Depression is a common illness, affecting approximately 20% of people in developed countries. Her therapy includes an integrated approach, including the use of medications. The new generation tranquilizer Grandaxin for depression is prescribed in case of moderately severe symptoms. It has a gentle effect on the patient’s psycho-emotional background, while exhibiting a minimum of side effects.
Action of amitriptyline
The main effect of amitriptyline is antidepressant.
It also has a sedative (calming), hypnotic and anti-anxiety effect. It has no effect on a healthy person with a normal psychological state. These effects appear only in the presence of depression, restlessness, anxiety and insomnia, respectively. In addition to the effects of amitriptyline, there are other effects:
- Anesthetic.
- Vegetative stabilizing.
- Antidiarrheal (fixing).
- Removes psychosomatic symptoms: skin rash, high blood pressure, restores appetite, etc.
- Effective for some forms of enuresis (bedwetting).
Treatment and prevention of neuroses
The cause of neuroses is psychological tension, which arises under the influence of stress and gives rise to internal conflict. In other words, a neurotic disorder is a distorted way of adapting the psyche to unbearable circumstances.
A neurotic disorder does not change personality and does not take away a person’s ability to think critically about their condition - this distinguishes neuroses from psychoses, when changes in the psyche are deeper and more persistent. Therefore, treatment of neuroses is usually successful and should result in complete recovery, provided that all the necessary conditions are met.
How do neuroses manifest themselves?
What comes to the fore in a state of neurosis: emotional instability, difficulties in adapting to rapidly changing circumstances, fear of the slightest changes, self-doubt, the desire to always focus on a certain standard, excessive sensitivity to the mood of others and anxiety when negative emotions of another, obsessive movements hands, frequent weakness and health complaints.
Neurotic disorders are characterized by a combination of anxiety and depression. Phobias, obsessions, panic attacks, headache attacks, hypochondriacal thoughts, disorders of a psychosomatic nature - manifest themselves depending on the type of neurosis.
Neurotic symptoms are a way to somehow stabilize the situation, to bring something permanent into your life against the backdrop of the factor that caused the neurosis. Psychologists and psychiatrists note that even without treatment, a neurotic disorder can go away if the trigger factor has been eliminated.
Treatment of neurotic disorders
The main method of treating neurosis is psychotherapy. Deep techniques are often used for this, but rational psychotherapy is increasingly used. The choice of method depends on the clinical picture observed by the psychotherapist. In some cases, immersion in the internal causes of neurosis can only harm the patient, so it is not always necessary to look for a psychoanalyst or Gestalt therapist as a doctor.
Physiotherapy is a method that helps you move from stressful thoughts to feeling your body. Often, the effects of relaxing and restorative massage techniques, swimming, electrical impulse therapy, and gymnastics help to normalize the psychological sphere and get rid of neurosis.
Drugs for the treatment of neurotic disorders are also selected based on the symptoms observed by the doctor. Tranquilizers and antidepressants are used only when other treatment methods have no effect without them, and are discontinued whenever possible when a lasting effect from treatment is obtained.
Sedatives and nootropics are used during the entire course of therapy, depending on the clinical picture. Glycine , a drug created by microencapsulation of the amino acid of the same name, is prescribed as a permanent drug for the complex treatment of neuroses The use of Glycine allows you to gradually restore the protective capabilities of the nervous system from the inside, increasing resistance to neurotic disorders.
Prevention of neurosis
Stress is an integral part of life, and neurotic disorder can be caused by any of them. By correctly experiencing stress, you help the nervous system cope with the load and avoid fixing the problem in the form of neurosis
- If you are experiencing negative emotions, it is important to give them an outlet. Playing sports, in particular martial arts, helps a lot with this. But any socially acceptable way to relieve stress will be helpful. Just don't relieve stress with alcohol
- Rest, sleep as much as you need to recover. Don't work too hard and take your vacation on time. Simple methods of protecting yourself from overload help you stay healthy
- Resolve conflicts as they arise, do not hide emotions for the greater good. This approach to maintaining peace will not be useful to either side.
- Take Glycine to prevent neuroses. The amino acid glycine improves energy production in the nervous system and protects it from overload. The drug is safe for children and adults, recommended for stress.
Indications for use
As doctors and scientists accumulate experience in the use of amitriptyline and clarify the mechanisms of development of many diseases, the indications for its use are constantly expanding. Main indications:
- Endogenous depression.
- Depressive psychosis.
- Anxiety disorders: generalized anxiety disorder, panic disorder, phobias, obsessive-compulsive disorder.
- Organic anxiety and depression.
- Schizotypal disorder, schizophrenia with depressive symptoms.
- Addictions (alcohol, drug, polydrug addiction).
- Neuroses.
- Personality disorders (psychopathy).
- Somatoform and psychosomatic diseases.
- Eating disorders.
- Pain syndrome.
- Enuresis.
Content:
- Interaction of antidepressants with amphetamines
- Serotonin syndrome
- Help with serotonin syndrome
Amphetamine and antidepressants are mixed to enhance the euphoric effect, to reduce the dose of the drug and increase its duration of action. But when these substances are combined, their influence decreases and it seems to the person that the amphetamine taken works poorly. He begins to increase the amount of the substance to achieve the desired effect, risking an overdose or a host of other life-threatening complications.
Interaction of antidepressants with amphetamines
Tricyclic antidepressants are used to treat persistent depression that is not treatable with new generation drugs. They are effective for melancholic depression, but have many side effects. This limits their use in everyday practice. The mechanism of action is to block serotonin and epinephrine transporters, which causes an increase in the concentration of neurotransmitters, and improves the patient’s condition, reduces melancholy and apathy.
Amphetamines are psychostimulants that enhance the release of serotonin, dopamine, and norepinephrine into the synaptic cleft. An increased concentration of these substances causes euphoria, increased performance and focus, reduces the need for sleep, rest and food, and accelerates thought processes. Their uncontrolled use leads to complete exhaustion of the body and early death.
The combination of amphetamine and antidepressants produces unpredictable results. There may be an option when cross-reaction does not occur, and all the standard properties of these substances are preserved. Or vice versa, it will lead to an increase in anxiety and the formation of psychosis. In case of severe exhaustion, this mixture of drugs will take away the last of your strength.
Antidepressants, like psychostimulants, release large amounts of serotonin, and when they are mixed, all positive and negative effects are increased. The combined use of Amitriptyline or another tricyclic antidepressant with amphetamine can lead to the development of serotonin syndrome or cause the following complications:
- shock;
- severe form of hypertension;
- stroke;
- tachycardia and arrhythmia;
- panic attacks;
- cerebrovascular accident;
- hyperthermia;
- narrowing of most blood vessels;
- coma;
- suicidal thoughts.
In the most severe cases, death can occur.
For anxiety-anesthetic depression, antidepressants with sedative and anxiolytic effects are used: tricyclic (amitriptyline 150-250 mg/day, clomipramine (Anafranil) 150-250 mg/day, trimipramine (Gerfonal) 100-150 mg/day), serotonergic (sertraline ( Zoloft) 50-300 mg/day and fluvoxamine (fevarin) 100-300 mg/day) and tetracyclics (maprotiline (ludiomil) 250-300 mg/day).
Tranquilizers are prescribed as adjuncts and for anxiolytic purposes as part of combination therapy: phenazepam 3-6 mg/day, diazepam (Seduxen, Relanium) 10-30 mg/day, lorazepam (Merlit) 2-6 mg/day, alprazolam (Xanax , cassadan) 2-4 mg/day and antipsychotics: alimemazine (Teralen) 30-45 mg/day, thioridazine (sonapax) 30-40 mg/day, chlorprothixene 100-150 mg/day, clozapine (leponex, azaleptin) 50 -100 mg/day.
For melancholy-anesthetic depression, antidepressants with a powerful thymoanaleptic effect are used, as well as drugs with a “balanced” effect. Tricyclic antidepressants are used: imipramine (melipramine) 150-250 mg/day, clomipramine (anafranil) 150-250 mg/day; serotonergic agents: fluoxetine (Prozac, Portal) 20-80 mg/day and sertraline (Zoloft) 50-300 mg/day, as well as maprotiline (ludiomil) 250-300 mg/day. Antidepressants are combined if necessary, and the doses of tricyclics when combined with serotonergic drugs are reduced by half compared to the above. If the described remedies are ineffective in some patients, the use of a reversible monoamine oxidase inhibitor, moclobemide (Aurorix), in the maximum daily dose (600 mg/day) is successful.
It is usually necessary to add antipsychotics with a stimulating effect: trifluoperazine (stelazine, triftazine) 5-10 mg/day, sulpiride (eglonil) 100-400 mg/day, etaprazine 4-8 mg/day.
It should be noted that anxiety- and melancholy-anesthetic depressions do not show significant resistance to therapy in most cases. If resistance is detected, then intravenous drip administration of antidepressants (amitriptyline, imipramine, clomipramine, maprotiline) is effective, increasing the dose to a maximum of 125-150 mg/day in combination with the above listed tranquilizers and antipsychotics. Typically, a course of intravenous drip infusions for 15-20 days brings success. If there is no effect, it is necessary to immediately discontinue therapy as suggested by G.Ya. Avrutsky method. In some patients, the effect of treatment may be incomplete: depression from melancholy or anxiety-anesthetic goes into purely anesthetic, which, however, is subjectively less severe for patients (for the treatment of purely anesthetic depression, see below). At the same time, patients become able to work and consider the transition to purely anesthetic depression as a “positive” dynamics of their condition.
The general sequence of therapeutic measures for anxiety- and melancholy-anesthetic depression is as follows: oral therapy with one antidepressant in combination with a tranquilizer and (or) an antipsychotic (2-3 weeks)! combining two antidepressants orally or prescribing moclobemide (2-3 weeks)! intravenous drip administration of an antidepressant (2-3 weeks)! immediate withdrawal of therapy. It should be noted that in some patients, serotonergic drugs and moclobemide are more effective than powerful tricyclic antidepressants.
During treatment with antidepressants and, especially, after immediate discontinuation of therapy, an inversion of affect with the development of mania (hypomania) may occur, therefore, to prevent the latter and increase the effectiveness of therapy, it is recommended to prescribe normotimic drugs: lithium salts and carbamazepine.
Pure anesthetic depressions , in contrast to anxiety- and melancholy-anesthetic depressions, in the vast majority of cases show pronounced resistance to therapy, which allows only to slightly reduce the intensity of anesthetic disorders during treatment, but not to stop the symptoms completely. This condition is prone to a protracted, multi-year course and often develops as part of the schizophrenic process. If purely anesthetic depression is detected, high doses of tricyclic antidepressants (imipramine, clomipramine 300-350 mg/day) should be immediately prescribed or intravenous drip administration of these drugs should be immediately started, reaching maximum dosages (125-150 mg/day). S.N. Mosolov (1995) recommends in such cases the tactics of “rapid thymoanalepsy”: anafranil is administered intravenously, starting from 25-50 mg/day with a daily dose increase of 25-50 mg (i.e. by 1-2 ampoules) with quickly reaching the maximum daily level of 150 mg. To enhance the effect, 25-75 mg (1-3 ampoules) of maprotiline (ludiomil) are sometimes added to the infusion system. After 15-20 days, if there is no effect, it is recommended to immediately discontinue therapy, against the background of which in some patients it is possible to achieve a decrease in the severity of anesthetic disorders. Sometimes it is necessary to resume therapy and another 2-3 withdrawal sessions.
In patients with purely anesthetic depression, antidepressants must be combined with neuroleptics with stimulating and anti-negative effects (trifluoperazine 5-10 mg/day, etaprazine 4-8 mg/day, sulpiride 100-400 mg/day).
The experience of using electroconvulsive therapy for anesthetic depression is contradictory (both the effectiveness and complete ineffectiveness of this type of treatment and even worsening of the condition after it are described), so it is not possible to clearly recommend this technique for resistant anesthetic depression.
It should be added that when anesthetic depression occurs against the background of a pronounced progression of the schizophrenic process or in the presence of delusional disorders in the structure of depression, it is mandatory to prescribe powerful antipsychotics in medium doses (trifluoperazine 10-30 mg/day, clozapine 100-150 mg/day), regardless from a psychopathological type of depression.
Help with serotonin syndrome
The first thing to do is stop taking the medications. With a mild form of the disease, the manifestations will disappear on their own within 24 hours. Prescription of benzodiazepines helps reduce symptoms. The moderate and severe stages are treated in intensive care under the control of all body functions and with the use of intensive therapy. Serotonin blockers may be prescribed.
By mixing tricyclic antidepressants and amphetamine, drug addicts often overdose, which leads to death. Providing emergency assistance can be difficult, since it is not known what mixture of substances he consumed. By turning to a drug center for help and completing the entire course of treatment for addiction, a person will be able to avoid dangerous consequences and return to normal life.
Serotonin syndrome
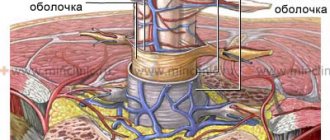
This rare condition occurs when there is an unsuccessful combination of drugs that affect serotonin metabolism. Abuse of them in large quantities leads to the accumulation of the neurotransmitter in the central nervous system. In the first place among such substances are tricyclic antidepressants and amphetamine. The risk of serotonin syndrome depends on the dose of the drug taken. In this case, characteristic symptoms develop:
- increase in temperature - in severe cases;
- increase in blood pressure;
- disturbance of consciousness;
- hallucinations;
- delirium;
- psychomotor agitation;
- inappropriate behavior;
- mutism;
- stomach ache;
- drooling and lacrimation;
- increased sweating;
- chills;
- involuntary movements of the eyeballs;
- crawling sensations;
- speech disorders;
- tremor;
- spasm of the chewing muscles;
- imbalance of all biological functions.
Symptoms increase rapidly and develop within 6 hours. This is an acute condition that requires emergency medical attention. Serotonin syndrome has various symptoms, and some may have no symptoms. The manifestation of disorders of only one type is likely (disorders of the autonomic system, mental or neuromuscular). In some cases, the syndrome progresses rapidly and ends in death.
There are three degrees of flow:
- Mild - occurs when using the drug in the usual dosage.
- Moderate - when the amount of one of the mixed serotonergic substances is exceeded.
- Severe - when large doses of amphetamine and antidepressant interact.
The majority of patients are cured within 7 days. In mild forms, resolution occurs after stopping the drug after 24-72 hours. In patients with a severe course, muscle pain and weakness may persist for several months.
The third form of serotonin syndrome leads to the development of life-threatening complications:
- progressive neuromuscular diseases;
- renal, liver and respiratory failure with extensive inflammation in the lungs;
- hyperkalemia,
- severe metabolic acidosis,
- circulatory disorders;
- stroke;
- leukopenia and thrombocytopenia;
- tonic-clonic seizures;
- asphyxia due to myoclonus of the pectoral muscles.
The risk of serotonin syndrome depends on the dose of the drug taken. The diagnosis is made only according to clinical data and the presence of three of the listed signs in the patient: agitation, disorientation, hypomania, myoclonus, chills, tremor, increased reflexes, motor disorders, diarrhea, fever. In addition, prior dosage increases or mixing of the antidepressant with other substances should be known.
Literature:
- Molecular mechanisms of drug interaction / [M. A. Paltsev et al.]; edited by Paltseva M. A., Kukesa V. G., Fisenko V. P.; Moscow honey. acad. them. I. M. Sechenov. - M.: AstraPharmServis, 2004 (ChPK OJSC). — 224 p.
- Adverse drug reactions = Adverse drug reactions. General information / Reichart D.V. et al.; edited by D. W. Reichart. - Moscow: Litterra, 2007. - 248 p.
- Secrets of toxicology / Louis J. Ling [et al.]; lane from English under general ed. E.A. Luzhnikov. - M.; St. Petersburg : Binom, 2006 (SUE IPK Ulyan. House of Printing). — 376 p.