Write a review
Reviews: 0
Manufacturers: UPSA Laboratoires
Active ingredients
- Acetylsalicylic acid
- Caffeine
- Paracetamol
Disease class
- Other and unspecified lesions of the oral mucosa
- Joint pain
- Myalgia
- Headache
- Other constant pain
- Dysmenorrhea, unspecified
Clinical and pharmacological group
- Not indicated. See instructions
Pharmacological action
- Not indicated. See instructions
Pharmacological group
- NSAIDs - Salicylic acid derivatives in combinations
Exedrin oral tablets
Instructions for medical use of the drug
Description of pharmacological action
Excedrin® is a combination drug containing paracetamol, acetylsalicylic acid and caffeine. Paracetamol has an analgesic, antipyretic and extremely weak anti-inflammatory effect, which is associated with its effect on the thermoregulation center in the hypothalamus and a weak ability to inhibit the synthesis of prostaglandins in peripheral tissues. Acetylsalicylic acid has analgesic, antipyretic and anti-inflammatory effects. Quickly relieves pain, especially caused by the inflammatory process, and also moderately inhibits platelet aggregation and slows down the process of thrombus formation, improving microcirculation at the site of inflammation. Caffeine increases the reflex excitability of the spinal cord, stimulates the respiratory and vasomotor centers, dilates the blood vessels of skeletal muscles, brain, heart, kidneys, and reduces platelet aggregation. Reduces drowsiness, fatigue, increases mental and physical performance. In this combination, caffeine in a small dose has virtually no stimulating effect on the central nervous system, but helps to normalize cerebral vascular tone and accelerate blood flow in it.
Indications for use
Pain syndrome of moderate and mild intensity of various origins: headache, migraine, toothache, neuralgia, arthralgia and myalgia (pain in muscles and joints), algodismenorrhea (pain during menstruation).
Release form
pills; package 16; film-coated tablets; laminated aluminum foil bag 2, cardboard pack 1; film-coated tablets; blister 10, cardboard pack 1; film-coated tablets; blister 10, cardboard pack 2; film-coated tablets; blister 10, cardboard pack 3; film-coated tablets; polypropylene bottle (bottle) 50, cardboard pack 1; film-coated tablets; polypropylene bottle (bottle) 24, cardboard pack 1; Composition 1 tablet (caplet) contains paracetamol 250 mg, aspirin 250 mg and caffeine 65 mg; per pack 16 pcs.
Pharmacodynamics
Excedrin is a combination drug containing paracetamol, acetylsalicylic acid and caffeine. Paracetamol has an analgesic, antipyretic and extremely weak anti-inflammatory effect, which is associated with its effect on the thermoregulation center in the hypothalamus and a weak ability to inhibit the synthesis of prostaglandins in peripheral tissues. Acetylsalicylic acid has analgesic, antipyretic and anti-inflammatory effects. Quickly relieves pain, especially caused by the inflammatory process, and also moderately inhibits platelet aggregation and slows down the process of thrombus formation, improving microcirculation at the site of inflammation. Caffeine increases the reflex excitability of the spinal cord, stimulates the respiratory and vasomotor centers, dilates the blood vessels of skeletal muscles, brain, heart, kidneys, and reduces platelet aggregation. Reduces drowsiness, fatigue, increases mental and physical performance. In this combination, caffeine in a small dose has virtually no stimulating effect on the central nervous system, but helps to normalize cerebral vascular tone and accelerate blood flow in it.
Pharmacokinetics
Paracetamol is easily absorbed from the gastrointestinal tract, Cmax in blood plasma is detected from 30 minutes to 2 hours after administration. Paracetamol is metabolized in the liver and excreted by the kidneys, mainly in the form of glucuronides and sulfate conjugates. Less than 5% of paracetamol is excreted unchanged. The duration of T1/2 varies from 1 to 4 hours. Communication with plasma proteins is negligible at usual therapeutic doses, however, it increases as the dose increases. The hydroxylated metabolite, formed in small quantities in the liver under the influence of mixed oxidases and usually neutralized by binding to glutathione, can accumulate during an overdose of paracetamol and cause liver damage. Acetylsalicylic acid is quickly and completely absorbed, undergoes rapid hydrolysis in the gastrointestinal tract, liver and blood to the formation of salicylates, which undergo further metabolism, mainly in the liver. Caffeine is completely and quickly absorbed. Maximum concentrations are observed between 5 and 90 minutes after administration on an empty stomach. In adults, elimination occurs almost entirely through hepatic metabolism. There is marked variability in individual elimination values in adults. The average T1/2 from blood plasma is 4.9 hours in the range of 1.9-12.2 hours. Caffeine is distributed in all body fluids. The binding of caffeine to plasma proteins is 35%. Caffeine is almost completely metabolized by oxidation, demethylation and acetylation and is excreted by the kidneys. Main metabolites: 1-methylxanthine, 7-methylxanthine, 1.7-dimethylxanthine.
Use during pregnancy
Despite the fact that acetylsalicylic acid can be used in the second trimester of pregnancy, the safety of this combination in pregnant and breastfeeding women has not been studied, therefore the drug is contraindicated in pregnant women (in all trimesters) and breastfeeding women.
Use for renal impairment
Contraindicated: renal failure.
Contraindications for use
Hypersensitivity to any of the components in the drug, erosive and ulcerative lesions of the gastrointestinal tract in the acute phase, gastrointestinal bleeding, complete or incomplete combination of bronchial asthma, recurrent polypnosis of the nose and paranasal sinuses and intolerance to acetylsalicylic acid or other non-steroidal anti-inflammatory drugs (including including a history), surgical interventions accompanied by bleeding, hemophilia, hemorrhagic diathesis, hypoprothrombinemia, severe arterial hypertension, portal hypertension, severe ischemic heart disease, glaucoma, vitamin K deficiency, renal failure, simultaneous use of other drugs containing paracetamol, acetylsalicylic acid or other non-steroidal anti-inflammatory drug, glucose-6-phosphate dehydrogenase deficiency, pregnancy, lactation, increased excitability, sleep disorders, children under 15 years of age (risk of developing Reye's syndrome in children with hyperthermia due to viral diseases). Carefully. Gout, liver disease, headaches associated with head trauma, taking anticoagulants, hypoglycemic agents, gout or arthritis, as well as concomitant use of drugs containing acetylsalicylic acid or other analgesic and antipyretic components.
Side effects
Gastralgia, nausea, vomiting, hepatotoxicity, nephrotoxicity, erosive and ulcerative lesions of the gastrointestinal tract, allergic reactions, tachycardia, increased blood pressure, bronchospasm. With long-term use - dizziness, headache, visual impairment, tinnitus, decreased platelet aggregation, hypocoagulation, hemorrhagic syndrome (epistaxis, bleeding gums, purpura, etc.), kidney damage with papillary necrosis, deafness, malignant exudative erythema (syndrome) Stevens-Johnson), toxic epidermal necrolysis (Lyell's syndrome), Reye's syndrome in children (hyperpyrexia, metabolic acidosis, nervous system and mental disorders, vomiting, liver dysfunction).
Directions for use and doses
The drug is taken orally during or after meals. Adults and adolescents over 15 years of age: 1 tablet every 4-6 hours. At the first sign of migraine, take 2 tablets. The average daily dose is 3-4 tablets per day, the maximum daily dose is 6 tablets per day. After taking 2 tablets, relief from headaches and other types of pain usually occurs quickly - within 15 minutes; for migraines, relief usually occurs within 30 minutes. In case of pain, the drug should not be taken for more than 5 days without consulting a doctor. For migraines, the drug should not be taken for more than 3 days without consulting a doctor.
Overdose
Symptoms caused by the presence of paracetamol (when taken in doses of more than 10-15 g/day): during the first 24 hours, pallor of the skin, nausea, vomiting, anorexia, abdominal pain, impaired glucose metabolism, metabolic acidosis. Symptoms of liver dysfunction may appear 12-48 hours after an overdose. In case of severe overdose - liver failure with progressive encephalopathy, coma, death; acute renal failure with tubular necrosis (including in the absence of severe liver damage); arrhythmia, pancreatitis. The hepatotoxic effect in adults occurs when taking 10 g or more. Symptoms caused by the presence of acetylsalicylic acid (when taken in doses of more than 150 mg/kg): for mild intoxication - nausea, vomiting, tinnitus, blurred vision, dizziness, severe headache. In severe poisoning - hyperventilation of the lungs of central origin (shortness of breath, suffocation, cyanosis, cold sticky sweat, respiratory paralysis), respiratory acidosis. The greatest risk of developing chronic intoxication is observed in children and the elderly when taking more than 100 mg/kg/day for several days. For moderate to severe poisoning, hospitalization is required. Symptoms caused by the presence of caffeine (when taken in doses of more than 300 mg / day): gastralgia, agitation, anxiety, agitation, restlessness, confusion, delirium, dehydration, tachycardia, arrhythmia, hyperthermia, frequent urination, headache, increased tactile or pain sensitivity, tremors or muscle twitching; nausea and vomiting, sometimes with blood; ringing in the ears, epileptic seizures (in case of acute overdose - tonic-clonic). Treatment: monitoring the acid-base status and electrolyte balance. Depending on the metabolic state, administration of sodium bicarbonate, sodium citrate or sodium lactate. Increasing alkalinity enhances the excretion of acetylsalicylic acid due to alkalinization of urine. Gastric lavage in the first 4 hours, provocation of vomiting, taking activated charcoal, laxatives, administration of SH-group donors and precursors for the synthesis of glutathione methionine within 8-9 hours after an overdose and acetylcysteine - within 8 hours.
Interactions with other drugs
The drug may enhance the effect of heparin, indirect coagulants, reserpine, steroid hormones and hypoglycemic drugs. Concomitant use with other non-steroidal anti-inflammatory drugs and methotrexate increases the risk of side effects. Reduces the effectiveness of spironolactone, furosemide, antihypertensive drugs, as well as anti-gout drugs that promote the excretion of uric acid. Barbiturates, rifampicin, salicylamide, antiepileptic drugs and other inducers of microsomal liver enzymes contribute to the formation of toxic paracetamol metabolites that affect liver function. Metoclopramide accelerates the absorption of paracetamol. Under the influence of paracetamol, the half-life of chloramphenicol increases 5 times. When taken repeatedly, paracetamol may enhance the effect of anticoagulants (coumarin derivatives). Simultaneous use of paracetamol, acetylsalicylic acid and alcoholic beverages increases the risk of developing hepatotoxic effects. Caffeine accelerates the absorption of ergotamine.
Special instructions for use
If symptoms persist, worsen, or new symptoms occur after taking the drug, you should immediately consult a doctor. When taking the drug at the recommended dose, the body receives the same amount of caffeine as is contained in one cup of coffee, so you should reduce the consumption of caffeine-containing products when treating with this drug in order to avoid the development of nervous agitation, irritability, insomnia and rapid heartbeat due to caffeine overdose. If you suspect an overdose, seek immediate medical attention, even if you have no symptoms. You should avoid drinking alcohol while taking the drug due to an increased risk of liver damage and gastrointestinal bleeding. Since acetylsalicylic acid slows down blood clotting, a patient undergoing surgery should notify the doctor in advance about taking the drug. Acetylsalicylic acid in low doses reduces the excretion of uric acid, and therefore in patients with a predisposition, the drug can provoke an attack of gout. With prolonged use of the drug, monitoring of peripheral blood and the functional state of the liver is necessary. Impact on the ability to drive vehicles and operate machinery. The effect of the drug on the ability to drive a car and operate machinery has not been reported.
Storage conditions
In a dry place, at a temperature not exceeding 25 °C.
Best before date
60 months
ATX classification:
N Nervous system
N02 Analgesics
N02B Analgesics and antipyretics
N02BA Salicylic acid and its derivatives
N02BA71 Acetylsalicylic acid in combination with psychotropic drugs
Preventive treatment of migraine: yesterday, today, tomorrow
O.E. Dubenko, D.D. Sotnikov Kharkov Medical Academy of Postgraduate Education
Migraine is one of the most common and socially significant diseases among people of all countries of the globe, races and social classes. According to epidemiological studies, in developed countries of Europe and America, migraine affects from 3 to 16% of the population, and according to some data, up to 30%; among women, 18% suffer from migraine, among men - 6%, and among children - 4% [1]. The economic costs associated with temporary disability and treatment of migraine are comparable to those for cardiovascular diseases [2]. The economic costs associated with migraine consist of the cost of medications and medical care (direct costs), as well as days of disability and lost productivity (indirect costs) [3], and in the United States in particular amount to about $13 billion per year, and severe a form of migraine is no less a disabling disorder than a number of conditions whose social and medical significance is not questioned (for example, hemi- and paraplegia) [4]. Although the history of migraine research is as old as the history of medicine, the mechanisms responsible for the origin of migraine attacks remain poorly understood. Recent decades have been marked by significant advances in the study of the pathophysiology of migraine: changes in cerebral blood flow during an attack have been identified, the effects of neurotransmitters and neuropeptides, and interactions between neuronal and vascular factors, called the trigeminovascular reflex, have been studied. A source of hope for millions of people suffering from migraine was the creation of a group of drugs - triptans - to relieve a migraine attack. However, preventive treatment for migraine, which a significant proportion of migraine sufferers require, is still far from perfect, and the search for new effective treatments continues. Today, most researchers agree that migraine is based on a complex set of interactions between the cerebral vessels, the trigeminal system and the central nervous system. The key role of aseptic inflammation in the mechanisms of migraine headache formation, which develops under the influence of a trigger factor due to the release of vasoactive neuropeptides (substance P, neurokinin A, calcitonin gene-related peptide (CGRP)) from the terminals of sensory nerve fibers of the trigeminal nerve, has been recognized. These neuropeptides cause vasodilation, increased permeability of the vascular wall, sweating of plasma proteins, swelling of the vascular wall and adjacent areas of the dura mater, degranulation of mast cells, and platelet aggregation. Due to the anatomical features of the trigeminal nerve, pain radiates to the fronto-orbital-temporal region. The symptoms of migraine aura are a manifestation of neuronal cortical depolarization of neurons (spreading cortical depression of Leao). It is also believed that migraine is a primary neurogenic cerebral dysfunction with the presence of a genetically determined brainstem insufficiency (“stem generator of migraine”) and impaired functioning of the nociceptive and antinociceptive systems of the brain in the direction of reducing endogenous pain control [5-7]. Based on the pathogenesis of migraine headaches, potential mechanisms of preventive agents can be identified:
- Prevention of neurogenic inflammation in the dura mater.
- Increased activity of antinociceptive systems of the brain.
- Modulation of the activity of noradrenergic, cholinergic and serotonergic systems.
- Suppression of spreading cortical depression.
Migraine is a lifelong suffering, but with varying frequency and severity of attacks throughout life. Some patients are forced to take medications for many years, so the ideal drug should be well tolerated, have a low range of side effects and have a rapid onset of effect.
The first attempts at preventive treatment of migraine were made in the 16th century. At this time, laxatives were recommended, believing that migraine attacks could be caused by intoxication due to weak bowel function. In the 19th century, various remedies began to be used: herbs such as valerian, tansy, hemp (which was the standard therapy), as well as belladonna derivatives, sodium bromide, phenobarbital and combinations thereof. Govers' mixture is known, containing strychnine, sodium bromide, phenazone (a pyrazolone derivative) and Galzemi tincture. Bequerel pills contained quinine sulfate, digitalis and colchicine. In addition, some doctors recommended a special diet, physical exercise and relaxation at resorts [8]. Modern preventive treatment for migraine began with dihydroergotamine. The medicinal effects of the ergot alkaloid, ergotamine, were first discovered by the Swiss scientist A. Stoll in 1917. Since 1925, migraines have been successfully treated with subcutaneous administration of ergotamine. In the classic works of J. Graham and H. Wolff in 1938, it was established that intravenous administration of ergotamine causes a distinct vasoconstriction of the dilated branches of the external carotid artery during migraine headache, which is accompanied by its reduction [9]. One of the leading specialists in the field of migraine, A. Prusinsky, in the 60-70s, considered ergot derivatives to be the main means for the preventive treatment of migraine [10]. The mechanism of action of ergotamine is complex; it is an agonist of α-adrenergic receptors, serotonin (especially HT1B/D) and dopamine D2 receptors. Ergotamine and dihydroergotamine have the ability to inhibit the phenomenon of plasma extravasation in the dura mater upon stimulation of the trigeminal ganglion, which is associated with the ability to block the release of neuropeptides from perivascular nerve terminals [11]. Current recommendations for the management of migraine no longer include ergotamine as a preventative treatment. The list of preventive medications recommended for migraine includes several dozen. The main groups of drugs are beta blockers, antiserotonin drugs, calcium antagonists, antidepressants, antiepileptic drugs. In general, none of these drugs is ideal, has a number of side effects and is no more than 50% effective in preventing attacks.
Antiserotonin drugs have become the next step in migraine prevention. In the 70-80s, a number of experimental studies showed that methysergide and pizotifen are capable of causing vasoconstriction in the carotid arterial system without increasing systemic blood pressure, that is, selectively influencing the carotid circulation [12]. Since then, methysergide, whose chemical formula is similar to ergotamine, has been actively used for the preventive treatment of migraine at a dose of 2-6 mg per day. However, a number of side effects such as drowsiness, gastrointestinal complications and even retroperitoneal fibrosis limit its use. An analysis of two multicenter studies showed that pizotifen does not reduce the severity of migraine, but may promote weight gain and is indicated only for patients with a frequency of 4 or more attacks per month [13].
Beta blockers have been used to treat migraine for over 30 years and continue to be considered one of the most effective treatments, although their mechanism of action in migraine remains unclear. The main drug in this group for the treatment of migraine is propranolol in an individually selected dose from 80 to 240 mg. About 60 studies were conducted to study its effectiveness; a positive effect was noted in 50-70% of patients. Propranolol is one of the first-line drugs for the preventive treatment of migraine [14]. Metoprolol, atenolol and timolol are also used [15, 16]. The mechanism of action of beta blockers is not fully known. It is assumed that they are able to modulate the activity of antinociceptive systems of the brain, as well as prevent vasodilation of cerebral vessels [17]. Beta blockers are a heterogeneous group; beta blockers without intrinsic sympathomimetic activity are more effective for migraine. Therefore, acebutolol, alprenolol, oxprenolol and pindolol show no prophylactic effect in the treatment of migraine. The most common side effects of beta blockers may be psycho-emotional disorders such as drowsiness, fatigue, lethargy, sleep disturbances, nightmares, depression, memory loss and hallucinations. The possible occurrence of muscle weakness limits their use in athletes. In addition, bradycardia, hypotension, and bronchospasm sometimes develop. Based on this, it is advisable to use beta blockers for concomitant cardiovascular pathology and anxiety disorders, however, they are contraindicated in patients with depression, diabetes mellitus and bronchial asthma.
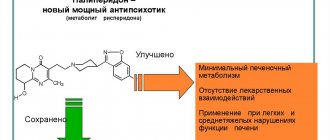
Calcium antagonists. The effect of Ca2 channel blockers in the prevention of migraine is associated with their ability to prevent neuronal hypoxia, contraction of cerebral vascular smooth muscle, inhibit Ca2-dependent enzymes involved in the formation of prostaglandins and prevent the initiation of spreading cortical depression. In addition, they are likely to have an antagonistic effect on serotonin and dopamine receptors [17]. The discovery of the influence of the state of cerebral specific P/Q-type calcium channels in the occurrence of familial hemiplegic migraine has led to an expansion of the role of calcium channel blockers in the treatment of migraine [18]. Of the drugs in this group, flunarizine is the most effective in preventing migraines, while nimodipine and nifedipine are probably not. Side effects of flunarizine include parkinsonism, depression, and weight gain. The effectiveness of verapamil, despite its widespread use in the United States, is questionable [19]. It is advisable to use drugs in this group for migraines accompanied by neurological symptoms of a vascular nature, for example, basilar, hemiplegic migraines, migraines with visual aura and prolonged ones.
The clinical effectiveness of ACE inhibitors and angiotensin II inhibitors confirms the role of the renin-angiotensin system in the pathogenesis of migraine. The effect of drugs in this group is associated not with the effect on blood pressure, but probably with the modulation of receptors in the central nervous system [20]. The use of lisinopril at a dose of 20 mg led to a reduction in headache days by 17% [21].
Several placebo-controlled studies have shown the effectiveness of non-steroidal anti-inflammatory drugs such as ketoprofen, naproxen, mefenamic acid for the preventive treatment of migraine [22, 23], but their long-term use can cause gastrointestinal complications.
The positive effect of some antidepressants (amitriptyline, nortriptyline, fluoxetine) on migraine is associated with their pharmacological effects, such as the effect on the metabolism of serotonin, norepinephrine and dopamine. However, their mechanism of action in migraine is unclear. It is known that the effectiveness of antidepressants for migraine does not depend on their psychotropic effect [24]. It is assumed that their effectiveness is associated with modulation of the activity of serotonergic neurons in the central nervous system [25]. This position is based on data from experimental and clinical studies indicating increased sensitivity of 5HT2 type serotonin receptors and reduced levels of serotonin in the central nervous system during the interictal period of the disease [26]. One of the most effective antidepressants used for the prevention of migraine and classified as first-line drugs is amitriptyline, which blocks the reuptake of serotonin and norepinephrine in the central nervous system and antagonizes 5HT2 receptors [27]. The most common side effects of antidepressants are dry mouth, muscle weakness, drowsiness, dizziness, constipation, and tachycardia.
Numerous accumulated data on the comorbidity of migraine and epilepsy have become the basis for the widespread use of antiepileptic drugs, such as valproic acid, gabapentin and topiramate, etc., in the preventive treatment of migraine [28]. Their effectiveness may be due to their effects on ion channels, neurotransmitter metabolism, and neurotransmitter receptors. Many antiepileptic drugs combine several mechanisms of influence on the excitability of neuronal membranes and have the ability to increase the concentration of gamma-aminobutyric acid in the central nervous system with a subsequent effect on the state of calcium and sodium membrane channels. In addition, they mediate their antimigraine effect through their influence on serotonergic neurotransmission in the raphe nuclei of the brainstem, as well as through antagonism of glutamate [29, 30]. Thus, lamotrigine blocks voltage-gated sodium channels and thus reduces the sensitization of nociceptive neurons. In addition, it limits the release of excitatory amino acids from the central terminals of pain receptors, in particular glutamate, thereby preventing spreading cortical neuronal depression, which is associated with the occurrence of aura. This explains the greater effectiveness of lamotrigine when used by patients with migraine with aura - 67% experienced a decrease in the frequency and duration of aura [31]. Lamotrigine also has normothimic and antidepressant properties. For more than 10 years, a relatively new anticonvulsant, gabapentin, a structural analogue of GABA, has been used in clinical practice. The mechanism of the analgesic action of gabapentin has not yet been precisely established. It has been shown that it interacts with α2δ-subunits of voltage-gated calcium channels, preventing overload of neurons with calcium ions, increases the synthesis of GABA, stimulating the activity of glutamate decarboxylase, reduces the amount of the excitatory neurotransmitter glutamate, and also modulates the activity of NMDA receptors. Gabapentin at an individualized dose of 900 to 2400 mg was statistically significantly more effective than placebo in the preventive treatment of migraine for 12 weeks [32]. A number of studies have proven the effectiveness of valproate in low doses (250-500 mg twice a day), and in some countries they are recommended as first-line drugs for the prevention of migraine [33]. However, their potential teratogenic effect must be taken into account when used in young women.
To date, a significant evidence base has been accumulated on the effectiveness of topiramate in the preventive treatment of migraine. Topiramate has multiple mechanisms of action, which makes it effective for the treatment of epilepsy and migraine. The most studied mechanisms include: blockade of voltage-dependent sodium channels, which limits the continuous flow of sodium ions into the cell; potentiation of the action of GABA by activating GABAA receptors through non-benzodiazepine and non-barbituric mechanisms; inhibition of glutamatergic transmission; decreased activity of the L-subtype calcium channels; inhibition of carbonic anhydrase [34]. Clinical studies have shown that topiramate is effective in preventing migraine attacks, significantly reducing their frequency. Its effect develops quite quickly—during the first month of therapy, there is a persistent, long-term reduction in the number of attacks without the development of resistance [35]. Compared to other anticonvulsants, topiramate has a favorable tolerability profile. In addition, with long-term use of topiramate, unlike most anticonvulsants, there is no increase in body weight, but, on the contrary, a decrease in body weight. In randomized 483 patients, a significant reduction in the number of migraine days per month was observed when taking topiramate at a daily dose of 100–200 mg compared with placebo [36].
Current guidelines for the management of patients with migraine recommend preventive therapy in the presence of two or more migraine attacks per month [37]. Drug treatment should ideally be prescribed after non-drug measures and the exclusion of provoking factors (for example, drinking red wine, long breaks in meals, late awakenings, etc.) do not produce an effect.
Analysis of the results of numerous studies made it possible to formulate the basic principles and indications for preventive therapy for migraine (US Headache Consortium Guidelines) [38]. Indications for prescribing preventive treatment are:
- recurrent migraine attacks that reduce daily activity despite taking relief medications (two or more attacks per month that cause maladjustment for more than 3 days, or attacks that are less frequent but cause deeper maladjustment);
- ineffectiveness, side effects or contraindications for the relief of attacks;
- special circumstances such as hemiplegic migraine or attacks with a high risk of developing a permanent neurological defect;
- very high frequency of headaches (more than 2 times per month) or a pattern of increasing frequency with a risk of developing drug-induced headache due to repeated use of abortifacients.
Principles of preventive therapy
- The choice of drug among highly effective prophylactic agents should be based on effectiveness, tolerability and comorbidity.
- Treatment should begin with a small dose and gradually increase until therapeutic improvement or side effects occur.
- The prescribed drug is taken for a long time, from 2 to 6 months, the effect is expected after 4 weeks of use and progressive improvement is expected over three months.
- In the presence of a comorbid disease, the therapeutic dose should be adequate for both diseases.
- When headaches become manageable, the dose of the drug is reduced with the possible gradual withdrawal of preventive treatment.
Despite proven high effectiveness, preventive treatment is underused. According to the results of the American Migraine Study II (AMSII), a large telephone interview, only 5% of migraine patients receive preventive treatment [39]. The importance of correct diagnosis of migraine and the effectiveness of preventive treatment is also related to the fact that numerous epidemiological studies have revealed a connection between migraine and stroke, especially in young women suffering from migraine with aura. Migraine is associated with a 16-fold increase in the risk of stroke in pregnancy and the overall risk of cardiovascular events in women [40]. The finding of a high incidence of migraine among young people with stroke has led to the hypothesis that migraine may be a risk factor for ischemic stroke. Neuroimaging studies have shown that migraine may not only be a risk factor for stroke, but also for silent infarctions and white matter lesions in the brain. These changes are more common in women with migraine with aura and are associated with severe and frequent attacks [41].
Genetic studies in migraine have improved our understanding of the mechanisms of migraine attacks and their relationship with trigger factors, which leads to more specific and effective use of medications for preventive treatment [42]. The first discovered migraine gene was the so-called CAC-NA 1A gene on chromosome 19p13, encoding the a1A subunit of neuronal P/Q calcium channels. These channels are involved in modulating the release of neurotransmitters including monoamines, acetylcholine, glutamate, substance P, and calcitonin gene-related peptide. Various mutations of this gene are associated with a wide range of neurological diseases: familial hemiplegic migraine, episodic ataxia type 2, epilepsy and a combination of these diseases. Intensive biochemical, neuropharmacological and genetic studies have identified other mutations. It was revealed that familial hemiplegic migraine is associated with a mutation of the AT3A2 gene on chromosome 1q23, encoding Na+, K+ and ATPase ion channels. Mutation of this gene is also associated with various types of epilepsy. Other loci associated with migraine are 1q, 3p21, 6p12-21 (migraine with and without aura), Notch 3 CADASIL gene (migraine and white matter pathology).
A number of studies have shown the effectiveness of botulinum toxin type A at a dose of 260 units in people suffering from migraines and daily headaches. The effectiveness of botulinum toxin for headaches was first noted by plastic surgeon William Binder when many of his patients who received botulinum toxin injections to correct facial wrinkles in the glabellar region noted a decrease in the frequency and severity of headaches. For migraine, botulinum toxin type A preparations are usually injected into the glabella, temporal, frontal and sometimes occipital areas. It is believed that botulinum toxin may reduce the release of not only acetylcholine, but also other neurotransmitters, in particular glutamate and substance P, suppressing neurogenic inflammation. The use of Botox reduced the frequency of migraine attacks, the number of headache days per month, and the use of medications for acute headache relief [43, 44].
To evaluate the therapeutic potential in the preventive treatment of migraine, a double-blind, 12-week controlled trial of subcutaneous histamine injection (1-10 mg twice weekly) was conducted versus topiramate 100 mg daily. The results showed identical effectiveness of these two agents in reducing attack frequency by 50%, reducing pain intensity by 51%, reducing attack duration by 55%, and reducing migraine disability scale (MIDAS) scores by 75% [45]. The therapeutic effect of histamine in migraine is explained by specific mechanisms of inhibition of neurogenic edema, degranulation of mast cells and the release of neuromodulatory peptides from the endings of C-fibers, which is explained by the interaction of histamine with H3 receptors and represents a local feedback loop between C-fibers of nerve endings and mast cells that control neurogenic inflammation [46]. In addition, subcutaneous histamine injections did not cause side effects other than transient pain at the injection sites, whereas in the topiramate treatment group, 22% of patients refused treatment due to side effects such as paresthesia, weakness and dizziness. Thus, subcutaneous histamine injections may be a new therapeutic strategy in the preventive treatment of migraine, especially in patients with gastritis and intolerance to other medications.
Drugs from the triptan group were usually used to relieve migraine attacks, but recent studies have attempted to use triptans with a long half-life (frovatriptan, naratriptan) for preventive treatment. Thus, a randomized, double-blind, placebo-controlled study of frovatriptan 2.5 mg twice daily for 6 days led to a reduction in the frequency and duration of menstrual migraine [47].
Thus, preventive therapy for migraine is aimed at reducing the frequency of attacks and preventing the development of chronic migraine. Despite the extensive accumulated knowledge about the possibility of using various drugs in the preventive treatment of migraine, there are still no universal remedies. Perhaps future research will help create them.
References 1. Rasmussen BK, Jensen R., Schroll M., Olesen J. Epidemiology of headache in a general population. A prevalence study // J. Clin. Epidemiol. - 1991. - Vol. 11. - P. 1147-1157. 2. Filatova E.G., Klimov M.V. Anticonvulsants in the preventive therapy of migraine // Journal of Neurology and Psychiatry. - 2003. - No. 10. - P. 65-67. 3. Brown JS, Papadopoulos G., Neumann PJ, Friedman M., Miller JD, Menzin J. Cost-effectiveness of topiramate in migraine prevention: results from a pharmacoeconomic model of topiramate treatment // Headache. - 2005. - Vol. 45. - P. 1012-1022. 4. Lipton RB, Newman LC Epidemiology, impact, and comorbidities of migraine headaches in the United States // Neurology. - 2003. - Vol. 60 - P. 3-8. 5. Goatsby PJ Migraine pathophysiology // Headache. - 2005. - Vol.45., Suppl.1. — P.s14-s24. Buzzi MG, Moskowitz MA The pathophysiology of migraine: year of 2005 // J. Headache Pain. - 2005. - Vol. 6. - P. 105-111. 6. Goatsby PJ Recent advances in the diagnosis and management of migraine // BMJ. - 2006. - Vol. 332. - P. 25-29. 8. Migraine in General Practice: basic concepts / Editor Karl Ekbom, 1993. - Smith-Gordon, 112 p. 9. Tabeeva G.R. Specific treatment of migraine: the story of one triptan // Journal of Neurology and Psychiatry named after S.S. Korsakov. - 2007. - T. 107, No. 5. - P. 75-78. 10. Prusinsky A. Migraine. - Moscow: Medicine, 1979. - 198 p. 11. Silberstein SD, Mc Grory DC, Ergotamine and dihydroergotamine: history, pharmacology and efficacy // Headache. - 2003. - Vol. 43. - P. 144-146. 12. Saxena PR Selective in carotid vascular by methysergide: possible prevalence to its antimigraine effect // Eur. J. Pharmacol. - 1974. - Vol. 27. - R. 99-105. 13. Cleland PG, Barnes D., Elrington GM, Loizou LA, Rawes GD Studies to Assess if Pizotifen Prophylaxis improves Migraine beyond the Benefit Offered by Acute Sumatriptan Therapy alone // European Neurology. - 1997. - Vol. 38, No. 1. - P. 31-38. 14. Duhlof C. Flunarizine versus long-acting propranolol in the prophylactic treatment of migraine / A double-blind study with parallel groups // Furyher advances in headache research / Ed. Clifford Rose F. - 1989, London, Smith-Gordon. - R. 281-290. 15. Ljung O. Metoprolol in migraine // Cephalgia. - 1981. - Vol. 1. - P. 142. 16. Johannsson V., Nilsson L.R., Widelius T. et al. Atenolol in migraine prophylaxis: A double blind crossover multicentric study // Headache. - 1987. - Vol. 27. - P. 372-374. 17. Silberstein SD, Goadsby PJ Migraine: preventive treatment // Cephalalgia. - 2002. - Vol. 22. - R. 491-512. 18. Ophoff RA et al. Familial hemiplegic migraine and episodic ataxia type-2 are caused by mutations in the Ca2+ channel gene CACNLA4 // Cell. - 1996. - Vol. 87. - R. 543-552. 19. Herbert G, Markley MD, Cohn CD et al. Verapamil in prophylactic therapy of migraine // Neurology. - 1984. - Vol. 34. - P. 973-976. 20. Tronvik E., Stovner LJ, Bovim G. Involvement of the rennin-angiotensin system in migraine // J. Hypertens. - 2006. - Vol. 24. - P. S139-S143. 21. Schrader H., Stovner LJ, Helde GT, Bovim G. Prophylactic treatment of migraine with angiotensin converting enzyme inhibitor (lisinopril): randomized, placebo-controlled, crossover study // BMJ. - 2001. - Vol. 322. - P. 19-22. 22. Welch KM, Ellis DJ, Keenan PA Successful migraine prophylaxis with naproxen sodium // Neurology. - 1985. - Vol. 92. - P. 1198-1199. 23. Johnson RH, Hornabrook RW, Lambie DG Comparison of mefenamic acid and propranolol with placebo in migraine prophylaxis // Acta Neurol. Scand. - 1986. - Vol. 73. - P. 490-492. 24. Peatfield RC, Fozard JR, Rose FC Drug treatment of migraine // Handbook of Clinical Neurology. - New York: Elsevier, 1986. - Vol. 4. - P. 173-216. 25. Goadsby, PJ Can we develop neurally acting drugs for the treatment of migraine? //Nat. Rev. Drug Discov. - 2005. - Vol. 4. - R. 741-750. 26. Maertens de Noordhout A., Wang W., Schoenen J. Clinical neurophysiology and neurotransmitters // Cephalgia. - 1995. - Vol. 15. - P. 301-309. 27. Krymchantowski AV, Silva MT, Barbosa JS, et al. Amitriptyline versus amitriptyline combined with fluoxetine in the preventative treatment of transformed migraine: a double-blind study // Headache. - 2002. - Vol. 42. - R. 510-514. 28. Tabeeva G.R., Azimova Yu.E. The nature of comorbidity of migraine and epilepsy // Neurological Journal. - 2007. - T. 12, No. 5. - P. 36-44. 29. Curter FM Antiepileptic drugs: how they work in headache // Headache. - 2001. - Vol. 41, Suppl. 1. - P. s3-s10. 30. Mathew NT Antiepileptic drug in migraine prevention // Headache. - 2001. - Vol. 41, Suppl. 1. - P. s18-s24. 31. Wheeler, SD Lamotrigine efficacy in migraine prevention // Cephalalgia. - 2001. - Vol. 21. - R. 374. 32. Mathew NT, Rappoport A., Saper J. et al. Efficacy of gabapentin in migraine prophylaxis // Headache. - 2001. - Vol. 41. - P. 119-128. 33. Freitag FG, Collins SD, Carlson HA et.al. A randomized trial of divalproex sodium extended-release tablets in migraine prophylaxis // Neurology. - 2002. - Vol. 58. - P. 1652-1659. 34. White YS Molecular pharmacology of topiramate: managing seizures and preventing migraine // Headache. - 2005. - Vol. 45, Suppl. 1. - P. s48-s56. 35. Silberstein, SD Topiramate in migraine prevention // Headache. - 2005. - Vol. 45. - P. S57-S65. 36. Brandes JL, Saper JR, Diamond M. et al. MIGR-002 Study Group. Topiramate for migraine prevention: a randomized controlled trial // JAMA. - 2004. - Vol. 291. - P. 965-973. 37. Silberstein SD Preventive treatment of migraine // Rev. Neurol. Dis. - 2005. - Vol. 2. - P. 167-175. 38. Dodic DW, Silberstein, SD Migraine prevention // Practical Neurology. - 2007. - Vol. 7. - R. 383-393. 39. Lipton RB et al. Migraine in the United States: epidemiology and patterns of health care use // Neurology. - 2002. - Vol. 58. - R. 885-894. 40. Bushell CD Migraine and stroke // International Journal of Stroke. - 2008. - Vol. 3, Suppl. 1. — P. 45. 41. Diener HC Migraine — a progressive disorder better prevented? // The Abstr. of the 9th Congress of the European Federation of Neurological Societies, Athens, Greece, 17-20 Sept. 2005 // European Journal of Neurology. - 2005. - Vol. 12, Suppl. 2. - P. 4. 42. Ferrari MD From migraine patients to migraine genes: Why do patients get attack? // The Abstr. of the 9th Congress of the European Federation of Neurological Societies, Athens, Greece, 17-20 Sept. 2005 // European Journal of Neurology. - 2005. - Vol. 12, Suppl. 2. - P. 3-4. 43. Freitag FG, McAllister P, Freud B. et al. Botulinum toxin type A for the prophylaxis of chronic daily headache in migraineurs: Effect on acute headache pain medication use // The Abstr. of the 9th Congress of the European Federation of Neurological Societies, Athens, Greece, 17-20 Sept. 2005 // European Journal of Neurology. - 2005. - Vol. 12, Suppl. 2. - P. 197. 44. Saper JR, Brandes JL, Wrubel B. et al. Efficacy of prophylactic treatment with botulinum toxin type A in migraineurs with chronic daily headache overusing acute headache pain medication // The Abstr. of the 9th Congress of the European Federation of Neurological Societies, Athens, Greece, 17-20 Sept. 2005 // European Journal of Neurology. - 2005. - Vol. 12, Suppl. 2. - P. 197. 45. Millan-Guerrero RO, Isais-Millan R., Barreto-Vizcaino S. et al. Subcutaneous Histamine versus Topiramate in Migraine Prophylaxis: A Double-Blind Study // Eur. Neurol. - 2008. - Vol. 59, Suppl. 5. - P. 237-242. 46. Akerman S., Williamson DJ, Kaube H., Goadsby PJ The role of histamine in dural vessel dilatation // Brain Res. - 2002. - Vol. 956. - P. 96-102. 47. Silberstein SD, Elkind AH, Schreiber C, Keywood C. A randomized trial of frovatriptan for the intermittent prevention of menstrual migraine. Neurology. - 2004. - Vol. 63. - R. 261-269.
Similar drugs:
- Carsil Dragee
- Ascorutin Oral tablets
- Yogurt Capsule
- Ergoferon () Lozenges
- Magne B6 Oral tablets
- Omez Capsule
- Papaverine Oral tablets
** The Drug Directory is intended for informational purposes only. For more complete information, please refer to the manufacturer's instructions. Do not self-medicate; Before you start using Excedrin, you should consult your doctor. EUROLAB is not responsible for the consequences caused by the use of information posted on the portal. Any information on the site does not replace medical advice and cannot serve as a guarantee of the positive effect of the drug.
Are you interested in Excedrin? Do you want to know more detailed information or do you need a doctor's examination? Or do you need an inspection? You can make an appointment with a doctor - the Euro lab is always at your service! The best doctors will examine you, advise you, provide the necessary assistance and make a diagnosis. You can also call a doctor at home . Euro lab clinic is open for you around the clock.
** Attention! The information presented in this medication guide is intended for medical professionals and should not be used as a basis for self-medication. The description of the drug Excedrin is provided for informational purposes only and is not intended for prescribing treatment without the participation of a doctor. Patients need to consult a specialist!
If you are interested in any other drugs and medications, their descriptions and instructions for use, information about the composition and form of release, indications for use and side effects, methods of use, prices and reviews of drugs, or you have any other questions and suggestions - write to us, we will definitely try to help you.