Mechanism of action of carbamazepine
According to its chemical structure, carbamazepine belongs to the group of tricyclic antidepressants.
In clinical practice, it is used as a sedative, normothymic and anticonvulsant substance. Pharmaceutical preparations based on it are characterized by low toxicity and low potential for addiction. Unfortunately, the mechanism of action of the substance is still not fully understood. It has been established that its administration makes it possible to stabilize the cell membranes (membranes) of hyperstimulated cells of the nervous system, for example, in epilepsy or acute psychosis with convulsive syndrome. At the same time, it suppresses the development of repeated excitation and inhibits the conduction of neuronal impulses.
Description of the drug CARBAMAZEPINE PHARMLAND
With simultaneous use of inhibitors of the CYP3A4 isoenzyme, an increase in the concentration of carbamazepine in the blood plasma is possible.
With the simultaneous use of inducers of the CYP3A4 isoenzyme system, it is possible to accelerate the metabolism of carbamazepine, reduce its concentration in the blood plasma, and reduce the therapeutic effect.
With simultaneous use, carbamazepine stimulates the metabolism of anticoagulants and folic acid.
When used simultaneously with valproic acid, a decrease in the concentration of carbamazepine and a significant decrease in the concentration of valproic acid in the blood plasma is possible. At the same time, the concentration of carbamazepine metabolite, carbamazepine epoxide, increases (probably due to inhibition of its conversion to carbamazepine-10,11-trans-diol), which also has anticonvulsant activity, so the effects of this interaction can be neutralized, but more often adverse reactions occur - blurred vision, dizziness, vomiting, weakness, nystagmus. With the simultaneous use of valproic acid and carbamazepine, a hepatotoxic effect may develop (apparently due to the formation of a minor metabolite of valproic acid, which has a hepatotoxic effect).
With simultaneous use, valpromide reduces the metabolism in the liver of carbamazepine and its metabolite carbamazepine-epoxide due to inhibition of the enzyme epoxide hydrolase. This metabolite has anticonvulsant activity, but with a significant increase in plasma concentration it can have a toxic effect.
When used simultaneously with verapamil, diltiazem, isoniazid, dextropropoxyphene, viloxazine, fluoxetine, fluvoxamine, cimetidine, acetazolamide, danazol, desipramine, nicotinamide (in adults, only in high doses), erythromycin, troleandomycin, josamycin, clarithromycin; with azoles (including itraconazole, ketoconazole, fluconazole), terfenadine, loratadine, it is possible to increase the concentration of carbamazepine in the blood plasma with the risk of side effects (dizziness, drowsiness, ataxia, diplopia).
When used simultaneously with hexamidine, the anticonvulsant effect of carbamazepine is weakened; with hydrochlorothiazide, furosemide - a decrease in sodium content in the blood is possible; with hormonal contraceptives - the effect of contraceptives may weaken and acyclic bleeding may develop.
When used simultaneously with thyroid hormones, it is possible to increase the elimination of thyroid hormones; with clonazepam - it is possible to increase the clearance of clonazepam and decrease the clearance of carbamazepine; with lithium preparations - a mutual enhancement of the neurotoxic effect is possible.
When used simultaneously with primidone, a decrease in the concentration of carbamazepine in the blood plasma is possible. There are reports that primidone may increase plasma concentrations of the pharmacologically active metabolite, carbamazepine 10,11-epoxide.
When used simultaneously with ritonavir, the side effects of carbamazepine may increase; with sertraline - a decrease in the concentration of sertraline is possible; with theophylline, rifampicin, cisplatin, doxorubicin - a decrease in the concentration of carbamazepine in the blood plasma is possible; with tetracycline - the effects of carbamazepine may be weakened.
With simultaneous use with felbamate, a decrease in the concentration of carbamazepine in the blood plasma is possible, but an increase in the concentration of the active metabolite of carbamazepine-epoxide, while a decrease in the plasma concentration of felbamate is possible.
When used simultaneously with phenytoin and phenobarbital, the concentration of carbamazepine in the blood plasma decreases. A mutual weakening of the anticonvulsant effect is possible, and in rare cases, its strengthening.
Use for alcoholism
In the treatment of any pathological conditions associated with long-term alcohol abuse, one-size-fits-all medications are never used. The choice of each medicine is approached with the utmost rigor, since in some cases it can only worsen the situation. The patient is thoroughly examined, after which the benefit/risk factor is assessed.
Indications
The main spectrum of action of the drug is the relief of seizures; to a lesser extent, the emotional background is normalized. Carbamazepine is used for alcoholism if the following indications exist:
- The structure of the syndrome of pathological craving for alcohol contains affective (psycho-emotional) disorders.
- Relief of withdrawal symptoms - “withdrawal” during the period of cessation of abuse in fully formed true binge drinking.
- Prevention of the development of convulsive attacks in cases of aggravated medical history.
- The patient is not suitable for other antidepressants or antiepileptic drugs.
Carbamazepine has been shown to be as effective as or superior to barbital, tiapride, clomethiazole, oxazepam, and placebo in open-label and double-blind studies. A double-blind study conducted by Malcolm et al. and repeated by Stuppaeck et al. demonstrated equal effectiveness of carbamazepine and oxazepam in relieving alcohol withdrawal. However, no differences were found in laboratory testing of liver and blood function, although carbamazepine may worsen these indicators. In addition to relieving withdrawal symptoms, carbamazepine, compared to oxazepam, more effectively improves the general condition of the patient, assessed according to the SCL-90-R criteria.”
Portal about medicines Medi Ru
Carbamazepine also enhances the positive effects of other neurotropic drugs that are used during the period of active anti-relapse treatment. In small dosages, it improves the emotional background, eliminates dysphoric symptoms (anxiety, depression, apathy) and reduces convulsive readiness. At the same time, the craving for drinking alcohol is suppressed.
Side effects and contraindications
The dose of the anticonvulsant is selected individually; the drug is usually well tolerated. Carbamazepine is contraindicated in case of clinically significant cardiac rhythm and conduction disturbances, hypersensitivity to tricyclic antidepressants, acute porphyria and a history of myelosuppression. The following side effects are possible:
- disturbance of taste and speech
- headache
- relapse of psychosis
- depression
- appearance of hallucinations
- dizziness
- excessive psychomotor agitation
- nystagmus – multi-frequency involuntary eye movements
- diplopia - double vision
- noise in ears
- conjunctivitis
- peripheral neuropathy
- muscle weakness up to paresis
- atrioventricular block
- worsening heart failure, including due to hemodynamic disorders (hypo- or hypertension)
- kidney damage
- nausea
- vomit
- toxic hepatitis
- thromboembolic complications if there is a predisposition
- electrolyte disorders
- allergic reactions
Carbamazepine
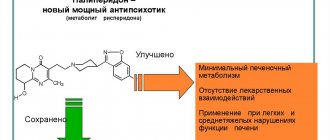
Cytochrome P4503A4 (CYP 3A4) is the main enzyme responsible for the formation of carbamazepine-10,11-epoxide (the active metabolite). Concomitant use with a drug that is an inhibitor of the CYP3A4 isoenzyme may lead to increased plasma concentrations of carbamazepine, which, in turn, may cause adverse reactions. The simultaneous use of inducers of the CYP3A4 isoenzyme may lead to an acceleration of the metabolism of carbamazepine and, thus, to a possible decrease in its concentration in plasma and, consequently, to a possible decrease in the severity of the therapeutic effect of the drug. Cancellation of concomitantly taken inducers of the CYP3A4 isoenzyme may reduce the rate of biotransformation of carbamazepine, and, as a result, lead to an increase in the concentration of carbamazepine in the blood plasma.
Carbamazepine is a strong inducer of CYP3A4 and phase 1 and 2 hepatic enzyme systems and, when used concomitantly with drugs metabolized by CYP3A4, can cause induction of metabolism and a decrease in plasma concentrations.
Since the conversion of carbamazepine-10,11-epoxide to carbamazepine-10,11-transdiol occurs with the help of the microsomal enzyme epoxide hydrolase, the use of carbamazepine together with epoxide hydrolase inhibitors may lead to an increase in the plasma concentration of carbamazepine-10,11-epoxide.
Drugs that may increase plasma concentrations of carbamazepine:
dextropropoxyphene, ibuprofen, danazol, macrolide antibiotics (eg, erythromycin, troleandomycin, josamycin, clarithromycin); fluoxetine, fluvoxamine, nefazodone, paroxetine, trazodone, viloxazine, stiripentol, vigabatrin, azoles (eg, itraconazole, ketoconazole, fluconazole, voriconazole), loratadine, terfenadine, olanzapine, isoniazid, viral protease inhibitors for the treatment of HIV infection (eg, ritonavir ), acetazolamide, verapamil, diltiazem, omeprazole, oxybutynin, dantrolene, ticlopidine, nicotinamide (in adults, only in high doses), possibly cimetidine, desipramine.
Since an increase in the level of carbamazepine in the blood plasma can lead to adverse reactions (for example, dizziness, drowsiness, ataxia, diplopia), in these situations the dose of the drug should be adjusted and/or the concentration of carbamazepine in the blood plasma should be regularly determined.
Drugs that may increase plasma concentrations of carbamazepine 10,11-epoxide
: loxapine, quetiapine, primidone, progabide, valproic acid, valnoctamide and valpromide.
Since an increase in the level of carbamazepine-10,11-epoxide in the blood plasma can lead to adverse reactions (for example, dizziness, somnolence, ataxia, diplopia), in these situations the dose of Zeptol should be adjusted and/or the concentration of carbamazepine-10,11 should be regularly determined -epoxide in blood plasma.
Drugs that may reduce plasma concentrations of carbamazepine
: felbamate, methsuximide, oxcarbazepine, phenobarbital, phensuximide, phenytoin and fosphenytoin, primidone, theophylline, aminophylline, isotretinoin, rifampicin, cisplatin or doxorubicin, herbal preparations containing St. John's wort (Hypericum perforatum), and although the data are partly conflicting, possibly also clonazepam . When used simultaneously with the above drugs, it may be necessary; Carbamazepine dose adjustment.
Effect of carbamazepine on plasma concentrations of drugs used as concomitant therapy
When used together with carbamazepine, a decrease in plasma concentration, a decrease or even a complete cessation of the effect of some drugs is possible.
When used simultaneously with carbamazepine, dose adjustment of the following drugs may be required: methadone, paracetamol, phenazone (antipyrine), tramadol, doxycycline, oral anticoagulants (warfarin, phenprocoumon, dicumarol and acenocoumarol), bupropion, citalopram, trazodone, tricyclic antidepressants (imipramine, amitriptyline, nortriptyline, clomipramine), clobazam, clonazepam, ethosuximide, felbamate, lamotrigine, oxcarbazepine, primidone, tiagabine, topiramate, valproic acid, zonisamide, itraconazole, praziquantel, imatinib, clozapine, haloperidol, bromperidol, olanzapine, quetiapine, risperidone, ziprasidone, used for HIV therapies (indinavir, ritonavir, saquinavir), alprazolam, midazolam, theophylline, calcium channel blockers of the dihydropyridine group (for example, felodipine), digoxin, oral contraceptives (selection of alternative methods of contraception is necessary), glucocorticosteroids (for example, prednisolone, dexamethosone) , cyclosporine, everolimus; levothyroxine, drugs containing estrogens and/or progesterone.
There are reports that while taking carbamazepine, the level of phenytoin in the blood plasma may either increase or decrease, and the level of mephenytoin may increase (in rare cases).
Combinations to Consider
When carbamazepine was prescribed together with levetiracetam, an increase in the toxic effect of carbamazepine was observed in some cases.
There are reports of increased hepatotoxicity caused by isoniazid in cases where it was used concomitantly with carbamazepine.
The combined use of carbamazepine and lithium or metoclopramide, as well as carbamazepine and antipsychotic drugs (haloperidol, thioridazine) can lead to an increase in the frequency of adverse neurological reactions (in the case of the latter combination, even with therapeutic concentrations of active substances in the blood plasma.
The simultaneous use of carbamazepine with some diuretics (hydrochlorothiazide, furosemide) can lead to hyponatremia, accompanied by clinical manifestations.
Carbamazepine may antagonize the effects of non-depolarizing muscle relaxants (eg, pancuronium bromide). In the case of using such combinations of drugs, it may be necessary to increase the dose of these muscle relaxants; Patients should be closely monitored as the effects of muscle relaxants may cease more quickly than expected.
Bleeding has been reported in women between menstrual periods when oral contraceptives were used at the same time. The drug may reduce the therapeutic effect of oral contraceptives due to the induction of microsomal enzymes.
Carbamazepine, like other psychotropic drugs, can reduce alcohol tolerance. In this regard, the patient is advised to stop drinking alcohol.
Coadministration with grapefruit juice may increase plasma levels of carbamazepine.