Zoloft - what kind of drug is it? The active ingredient of the drug is sertraline. It belongs to the pharmacological group of antidepressants and is prescribed to patients with the following symptoms: depression, OCD, panic disorder, PTSD, social phobia. Zoloft is a powerful serotonin reuptake inhibitor in human brain cells.
More than 1/3 of people experience dangerous consequences from abrupt Zoloft withdrawal. In narcology, this phenomenon is called withdrawal syndrome or withdrawal syndrome. The time for withdrawal symptoms to occur when used is directly proportional to the half-life of the drug from the body. A drug such as Zoloft is addictive if used systematically, irregularly, so there is also Zoloft withdrawal syndrome, which usually occurs 3-5 days after the last use of the drug. Zoloft withdrawal symptoms are quite difficult to recognize, so people think that the disease has returned and start using the medicine again.
- You can't convince me to get treatment
? - We will help you with motivation for treatment. As a rule, it is difficult for loved ones to persuade or force an addict to undergo treatment. World experts have developed EFFECTIVE motivation schemes, using which you can lead an addict to the decision to seek help. 8
Pharmacological properties of the drug Zoloft
Pharmacodynamics. Sertraline is a potent and nonspecific inhibitor of serotonin (5-HT) reuptake in neurons. Very little effect on the reuptake of norepinephrine and dopamine. At therapeutic doses, sertraline blocks the uptake of serotonin into human platelets. It does not have a stimulating, sedative or anticholinergic effect, and also does not exhibit a cardiotoxic effect in the experiment. In controlled trials in healthy volunteers, sertraline did not cause sedation or affect psychomotor performance. Consistent with its selectivity for (5-HT) reuptake inhibition, sertraline does not stimulate catecholaminergic activity. Sertraline does not show affinity for muscarinic, serotonergic, dopaminergic, adrenergic, histaminergic, GABAergic and benzodiazepine receptors. Long-term use of sertraline in animals led to a decrease in the activity of brain adrenergic receptors; Other antidepressants and anti-obsessive drugs exhibit a similar effect. Sertraline does not cause drug dependence; does not have the stimulant and anxiety effects of d-amphetamine or the sedation and psychomotor effects of alprazolam. Pharmacokinetics. In the dose range of 50–200 mg, the pharmacokinetics of sertraline are dose dependent. When sertraline was administered orally at a dose of 50–200 mg once a day for 14 days, the concentration of the drug in the blood plasma reached its maximum level 4.5–8.4 hours after administration. The pharmacokinetic profile in adolescents and the elderly does not differ significantly from that in adult patients aged 18–65 years. The half-life of sertraline in young and old men and women is 22–36 hours. In accordance with the terminal half-life, a double cumulation is observed upon reaching an equilibrium concentration, which is achieved after 1 week of treatment (use once a day). Plasma protein binding is 98%. Animal studies have demonstrated a large apparent volume of distribution for sertraline. The pharmacokinetics of sertraline in children with obsessive-compulsive disorder (OCD) are the same as in adults (although sertraline is metabolized somewhat more rapidly in children). However, it may be appropriate to use it at lower doses in children, given their lower body weight and the need to prevent excessive plasma concentrations. Sertraline undergoes biotransformation during its initial passage through the liver. Its major plasma metabolite is Ν-desmethylsertraline, which has much lower activity (approximately 20-fold) than sertraline in vitro in vivo models of depression . The half-life of N-desmethylsertraline is 62–104 hours. Sertraline and N-desmethylsertraline undergo intensive biotransformation in the human body, and the final metabolites are excreted in feces and urine in equivalent amounts. Only a small portion of sertraline (≤0.2%) is excreted unchanged in the urine. Concomitant food intake does not significantly affect the bioavailability of sertraline.
Composition and form of the product
The active ingredient in the product is sertraline hydrochloride. The component has a powerful antidepressant effect, but does not have a sedative effect, and also does not have anticholinergic or stimulating properties.
Zoloft is produced in tablet form. One biconvex film-coated tablet contains 50 mg or 100 mg of active substance. Distinctive features of the tablets are their oval shape, white color, and the presence of “Pfizer” and “ZLT-50” engravings on different sides.
Other ingradienites are also used to produce the medicine. Their list is indicated in the instructions for use.
Indications for use of the drug Zoloft
Depression (including accompanied by anxiety) with or without a history of mania. OCD in adults and children. Panic disorders, with or without agoraphobia. Post-traumatic stress disorder (PTSD). Social phobia (social anxiety disorder). If the treatment outcome is satisfactory, continuation of sertraline therapy is an effective means of preventing recurrence of the initial episode of depression and its development in the future; relapse of an initial episode of OCD; panic disorder, initial episode of PTSD, social phobia.
Use of the drug Zoloft
Orally 1 time per day in the morning or evening, regardless of meals. Beginning of treatment For depression and OCD : treatment should begin with a dose of 50 mg/day. Panic disorders, PTSD and social phobia : start with a dose of 25 mg/day, after 1 week the dose of the drug is increased to 50 mg/day. This dosage regimen reduces the incidence of side effects at the initial stage of treatment of panic disorders. Dose titration Depression, OCD, panic disorder, PTSD : if the effect of the 50 mg dose is insufficient, the dose can be increased. Dose adjustment should begin no earlier than after 1 week of treatment, titration dose - 50 mg per week. The dose should not exceed 200 mg/day. Dose adjustments should be made no more than once a week, taking into account the half-life of sertraline, which is 24 hours. The first manifestations of the clinical effect are observed within 7 days of treatment. However, a longer period is required for its full development, especially in OCD. Maintenance dose When carrying out long-term treatment, the dose should be minimally effective; it is subsequently adjusted depending on the response to treatment (therapeutic effect). Use in children The safety and effectiveness of sertraline have been established for children and adolescents with OCD aged 13–18 years. There is no experience with the use of sertraline in children under 6 years of age, as well as in other pathologies. When using sertraline in children with OCD (age 13–18 years), a dose of 50 mg/day should be used. If there is no effect when taking the drug at a dose of 50 mg/day, if necessary, it may be further increased to 200 mg/day. In clinical trials in children aged 13 to 18 years with depression or OCD, the pharmacokinetic profile of sertraline was similar to that in adults. However, in pediatrics, when increasing the dose of 50 mg, the lower body weight in children compared to adults should be taken into account. Dose titration in children The half-life of sertraline is about 24 hours. Dose adjustments should not be made more than once a week. Use in elderly people In elderly people (over 65 years of age), the drug is used in the same doses as in younger people (up to 65 years of age). Side effects and their frequency were the same as in younger patients. Use in patients with liver failure In patients with liver disease, sertraline is used with caution. In patients with liver failure, the dose or frequency of administration should be reduced. Use in patients with renal failure Sertraline is intensively metabolized in the body, so a small amount of the drug is excreted unchanged in the urine. Due to the insignificant renal excretion of sertraline, there is no need to change the dose of the latter in patients with renal failure.
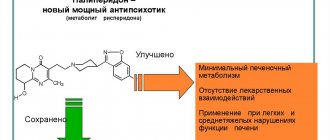
Zoloft and antipsychotics
Zoloft and antipsychotics are prescribed only by the attending physician if monotherapy with an antidepressant is not effective. Such polytherapy is used in the following cases:
- For anxiety-anesthetic depression to provide a sedative effect and enhance the anxiolytic effect of the antidepressant.
- In case of melancholy-anesthetic depression, Zoloft has a serotonergic effect, which can be enhanced by adding antipsychotics with a stimulating effect. If treatment with oral forms of drugs is not effective, intravenous administration of antidepressants is possible.
- For purely anesthetic depressions that are highly resistant to antidepressant monotherapy. After making the appropriate diagnosis, the combination of Zoloft with antipsychotics with stimulating and anti-negative effects is mandatory.
The effectiveness of combined treatment with Zoloft and antipsychotics reaches 60-70%. However, when using polytherapy, it should be taken into account that antidepressants reduce the effectiveness of antipsychotics.
Side effects of the drug Zoloft
From the gastrointestinal tract: diarrhea/fecal incontinence, dry mouth, dyspepsia, nausea, abdominal pain, constipation, pancreatitis, vomiting. Metabolic disorders: anorexia; increased appetite, hyponatremia. From the central nervous system and peripheral nervous system: dizziness, drowsiness and tremor, coma, convulsions, headache, hypoesthesia, migraine, movement disorders (including extrapyramidal symptoms, including hyperkinesia, jaw muscle spasms or gait disturbances), involuntary muscle contractures, paresthesia and loss of consciousness. The development of manifestations of serotonergic syndrome, in some cases associated with the use of serotonergic drugs, has also been recorded, namely: agitation, confusion, increased sweating, diarrhea, fever, hypertension (arterial hypertension), rigidity and tachycardia. Mental disorders: insomnia, aggressive reactions, agitation, anxiety, depressive symptoms, euphoria, hallucinations, decreased libido in men and women, nightmares and psychosis. From the reproductive system: sexual dysfunction (primarily delayed ejaculation in men), galactorrhea, gynecomastia, irregular menstrual cycle and priapism. From the skin and subcutaneous tissues: increased sweating, alopecia, angioedema, facial edema, periorbital edema, photosensitivity skin reactions, itching, skin rash (including isolated cases of exfoliative skin lesions - Stevens-Johnson syndrome and epidermal necrolysis), urticaria. From the blood system: leukopenia and thrombocytopenia. From the cardiovascular system: palpitation and tachycardia, pathological bleeding (for example, nosebleeds, gastrointestinal bleeding or hematuria), flushing (sudden redness of the skin) and hypertension (arterial hypertension). From the hearing organs/vestibular system: ringing in the ears. From the endocrine system: hyperprolactinemia, hypothyroidism, hypoaldosteronism syndrome; From the organs of vision: mydriasis and visual impairment. Body as a whole: asthenia, chest pain, peripheral edema, fatigue, fever, malaise. From the hepatobiliary system: severe liver dysfunction (hepatitis, jaundice, liver failure) and asymptomatic increase in the level of transaminases in the blood plasma (ALAT and AST). From the immune system: allergic reactions, anaphylactic reactions. Laboratory indicators: false results of clinical laboratory tests, changes in platelet function, increased cholesterol concentration in the blood serum, increase or decrease in body weight. From the musculoskeletal system: arthralgia and muscle spasms. From the urinary system: urinary incontinence, urinary retention. From the respiratory system: bronchospasm and yawning. The range of side effects most commonly observed in studies of patients with OCD, panic disorder, PTSD, and social phobia were similar to those observed in clinical studies of patients with depression. Other: manifestations of withdrawal syndrome when stopping treatment with sertraline, in particular agitation, anxiety, dizziness, headache, nausea and paresthesia.
Special instructions for the use of Zoloft
MAO inhibitors. Cases of serious side effects, sometimes fatal, have been reported in patients using sertraline in combination with MAO, in particular with the selective MAO inhibitor selegiline and the reversible MAO inhibitor moclobemide. In some cases, serotonergic syndrome developed with the appearance of symptoms such as hyperthermia, rigidity, myoclonus, autonomic dysfunction with the possibility of sudden disturbances in vital functions. Mental disorders in this case are manifested by delirium, irritability and severe agitation, which progresses to a state of delirium and coma. Therefore, sertraline should not be prescribed concomitantly with MAO inhibitors or within 14 days after stopping treatment with this class of drugs. Also, treatment with MAO inhibitors should not be started earlier than 14 days after the end of treatment with sertraline. Other serotonergic agents. The combined use of sertraline and other drugs that stimulate serotonergic neuromediation, in particular tryptophan, fenfluramine or 5-HT agonists, should be carried out with caution and, if possible, excluded (given the risk of pharmacodynamic interaction). Switching from selective serotonin reuptake inhibitors, antidepressants or anti-obsessive drugs. There is limited controlled experience in calculating the optimal timing of switching from selective serotonin reuptake inhibitors, antidepressants or anti-obsessive medications to sertraline. Caution should be exercised when switching from selective serotonin reuptake inhibitors and other antidepressants and anti-obsessive medications, especially long-acting ones (for example, fluoxetine), to sertraline. The duration of the break when switching from treatment with one drug to another has not been established. Increased manic/hypomanic symptoms. During pre-marketing trials of sertraline, increased manic/hypomanic symptoms were observed in approximately 0.4% of patients. Isolated cases of increased mania/hypomania have been described in patients with significantly severe affective disorder who received other antidepressant or antiobsessive drugs. Convulsive seizures. Seizures are a potential complication of therapy with antidepressants or anti-obsessive medications. Seizures were reported in approximately 0.08% of patients treated with sertraline during the depression treatment program. No cases of seizures have been reported during the treatment of panic disorders with sertraline. During treatment with sertraline in 1800 patients with OCD, only 4 of them had seizures (about 0.2%). Three of these patients were children, two had existing seizure pathology, and one had a family history of seizure pathology. However, none of them used anticonvulsants. In all of these cases, a causal relationship with sertraline therapy is unlikely. Since sertraline has not been studied in patients with seizure disorders, it should not be used in patients with uncontrolled epilepsy, and patients with controlled epilepsy should be monitored during treatment. If seizures develop, the drug must be discontinued. Suicides. Patients with depression have a tendency to attempt suicide, which persists until remission occurs. For this reason, patients should be monitored at the beginning of treatment. Given the established fact of increased co-occurrence rates of OCD and depression, panic disorder and depression, and PTSD and depression, similar precautions should be taken when treating patients with OCD, panic disorder, and PTSD. Use for liver failure. Sertraline is actively biotransformed in the liver. According to a multidose pharmacokinetic study, with repeated use of sertraline in patients with compensated mild liver cirrhosis, an increase in the half-life of the drug, an almost 3-fold increase in AUC and an increase in the maximum concentration of the drug in the blood plasma were observed compared with the same values in healthy individuals. There were no significant differences in the level of binding to plasma proteins in patients of these 2 groups. Sertraline should be prescribed with caution to patients with liver disease. If liver function is impaired, it is necessary to reduce the dose and reduce the interval between doses of the drug. Use for renal failure. Sertraline undergoes active biotransformation in the body, so a small part of the drug is excreted unchanged in the urine. In studies of patients with mild and moderate renal failure (drug clearance 30–60 ml/min) and patients with severe renal failure (drug clearance 10–29 ml/min), the main pharmacokinetic parameters of sertraline when taken repeatedly in patients of these groups were not reliably were different. The half-life was the same and no differences in binding to plasma proteins were detected in patients of the study groups. Research data indicate that, given the low rates of sertraline excretion by the kidneys, drug doses may not be adjusted depending on the degree of renal impairment. Children: see APPLICATION section. During pregnancy and breastfeeding. Sertraline can be used during pregnancy and lactation only if the expected benefit to the mother outweighs the likely risk to the fetus and newborn. Women of reproductive age must use effective contraception during treatment. The ability to influence reaction speed when driving vehicles or working with other mechanisms. Clinical and pharmacological studies indicate that sertraline has no effect on psychomotor functions. However, patients should be careful when driving or operating machinery, as the drug may interfere with mental or physical reactions.
How long does Zoloft withdrawal last?
Symptoms of drug withdrawal can persist without drug treatment for quite a long time, for several weeks. While taking antidepressants, the activity of neurons changes, so after stopping the drugs, the body needs time to readjust and adapt to new conditions. The longer the course of treatment, the longer the rehabilitation period will be. Withdrawal symptoms will not disappear until the active substance of the drug is removed from the body. If general weakness lasts for a month, you should consult your doctor or specialists at the Center for Healthy Youth.
When does Zoloft start to work and help?
It is important to understand that the drug Zoloft does not begin to act immediately, but after a certain period of time. How long does it take for Zoloft to start working? As a rule, the first positive dynamics begin to be noticeable to the patient only after 2-3 weeks of regular use. The maximum effect is noticeable after 2-3 months of use.
Cancellation Features
When choosing antidepressants, it is important to know what medications the patient has previously taken and what medications he is currently taking. Before prescribing an effective drug that normalizes the functioning of the central nervous system, the doctor conducts a number of necessary examinations, identifies existing contraindications and prevents side effects. If Zoloft is not recommended for you, the specialist will offer you a wide range of analogues of this drug, including Cipralex, Prozac, Paxil, Cipramil and other equally effective drugs. The drug Velaxin, Amitriptyline, etc. have a similar effect.
If you experience withdrawal symptoms after taking Zoloft, seek help from the drug treatment center for Healthy Youth. We have been treating addictions for over 15 years.
Zoloft drug interactions
MAO inhibitors. The combined use of sertraline with MAO inhibitors is contraindicated (see SPECIAL INSTRUCTIONS). Other serotonergic drugs (see SPECIAL INSTRUCTIONS). Switching from taking selective serotonin reuptake inhibitors, antidepressants or anti-obsessive drugs (see SPECIAL INSTRUCTIONS). Pimozide. In a study of the combined use of a low dose of pimozide (2 mg once) and sertraline at a dose of 200 mg/day, an increase in the level of pimozide in the blood plasma was noted without any changes in the ECG. Since the mechanism of this interaction has not been established, and given the narrow therapeutic index of pimozide, the simultaneous use of sertraline and pimozide is contraindicated. CNS depressants and alcohol. The combined use of sertraline (200 mg/day) did not potentiate the effect of alcohol, carbamazepine, haloperidol or phenytoin on cognitive and psychomotor performance in healthy individuals; however, the simultaneous use of sertraline and alcohol is not recommended. Lithium. The combined use of sertraline and lithium did not significantly change the pharmacokinetics of lithium, however, tremor increased, which may indicate a pharmacodynamic interaction. With the simultaneous use of sertraline and lithium preparations, which affect serotonergic neuromediation, it is necessary to ensure appropriate control. Phenytoin. Long-term use of sertraline at a dose of 200 mg/day does not lead to clinically significant inhibition of phenytoin metabolism. Despite this, monitoring of phenytoin plasma concentrations during the initial phase of sertraline therapy with appropriate adjustment of the phenytoin dose should be recommended. In addition, concomitant use of phenytoin may cause a decrease in sertraline plasma concentrations. Sumatriptan. There are reports of isolated cases of the development of general weakness, hyperreflexia, impaired coordination, confusion, anxiety and agitation, which were observed after the simultaneous use of sertraline and sumatriptan. If it is necessary to prescribe sertraline and sumatriptan simultaneously, the patient should be under medical supervision. Drugs that bind to blood plasma proteins. Since sertraline binds to plasma proteins, it is necessary to consider the possibility of its interaction with other drugs that also bind to plasma proteins. However, in 3 studies, no significant effect of sertraline on the binding of diazepam, tolbutamide and warfarin to plasma proteins was detected. Warfarin. With simultaneous use of sertraline at a dose of 200 mg/day with warfarin, a slight but statistically significant increase in prothrombin time was observed; the clinical significance of this effect is unknown. In this regard, prothrombin time should be carefully monitored at the beginning of sertraline therapy and after its discontinuation. Interaction with other means. A number of studies have examined the interaction of sertraline with various drugs. The simultaneous use of sertraline at a dose of 200 mg/day with diazepam and tolbutamide led to a slight but statistically significant change in some pharmacokinetic parameters. Cimetidine caused a significant decrease in the clearance of sertraline when used simultaneously. The clinical significance of these changes is unknown. Sertraline did not affect the β-adrenergic blocking activity of atenolol. There were no signs of interaction of sertraline (at a dose of 200 mg/day) with glibenclamide and digoxin. Electroconvulsive therapy . The safety and effectiveness of the combined use of electroconvulsive therapy and sertraline have not been studied in clinical studies. Drugs metabolized with the participation of cytochrome P450 CYP 2D6. Antidepressant drugs have varying abilities to inhibit the activity of the 2D6 isoenzyme of cytochrome P450 CYP 2D6. The clinical significance of this depends on the degree of inhibition and the therapeutic index of the drug prescribed. CYP2D6 substrates with a low therapeutic index include tricyclic antidepressants and class Ic antiarrhythmics such as propafenone, flecainide. In studies of drug interactions with long-term use of sertraline at a dose of 50 mg/day, an increase (on average by 23–37%) in stable plasma levels of desipramine (a marker of CYP 2D6 activity) was detected. Drugs metabolized by other CYP isoenzymes (CYP 3A3/4, CYP 2C9, CYP 2C19, CYP 1A2). CYP 3A3/4: In vivo studies revealed that long-term use of sertraline at a dose of 200 mg/day does not inhibit CYP 3A3/4 dependent 6-β-hydroxylation of endogenous cortisol, or the metabolism of carbamazepine or terfenadine. In addition, long-term use of sertraline at a dose of 50 mg/day did not inhibit CYP 3A3/4, which is involved in the metabolism of alprazolam. The results of this study indicate that sertraline is not a clinically significant inhibitor of CYP3A3/4. CYP 2C9: Chronic use of sertraline 200 mg/day had no effect on plasma concentrations of tolbutamide, phenytoin, and warfarin, indicating that sertraline is not a clinically significant inhibitor of CYP 2C9. CYP 2C19: The use of sertraline at a dose of 200 mg/day did not affect the plasma concentrations of diazepam, indicating that sertraline is not a clinically significant inhibitor of CYP 2C19. CYP 1A2: In vitro studies indicate that sertraline has no or little effect on the activity of CYP 1A2.
Zoloft overdose
An overdose of the drug itself will not bring serious consequences to the human body. However, its combination with certain drugs, chemicals, alcohol and drugs is much more dangerous. Antidepressants are a fairly broad group of drugs, which in narcology are classified as pharmaceutical drugs that cause psychological dependence.
In pursuit of new vivid sensations, people often resort to taking pills in higher dosages, which often leads to addiction and overdose. Any drug, when used systematically in high dosages, will become poisonous to the body and lead to its intoxication. What will the combination of Zoloft and alcohol lead to? To the disruption of all vital systems of the body, especially the cardiovascular, as well as the nervous, respiratory, and vegetative-vascular systems. Such health deviations in most cases lead to death. In some cases, self-administration of incompatible drugs leads to intoxication. You need to be careful when taking antidepressants; they can easily cause addiction if you take them on a regular basis, independently prolong the course of treatment and increase their dose uncontrollably.
Symptoms of Zoloft overdose
What are the signs that indicate that a person has overdosed on a drug?
- Sleep disturbances, drowsiness.
- Tremor.
- Spasms, convulsions.
- Nausea, vomiting.
- Gastrointestinal disorder.
- cardiopalmus.
- Dizziness.
- Increased emotional excitability.
Only a doctor can eliminate the symptoms of an overdose. You have the opportunity to call an ambulance for drug treatment at home, or to hospitalize the victim yourself in a hospital. If you see that your loved one is feeling unwell, you know that he is taking antidepressants, you should seek help from a narcologist. A specialist will be able to take the necessary measures to relieve signs of overdose in a hospital or at home. This requires symptomatic therapy using a number of restorative and cleansing medications.
If you have taken too much Zoloft, you should seek emergency drug treatment. Call us, we will help: 8 (800) 551-41-71!
Zoloft overdose, symptoms and treatment
Sertraline has a wide range of safety in overdose. Cases of drug overdose have been recorded when taken in doses of up to 13.5 g; Fatal outcomes from sertraline overdose were mainly observed when it was used in combination with other drugs and/or alcohol. In case of overdose, intensive therapy is necessary. Symptoms of overdose include serotonin-related effects such as drowsiness, digestive disturbances (nausea and vomiting), tachycardia, tremor, agitation and dizziness. Coma very rarely develops. Treatment: There is no specific antidote; treatment is symptomatic and supportive. It is necessary to ensure a patent airway and adequate levels of ventilation and oxygenation. Taking activated charcoal, which can be used as a laxative, may be more effective than gastric lavage. Inducing vomiting is not recommended. Monitoring of cardiac function and other vital signs should be ensured. Given the large volume of distribution of sertraline, forced diuresis, dialysis, hemoperfusion and exchange transfusion are unlikely to be effective.
Contraindications
The drug is not prescribed if you are allergic to Zoloft or to any of the components of the drug. To determine whether there is an individual intolerance to the drug, the doctor must first examine the patient. It is important to know that the antipsychotic drug Pimozide and MAOIs (monoamine oxidase inhibitors) cannot be combined with Zoloft. Zoloft should not be used during pregnancy and lactation, or combined with alcohol.
Among the relative contraindications, it is worth using the drug for the following deviations from human health:
- epileptic seizures;
- mental retardation;
- brain pathologies;
- liver failure;
- severe exhaustion.