitation measures are only successful when they are applied systematically and continuously. Buy a rehabilitation manual in video format. Consult with really smart rehabilitologists. And be patient.
Whenever possible, try to get qualified help .
We apologize if the material in this article seemed harsh and uncompromising to you. But if you look at it, the lives, health and well-being of both patients and their relatives are at stake.
Take care of yourself!
Sick leave
Inpatient treatment only stabilizes the health condition, and then the person receives further treatment at home. A sick leave certificate after a stroke is opened in the hospital, and after discharge the stroke patient renews the document by visiting a doctor.
The duration of disability depends on the nature of the brain lesion:
- mild ischemic stroke is treated for about 3 months;
- a patient after surgery for removal of an intracranial term requires a minimum of four months of rehabilitation.
Sick leave after a stroke can be extended to 7-8 months. After this time has expired or if the doctor sees that full rehabilitation is impossible, the patient is sent to MSEC to receive disability.
Resuscitation in the early post-stroke period is one of the important stages of rehabilitation treatment. Intensive therapy helps prevent brain swelling and reduce the lesion. If a person has been taken away with a diagnosis of stroke, then there is no need to look for which department to treat stroke - patients after an acute attack are hospitalized in the ARC.
Treatment
Pre-hospital stage
An important task of the prehospital stage is collecting anamnesis (time of onset and changes in symptoms, concomitant diseases, medications taken).
Assistance to patients at the prehospital stage comes down to maintaining airway patency, stabilizing hemodynamic readings and transporting to the nearest vascular center as quickly as possible. Patients without life-threatening conditions should, if possible, be transported to a center providing highly specialized medical care. This is due to the need to conduct contrast studies of the cerebral bed to determine the causes of stroke, as well as a significant number of patients who may require surgical assistance.
Inpatient care
Resuscitation/Intensive Care Ward
Patients in the most acute period of HI have a very high risk of rapid development of complications. Therefore, it is recommended that patients be placed in a neurocritical care unit, emergency department, or vascular intensive care unit. Carrying out basic therapy for patients with HI corresponds to the general principles of treating patients with any type of stroke.
Correction of respiratory disorders
Patients should be monitored by pulse oximetry. Blood oxygen saturation should be at least 95%.
If hypoxia is detected, oxygen therapy should be established: 2–4 liters of oxygen through nasal cannulas.
Patients with tachypnea more than 32 or less than 12 per minute, severe hypoxemia (pO2 < 60 mm Hg in arterial blood) or hypercapnia (pCO2 > 50 mm Hg in arterial blood in the absence of COPD), with a decrease in the level Consciousness less than 9 points on the Glasgow Coma Scale requires tracheal intubation and artificial ventilation to ensure normal blood gas composition (Table 1).
Table 1. Normal blood gas parameters
| Parameter | Norm |
| paO2 | 75 – 100 mm. rt. Art. |
| paCO2 | 35 – 45 mm. rt. Art. |
| pvО2 | 38 – 42 mm. rt. Art. |
| saO2 | 95 – 100% |
Blood pressure control
No controlled studies have determined optimal blood pressure levels in patients with acute hemorrhagic stroke. There are several conflicting opinions regarding the correction of arterial hypertension in patients with ICH. A marked increase in blood pressure can worsen the course of ICH by increasing bleeding, leading to an increase in hematoma size and worsening the prognosis, so lowering blood pressure may improve the outcome. However, increased blood pressure may be beneficial in terms of maintaining cerebral perfusion in some patients with ICH, and a decrease in blood pressure may cause ischemia, thereby provoking worsening neurological deficits. Although earlier studies have shown that lowering blood pressure in patients with acute ICH slows hematoma growth, larger controlled studies have not shown a benefit of aggressive blood pressure lowering in most clinical settings.
Below are the 2015 American Heart Association/Ischemic Stroke Association recommendations for the diagnosis and treatment of spontaneous ICH. Patients with ICH and systolic arterial hypertension levels from 150 to 220 mmHg. Art. in the absence of contraindications to antihypertensive therapy, aggressive reduction of SBP to 140 mmHg. Art. is safe (Class I, Level of Evidence A) and effective in improving functional outcomes (Class IIa, Level of Evidence B). Patients with ICH and systolic arterial hypertension > 220 mm Hg. Art. Aggressive BP lowering through continuous intravenous infusion of antihypertensive agents and frequent BP monitoring may be appropriate (Class IIb, Level of Evidence C).
According to the recommendations for the treatment of arterial hypertension, adopted in August 2021 at the Congress of the European Society of Cardiology in Munich, immediate reduction of blood pressure is not recommended for patients with acute intracerebral hemorrhage with systolic arterial hypertension <220 mm. rt. Art. (Class III, Level of Evidence A). Patients with ICH and systolic arterial hypertension ≥220 mm. rt. Art. It is advisable to carefully lower blood pressure through intravenous antihypertensive therapy with the goal of reducing it to <180 mm. rt. Art. (Class IIa, Level of Evidence B).
Thus, the optimal target blood pressure for HI has not been established, but a SBP level of 140 - 160 mm Hg is considered acceptable. Art. Of the drugs available in Russia to control blood pressure, the use of enalapril is recommended. Beta blockers and calcium antagonists are used abroad. The choice of drug should take into account the speed of onset and duration of effect, route of administration (bolus or infusion), concomitant diseases, potential adverse events and experience in a particular institution.
Control of intracranial pressure
Increased intracranial pressure (ICP) with ICH is a consequence of hematoma pressure or mass effect due to surrounding edema. Hydrocephalus developing with ICH may be an additional factor in increased ICP and brain damage, which lead to worsening neurological deficits. Basic measures should be carried out for all patients with ICH.
Indications for monitoring ICP and the effectiveness of treatment (cerebrospinal fluid drainage and osmotic therapy) are presented below.
Basic therapy
- Raise the head of the bed by 30 degrees.
- Light sedation to ensure patient comfort.
- If possible, avoid endotracheal tube retainers or fixation devices that may compress the jugular veins.
- Using saline to compensate for fluid deficiency and refusing to administer hypotonic solutions.
In most cases, there are contraindications for the administration of corticosteroids to reduce ICP. Corticosteroids are not recommended for cerebral edema in patients with HI, due to their low effectiveness and high risk of developing infectious complications.
ICP monitoring
Invasive ICP monitoring is advisable for patients with a Glasgow Coma Scale (GCS) score of <8, with clinical signs of transtentorial herniation, signs of significant intraventricular hemorrhage, or hydrocephalus. Direct ICP measurement allows targeted treatment to maintain cerebral perfusion pressure (CPP) between 50 and 70 mmHg. Art. However, convincing evidence indicating that monitoring ICP or reducing elevated ICP improves the outcome of patients with ICH is currently lacking. Ventricular drainage of cerebrospinal fluid helps reduce elevated ICP. Its implementation is advisable for patients with occlusive hydrocephalus, especially when combined with depression of consciousness. Occlusive hydrocephalus is a common complication of hemorrhages in the thalamic region with compression of the third ventricle and hemorrhages in the cerebellum with compression of the fourth ventricle. In the latter case, surgical drainage of the hematoma is preferable to ventricular drainage. In the case of a combination of intraventricular hemorrhage with hydrocephalus, ventriculostomy is also often used.
Osmotic therapy
Increased ICP or life-threatening mass effect can be treated with hypertonic sodium chloride solution or mannitol.
Intravenous mannitol rapidly and effectively reduces ICP. Drug administration regimens differ in different institutions and regions. It is advisable to administer a bolus of 0.5–1 g/kg. Higher doses are used for health reasons due to mass effect and/or signs of herniation. After this, repeated infusions are carried out at a dose of 0.25 - 0.5 g / kg every 4-12 hours under the control of blood osmolarity. Treatment is carried out to achieve plasma hyperosmolarity (300 - 310 mOsmol/kg) to eliminate excess accumulation of water in the brain tissue. The plasma osmolar gap should not exceed 55 mOsmol/kg, and the dose of mannitol should not exceed 250 mg/kg every 4 hours. A higher dose may cause reversible renal failure. To prevent renal failure, it is necessary to avoid severe hyperosmolarity.
Hypertonic sodium chloride solution is an effective hyperosmolar agent for controlling elevated ICP. The drug can be used in a wide range of concentrations: from 3%, which is most often used for continuous infusion (it can also be used for bolus administration), to 23.4%, which is usually used for bolus administration. The use of a continuous infusion of 3% NaCl can be titrated to a sodium target of 145–155 mEq/L. Potential adverse effects include circulatory overload or pulmonary edema, as well as increased chloride ions, which can lead to normal anion gap metabolic acidosis (hyperchloremic acidosis).
"Therapy of Despair"
Placing a patient in a medically induced coma is advisable only if cerebrospinal fluid drainage and osmotic therapy are ineffective. Medically induced coma reduces cerebral blood flow and lowers ICP.
Barbiturate coma
Depression of consciousness is most often achieved by administering phenobarbital. This therapy may be associated with a high incidence of adverse events, especially the development of arterial hypotension. When administering high doses of barbiturates, it is advisable to conduct EEG monitoring. The dose is titrated until a burst-suppression pattern appears.
Propofol
Propofol reduces intracranial pressure, is easily titrated and has a short half-life. Propofol is given intravenously to mechanically ventilated patients with a loading dose of 1 to 3 mg/kg and continued as an infusion titrated to the desired level, usually 5 to 50 mg/kg per minute with a maximum dose of 200 mg/kg per minute. Hypotension is a common adverse effect of propofol infusion. Treatment includes intravenous hydration and/or infusion of vasopressors to maintain cerebral perfusion pressure. Propofol infusion syndrome is a rare complication that occurs when the drug is administered in high doses (>4 mg/kg per hour >67 mcg/kg per minute) and for a long duration (>48 hours), however, it has also been noted with short-term introductions. It is characterized by acute treatment-refractory bradycardia, metabolic acidosis, collapse, rhabdomyolysis, hyperlipidemia, renal failure, and hepatomegaly.
Hyperventilation
Hyperventilation causes a rapid decrease in ICP, causing cerebral vasoconstriction. Target PaCO2 value >30 - 35 mm Hg. Art. More aggressive hyperventilation (PaCO2 26–30 mmHg) may lead to cerebral ischemia, which worsens outcome. However, the effect of hyperventilation on ICP lasts several minutes. Thus, the use of hyperventilation remains a reserve therapy in cases where other treatment has been completed in full. This treatment method can be used as emergency treatment for patients with signs of brain herniation, before using more reliable methods of treatment.
Therapy with muscle relaxants
Muscle relaxant therapy is sometimes used to reduce ICP in patients who do not respond to analgesia and sedation, since muscle activity can increase ICP by increasing intrathoracic pressure, which reduces venous blood flow from the brain. A disadvantage of muscle relaxant therapy is the increased risk of pneumonia and sepsis. In addition, assessing the neurological status of an immobilized patient becomes impossible.
Correction of risk factors
Variable pneumocompression of the lower extremities is the main method of preventing thromboembolism in patients with acute ICH and should be carried out from the first day of admission to the hospital.
To compensate for fluid deficiency, it is recommended to use saline solution. Hypotonic solutions are contraindicated because they can increase the severity of cerebral edema and intracranial pressure. It is necessary to avoid hypervolemia for the same reasons. Control of water and electrolyte balance is achieved by maintaining normal blood plasma sodium levels (130–150 mmol/l; osmolality (280–295 mOsm/kg H2O), as well as daily diuresis of 1500 ml±500 ml/day. It is advisable to maintain normovolemia. Daily norm The patient's hydration is 30–35 ml per kg of body weight. In case of increased ICP, a slight negative water balance can be allowed (300–500 ml/day).
Hyperthermia above 38.0°C requires antipyretic therapy. It is necessary to eliminate the causes of hyperthermia. Prophylactic antibiotics do not improve clinical outcome.
Dysphagia is a common and important risk factor for the development of aspiration pneumonia. Diagnosis of dysphagia should be carried out in all patients before switching to oral nutrition to reduce the risk of developing pneumonia. Enteral nutrition is preferable to parenteral nutrition, as it is more physiological and is associated with a lower risk of developing malnutrition and infectious complications. The average energy requirement is approximately 30 kcal/kg per day (average 1800–2400 kcal per day).
Hyperglycemia after hyperglycemia is associated with adverse outcomes. It is prudent to avoid both hyperglycemia (>10 mmol/L) and hypoglycemia (<3.3 mmol/L).
It is advisable to conduct systematic screening of myocardial infarction after ICH using ECG and determination of cardiac-specific enzymes.
There is insufficient data to limit the use of statins in patients with ICH.
To prevent cerebral vasospasm, all patients who have suffered subarachnoid hemorrhage are prescribed nimodipine orally 60 mg every 4 hours for 3 weeks to prevent secondary ischemic brain damage, i.e. 2 x 6 times a day (360 mg/ days).
Surgery
The tactics of surgical treatment of patients with HI are outlined in accordance with clinical recommendations approved at the XXXVIII Plenum of the Board of the Association of Neurosurgeons of Russia.
Detection of spontaneous VMH during clinical neuroimaging examination is an indication for mandatory consultation with a neurosurgeon within the next few hours after diagnosis. Surgical treatment is aimed at eliminating compression and dislocation of the brain, as well as occlusive hydrocephalus, which leads to a significant decrease in mortality, and in some patients in whom conservative treatment is ineffective, to a decrease in neurological deficit already in the acute period of the disease.
Principles for selecting patients for surgical treatment
1. Indications for surgical treatment for HI are:
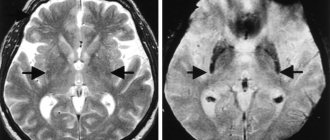
- lateral/putamental and subcortical/lobar hemorrhage with a volume of more than 30 cm3, accompanied by severe neurological deficits and/or leading to brain dislocation (displacement of the median structures of more than 5 mm or deformation of the brain stem cisterns);
- hemorrhage in the cerebellum with a volume of more than 10–15 cm3, with a diameter of more than 3 cm, accompanied by compression of the brain stem and/or occlusive hydrocephalus; it is not recommended to perform external ventricular drainage without removing the cerebellar hematoma due to a possible increase in axial dislocation of the brain;
- hemorrhage in the cerebellum with a volume of less than 10–15 cm3, accompanied by hemotamponade of the fourth ventricle and occlusive hydrocephalus;
- hemorrhage into the thalamus, accompanied by ventricular hemotamponade and/or occlusive hydrocephalus.
2. Surgical intervention is not indicated when consciousness is depressed to the point of coma (Glasgow Coma Scale score 7 or less).
3. A relative contraindication to surgery is the presence of severe somatic pathology (diabetes mellitus, renal - hepatic, cardiovascular and pulmonary pathology in the sub- and decompensation stage, coagulopathy, sepsis), uncontrolled arterial hypertension - systolic pressure more than 200 mm. rt. Art.
Risk factors for unfavorable outcome during surgical treatment are:
- decreased wakefulness to stupor and below;
- the volume of intracerebral hematoma is more than 50 cm3;
- massive ventricular hemorrhage;
- transverse dislocation 10 mm or more;
- deformation of the brainstem cisterns;
- recurrence of hemorrhage.
The advisability of surgical removal of hypertensive hematomas of the thalamus with a volume of more than 10 cm3 and the brain stem, accompanied by severe neurological deficits, is being discussed, and there is currently no established opinion on this matter among neurosurgeons.
Selection of surgical treatment method
Surgical intervention is carried out after examining the patient and determining the type of hematoma (see section 3, GI classification). In case of severe arterial hypertension (systolic blood pressure more than 200 mm Hg), in order to prevent perioperative complications (intraoperative hemostasis, high risk of postoperative relapse of ICH), it is advisable to postpone surgery until blood pressure stabilizes. In a number of observations, during the first 24 hours, ICH may continue to form and recur, so some neurosurgeons suggest not performing surgery within 6–24 hours from the onset of the disease.
Performing puncture aspiration of the IMH using the stereotaxic method (frameless navigation station) is indicated for lateral and cerebellar hematomas in patients without quantitative disorders of consciousness or with a decrease in consciousness no deeper than stunning. The intervention can be combined with local fibrinolysis of blood clots. Neuroendoscopy can be used to remove the hematoma. For fibrinolysis, 5000–6000 IU of urokinase, 50–100 thousand IU of recombinant prourokinase, 3 mg of tissue plasminogen activator, 15–30 thousand IU of streptokinase are used for a single injection. The administration of fibrinolytic and aspiration of lysed blood is carried out every 6 to 12 hours, depending on the type of drug. The optimal time for hematoma drainage without increasing the risk of infectious complications associated with the presence of drainage and intrathecal administration of the drug is 24–72 hours.
Open operations are indicated for subcortical/lobar hematomas, as well as for lateral/putamenal hemorrhages and cerebellar hematomas with a clinical picture of rapid growth of dislocation syndrome. In case of subcortical/lobar hemorrhages, microsurgical revision of the hematoma cavity is necessary to remove a possible angiographically negative malformation, the incidence of which can reach 30%. For lateral/putamenal and cerebellar hemorrhage, open surgery aims to quickly create external decompression of the brain and prevent or eliminate compression and dislocation of the brain.
In the presence of severe somatic pathology, it is possible to remove subcortical hematomas using one of the minimally invasive methods (using stereotaxis, endoscopy, local fibrinolysis), but only after cerebral angiography and exclusion of vascular malformation.
For small cerebellar hematomas, accompanied by displacement and/or occlusion of the fourth ventricle or aqueduct of Sylvius and the development of occlusive hydrocephalus, external ventricular drainage or endoscopic triventriculostomy is indicated. External drainage is carried out until regression of occlusive hydrocephalus and restoration of patency of the ventricular system.
In case of massive hemorrhage in the lateral ventricles, it is possible to drain them externally with local fibrinolysis of blood clots or their endoscopic removal.
In the severe condition of the patient (reduced wakefulness to deep stupor and stupor, severe somatic pathology), which may require long-term intensive care in the postoperative period, intervention on the hematoma must be supplemented with the installation of a sensor for measuring intracranial pressure.
Postoperative period
After the operation, the patient must remain in the neurointensive care unit. Within 1–2 days after open surgery, a control CT scan of the brain is necessary. Subsequently, if there is no deterioration in the condition, the study is repeated on days 7 and 21. When carrying out local fibrinolysis, CT scans are performed every 24 hours, after removal of the drainage - on days 7 and 21. Intracranial pressure is monitored until it is stablely normalized (less than 20 mm Hg), then the sensor is removed.