Stroke is a serious disease that causes destructive changes in brain cells as a result of circulatory problems. The most severe form of pathology is an extensive stroke, as a result of which several areas of brain tissue are affected, which leads to the formation of persistent irreversible disorders, including death. The consequences of a major stroke are serious, so the chances of survival and further prognosis are quite unfavorable, although everything depends on timely, high-quality treatment, a set of rehabilitation measures and the desire of the patient.
At the Yusupov Hospital, experienced neurologists diagnose and treat major strokes. For this purpose, modern medical equipment is used. It allows you to quickly and accurately determine the localization of the pathological focus. Based on the data obtained, doctors develop appropriate treatment. For this purpose, all conditions have been created in the neurology department:
- modern diagnostic equipment that allows you to quickly identify the type and location of a stroke and the degree of brain damage;
- a team of specialists, which includes professors and neurologists of the highest category with experience in treating major strokes;
- the presence of high-class life-support equipment that supports the vital functions of the body;
- modern effective drugs;
- the desire of all clinic staff to give the patient a chance to recover after a stroke;
- the use of innovative methods for restoring lost functions by rehabilitation clinic specialists;
- the possibility of performing minimally invasive neurosurgical interventions in partner clinics;
- psychological support for relatives of patients who have had a major stroke.
What is a major stroke
In the international classification of diseases ICD-10, acute cerebrovascular accident is coded I60-I69. A major stroke is the most dangerous type of cerebral blood flow disorder, leading to the death of several areas of the brain. The term “extensive” is due to several characteristics:
- large areas of the brain are affected;
- the formation of the disease is caused by damage to large arteries;
- the possibility of the appearance of many pathological foci.
Loss of oxygen and nutrients leads to rapid death of nerve cells. A large amount of damage during a major stroke leads to the loss of important functions and abilities of the body: vision, hearing, motor activity, etc. The consequences of minor injuries with quick and effective treatment can be completely eliminated, which allows the patient to return to normal life and restore lost functions, but the likelihood of recovery for large lesions is quite small.
Extensive lesions are characterized by a high rate of development of clinical signs, severity and the development of serious irreversible consequences, so the prognosis for the patient is rather disappointing. According to statistics, approximately 15-20% of victims have a chance of recovery.
Left hemisphere stroke: medical assistance
Therapy during the recovery period after a stroke includes several areas:
- drug treatment (aimed at eliminating blood clots in blood vessels, expanding the lumen of blood vessels, as well as alleviating the patient’s depressive conditions, etc.);
- physiotherapeutic procedures;
- physiotherapy;
- speech therapy classes;
- massage for stroke on the left side of the brain.
A brain stroke on the left side may cause the need to organize special classes to correct the patient’s psychological state and develop his desire to carry out all the necessary medical procedures.
Mandatory are: adherence to a daily routine, proper nutrition, and ensuring the patient’s physical activity.
The complex of restoration measures necessarily includes basic housework, which not only restores the functions of organs and systems, but also normalizes a person’s psychological state.
Stroke is a serious illness. Damage to the left side of the brain changes the patient’s life, putting him in a position where he has to relearn how to speak, walk, and work with his hands. However, the help of specialists and a person’s desire to normalize his condition help to treat him and achieve good results.
Paralysis of the left side does not require as much time as the right side to restore vital functions. Medical practice shows that a stroke on the left side brings less dangerous consequences, and patients seeking to recover have greater opportunities to deal with severe complications.
Symptoms, clinical picture
Precursors of a stroke may appear weeks and even months before an acute cerebrovascular accident. Among the obvious first symptoms of a stroke are:
- dizziness;
- headache;
- darkening of the eyes with sudden movements;
- episodic global memory loss (amnesia);
- sudden short-term disorientation.
The main signs of a major stroke appear several hours before an acute cerebrovascular accident or directly during an attack. Depending on the type of stroke, within a day the patient experiences pronounced symptoms of brain damage:
- drowsiness followed by excitement;
- stunned;
- loss of consciousness;
- increasing sharp headache;
- nausea and vomiting.
Patients are concerned about pain in the eyeballs, a feeling of heat, sweating, increased heartbeat, dry mouth, and convulsive syndrome develops. One of the most common symptoms of a major stroke is coma. It indicates significant and deep damage to brain structures. After treatment and rehabilitation at the Yusupov Hospital, 37% of patients who suffered a stroke live a full life, 25% regain consciousness, but there remain residual disturbances in speech and motor functions, which are also gradually corrected in the rehabilitation clinic.
General cerebral symptoms of a major stroke include:
- Strong headache;
- loss of consciousness;
- dizziness;
- stunned state;
- sopor;
- rarely coma;
- pale skin;
- cardiopalmus;
- nausea;
- vomit;
- convulsive syndrome;
- hyperthermia.
Focal symptoms depend on the location of the pathological focus. When the right hemisphere is damaged, motor and sensory disorders occur in the left half of the body, and vice versa. Among the main symptoms are:
- violation of superficial and deep sensitivity;
- inability to independently flex and straighten limbs;
- drooping corner of the mouth;
- inability to smile;
- impaired speech and swallowing;
- deviation of the tongue towards the affected side;
- memory loss;
- mental disorder;
- decreased visual acuity;
- dry mouth.
Doctors at the Yusupov Hospital pay special attention to the symptoms of a major stroke. The clinical picture, together with the diagnosis, allows us to determine the type of cerebrovascular accident and prescribe appropriate treatment.
Rehabilitation
If a coma develops after a stroke, what should the patient’s relatives expect?
Rehabilitation of a patient who has suffered a stroke is of great importance. Poor blood circulation in the brain causes many pathologies, and only full compliance with the rules protects against relapse and improves the patient’s condition.
Particular attention should be paid to the diet. It should consist only of healthy foods and contain the maximum amount of vegetables and fruits
It is advisable to purchase an orthopedic mattress, even if motor functions are relatively normal. If they are violated, you need to ensure that the patient’s position changes regularly so as not to provoke the appearance of bedsores.
Doctors often prescribe diuretics to help cope with leg swelling, a problem that often plagues patients after a stroke. If there are signs of aggression or, conversely, apathy, it is necessary to involve a psychologist. His help will be needed not only by the patient, but also by those who care for him.
Causes
Major stroke has several risk factors:
- Atherosclerosis. Reducing the lumen of the arteries due to cholesterol deposits disrupts the process of blood circulation in the tissues of the brain. This provokes the development of ischemia;
- Hereditary predisposition. If one of the relatives had a history of an episode of cerebrovascular accident, then subsequent generations are at risk;
- Taking certain medications. Oral contraceptives and other drugs thicken the blood, increasing the risk of spontaneous thrombosis;
- Arterial hypertension. High blood pressure has a strong impact on the vascular wall. As a result, arteries rupture with subsequent hemorrhage into the brain cavity;
- Frequent transient ischemic attacks;
- Diabetes mellitus complicated by cerebral vascular angiopathy;
- Asymptomatic carotid artery stenosis;
- Smoking and alcohol abuse;
- Drug use;
- Metabolic syndrome;
- Excess weight (more than 30% of normal).
The chances of surviving a major stroke depend on whether treatment for the disease is started within 3-4 hours of the onset of the first symptoms. Finding out the causes of major stroke is necessary to develop the most effective treatment regimen. In addition, eliminating provoking factors will reduce the risk of developing a recurrent cerebrovascular accident.
A major stroke is one of the most dangerous pathologies that occurs due to circulatory problems in several areas of the brain at once. As a result, the patient develops a number of complex pathological abnormalities, in some cases incompatible with life.
The most dangerous type is considered to be hemorrhagic stroke. In this case, problems arise with blood circulation in the brain, leading to hemorrhages. Blood entering the cranial cavity causes swelling of the surrounding tissues, as a result of which vital functions are disrupted. Ischemic stroke has favorable prospects. It is expressed in a short-term disruption of vascular conductivity, which, with proper therapy and care, is eliminated over a certain period of time.
The symptoms of a major stroke are characteristic: the patient loses coordination, inadequately perceives reality and the speech of others, completely or partially loses the ability to reproduce words and arrange them in logical chains. The main symptom is a severe headache.
If any of these manifestations occur, you should immediately consult a doctor. The sooner measures are taken, the greater the chances of recovery, and in some cases, life. The consequences of a major stroke are truly dangerous; most patients cannot fully recover their health for the rest of their lives. At the Yusupov Hospital, the examination takes minimal time, and a comprehensive treatment plan is prescribed in accordance with the type of extensive stroke and the extent of brain damage.
Make an appointment
Dementia
Complete rehabilitation after a stroke at home: what complex will help the patient?
Symptoms of stroke and the consequences of severe brain damage (especially in repeated cases) are an important risk factor for the development of cognitive deficits and dementia. Vascular dementia is diagnosed based on the development of multiple cognitive impairments, manifested by memory impairment and at least one of the following disorders:
- aphasia;
- apraxia;
- agnosia;
- impairment of executive functions in the presence of focal neurological symptoms.
Various scales have been developed to assess dementia, such as the MMSE (Mini-Mental State Examination). Scores of less than 24 out of a possible 30 points indicate the presence of dementia.
The Dementia Score (DS) is the most developed scale for assessing symptoms of dementia. Through 23 items, changes in a person's performance and habits in daily activities are detected. The higher the score, the higher the severity of dementia.
Kinds
Acute cerebrovascular accidents are divided into ischemic and hemorrhagic. In the first case, the lumen of the artery closes, in the second, blood escapes from the damaged vessel. Various reasons lead to the development of these types of stroke. In addition, they differ in pathogenetic mechanisms and clinical presentation. Extensive stroke is divided into the following types:
- Hemodynamic. Vasospasm provokes a decrease in the amount of oxygen that reaches the brain tissue. The cause of this condition is often hypotension.
- Microocclusion. A stroke develops due to a local disturbance in blood flow.
- Lacunar. In the brain, due to increased pressure in the vessel, a cavity is formed. It is filled with liquid.
- Cardioembolic. Arrhythmias lead to the detachment of a blood clot. As a result of uneven contraction of the myocardium, blood turbulence occurs. The detached blood clot enters the brain vessel, causing the development of a stroke.
- Atherothrombotic. The cause of acute cerebrovascular accident is the blocking of the artery lumen by an atherosclerotic plaque. Atherosclerosis is formed due to changes in the lipid composition of the blood.
Mechanism of ischemic stroke
Another name for ischemia is cerebral infarction. As a result of a sharp restriction of blood supply, brain tissue dies. This condition often occurs due to rupture of an atherosclerotic plaque, blockage of the lumen of a vessel by an embolus or thrombus.
The cause of atherosclerosis is the deposition of cholesterol in the inner layer of the artery. A blood clot forms due to increased blood viscosity. This condition often occurs against the background of concomitant diabetes mellitus and tumor formations. A cerebral infarction develops due to a sudden cessation of blood flow to the brain tissue. The changes that occur become irreversible 5–8 minutes after the onset of pathological symptoms. In the absence of correct treatment, the affected area increases. Therefore, it is important to seek medical help in time to preserve as much viable tissue as possible.
With the development of ischemic stroke of the left hemisphere, sensory disturbances and motor disorders appear on the right. Damage to the right hemisphere is accompanied by speech disorders. General cerebral symptoms include dizziness, nausea, loss of consciousness, and in rare cases, coma. Specific signs of ischemic stroke are considered to be a decrease or complete loss of sensitivity in the right half of the body, limited or absent movements in the limbs, problems with swallowing, and drooping of the corner of the mouth.
Ischemic stroke is divided into 5 subtypes:
- atherothrombotic – develops slowly due to atherosclerosis of the cerebral arteries;
- cardioembolic – occurs when a cerebral artery is completely or partially blocked and develops rapidly;
- lacunar – occurs due to damage to perforating arteries, develops within several hours;
- hemodynamic – occurs due to a sharp decrease in blood pressure, is sudden, affects all areas of the blood supply;
- microocclusive - develops due to a violation of the coagulation and anticoagulation system.
Determination of severity
Depending on the area of damage to the brain tissue, there are 3 degrees of stroke severity:
- Easy. The man experiences mild neurological symptoms: headache, unilateral decreased sensitivity, etc. Consciousness is preserved. Signs of pathology are insignificant and this makes diagnosis difficult - symptoms are mistaken for manifestations of other diseases. Without timely treatment, ischemia progresses and the patient's condition worsens.
- Average. Motor activity decreases, coordination is impaired, and speech is difficult. Consciousness is preserved or the patient is in a state of stupor.
- Heavy. The man is unconscious, facial asymmetry is visible outwardly, and involuntary urination appears. Seizures may develop. In severe cases, death often occurs.
IT IS IMPORTANT TO KNOW!
By timely assessing the severity, you can save a human life. There is no need to be afraid to call a doctor, even if you have doubts about the nature of the disease. Timely assistance will improve the prognosis of treatment of the disease.
Mechanism of hemorrhagic stroke
Among the main causes of hemorrhagic stroke are:
- uncontrolled arterial hypertension;
- excessively thin blood;
- congenital deformations of the vascular wall.
Rupture of blood vessels with subsequent leakage of blood into the brain cavity most often provokes a sharp rise in blood pressure. In addition to the listed etiological factors, aneurysm, traumatic brain injury, physical or emotional stress can cause hemorrhagic stroke.
Hemorrhagic stroke is characterized by a sudden and rapid onset. Symptoms include severe headache, rapid breathing, confusion, and possible development of coma. The skin becomes cold to the touch, the corner of the mouth droops, and blood pressure rises. Against the background of hemorrhage in the brain, the tone of the muscles of the limbs decreases, strabismus may appear, the pupils dilate, and swallowing is impaired. Hemorrhagic stroke has a less favorable course and is often accompanied by complications.
There are 2 types of hemorrhagic stroke:
- intracerebral. Occurs due to thinning of the arterial walls and a sharp jump in pressure. The risk group includes persons aged 45 to 60 years;
- subarachnoid. Occurs when a cerebral artery aneurysm ruptures and blood escapes under the arachnoid membrane of the brain. The risk group consists of people aged 30-60 years, abusing alcohol and smoking, and having excess body weight.
How long do they live after a stroke: statistics in detail
The life expectancy of a person after a stroke is highly individual. In 20% of cases, a person’s death occurs instantly.
Studies have shown that in the first 30 days the mortality rate is 30-40%; after the first year after a stroke, approximately 50% of patients die.
The repeated process of cerebral circulatory disturbance increases the possibility of death. Often, if a patient has a first stroke, he can live up to 10 years, but with a second attack on the brain, life expectancy is no more than 3 years.
The reason for such a high mortality rate after a second stroke is that after the first attack, lesions remain in the brain.
Dependence on age and gender
With hemorrhage before 40 years of age, the death rate is 15%, after 50 years of age – 45% of cases.
Women have a higher mortality rate than men – 39% versus 29%.
It is several times more difficult for newborns and people aged 65 years and above to survive a stroke. This is due to age-related factors in blood vessels and their walls, which cannot recover quickly. In newborns, the cells have not yet formed. Such wall problems lead to:
Lesion size
This is the main aspect that affects how long a person can live after a stroke. Tissues susceptible to necrosis take a long time to recover.
The larger the affected area, the worse the prognosis.
How consequences affect the outcome
If after a stroke the patient begins to develop concomitant pathologies (paralysis, numbness or impaired psychological functions), then life expectancy decreases several times.
In addition, these consequences create the preconditions for the occurrence of bedsores. Bedsores form irreparable processes in the blood circulation of the whole body. Mental disorders require round-the-clock care for the patient, since he is not able to soberly assess the situation and take medications on time.
Life expectancy without movement
A person who is immobilized after an attack does not have the necessary desire for long-term recovery. Because of this psychological feature, a person does not strive to adhere to all norms and procedures, which is why muscle endurance decreases, fibers lose tone, and blood flow in the limbs is disrupted.
This ultimately leads to blood clots and tissue necrosis, which poison the blood.
Diagnostics
Major stroke is a condition requiring urgent diagnosis and treatment. For this, the Yusupov Hospital uses the following methods:
- Collection of complaints and medical history. The doctor finds out the time of onset of pathological symptoms, their severity and speed of spread. It is necessary to establish predisposing factors.
- Measurement of blood pressure and heart rate. These are indicators by which the severity of the patient’s condition is assessed.
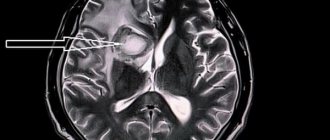
- MRI. Allows visualization of cerebral tissue. Today, tomography is considered the most informative method for diagnosing acute cerebrovascular accident.
- EEG. Evaluates brain activity. In the affected area, the waves received will be below normal.
- Doppler ultrasound of the vessels of the head and neck. It is carried out to determine the nature of blood flow in the brain area.
- Clinical and biochemical blood test. Prescribed to detect cholesterol concentrations. The standard of research includes a lipid profile.
The listed diagnostic methods can be expanded depending on the individual characteristics of the disease. The Yusupov Hospital uses modern medical equipment for examinations. Thanks to this, it is possible to quickly and accurately determine the pathological focus. Based on the data obtained, neurologists select a treatment and rehabilitation program for each patient. This approach allows you to reduce the length of hospital stay and minimize the risk of complications and recurrent stroke.
Make an appointment
Key risks and consequences for men
A transient ischemic attack or microstroke ends in complete restoration of function if neurological symptoms were present for no longer than a few minutes. When an attack lasts several hours, consequences are possible in the form of weakness of the limbs, speech disorders, memory, reaction speed, and coordination problems.
TIA severity criteria indicate the likely risk of another attack, which may result in a stroke.
| Criteria | Indicators | Point |
| Hell | More than 140/90 | 1 point |
| Age | Over 60 years | 1 point |
| Clinic | Weakness in the arm/leg during an attack | 2 points |
| Speech Impairment | 1 point | |
| Other symptoms | 0 points | |
| Duration of attack | 60 minutes | 2 points |
| From 10 minutes to an hour | 1 point | |
| Less than 10 minutes | 0 points | |
| Diabetes | Eat | 1 point |
Criteria for evaluation:
- With 3 points scored, men remain at low risk of a second attack;
- At 4-5 average;
- At 6 and above, the patient is considered to be at high risk.
Patients at medium and high risk are subject to clinical observation for a year after the attack. They also need to undergo a full range of examinations, if it was not performed in a hospital (general and biochemical blood tests, coagulogram, MRI, ultrasound scanning of the heart and extracranial vessels, ECG or Holter). Mandatory correction of risk factors (BP, DM, cholesterol) and treatment of concomitant pathologies.
Differences in consequences between men and women
| Criterion | Sex difference |
| Probability of recurrent attacks | Men have higher |
| Mortality from strokes | Men have higher |
| Rehabilitation after an attack | It goes faster in men |
| Likely consequences of the attack | Expressed in females |
Treatment
Treatment for a major stroke should begin as early as possible. Irreversible consequences for the brain develop rapidly. To prevent stroke complications, comprehensive treatment is necessary. Self-therapy is excluded. The patient needs to be urgently hospitalized. The following drugs are used to treat major stroke:
- Hypotensive. Prescribed to lower blood pressure. In inpatient settings, antihypertensive therapy is emergency. In the future, a permanent treatment regimen is selected for the patient.
- Anticoagulants. Prevents thrombus formation and improves the rheological properties of blood.
- Diuretics. Against the background of a major stroke, the risk of developing cerebral edema increases. It occurs due to an increase in the amount of cerebrospinal fluid in certain areas. Diuretics help remove excess fluid from the body and alleviate the condition.
- Statins. Prescribed to reduce blood cholesterol levels, as well as prevent the development of atherosclerosis.
- Angioprotectors. Protect the vascular wall from the exogenous effects of provoking factors.
- Cerebrovascular drugs. Improves blood circulation in the brain and restores metabolic processes.
Surgery for stroke is indicated in the presence of an extensive hematoma. The purpose of the operation is to remove liquid connective tissue. This is necessary to reduce the risk of developing compression of healthy nerve structures. The surgical operation is performed through trepanation.
After treatment and relief of the acute period, patients are transferred to the rehabilitation period. At the Yusupov Hospital, experienced exercise therapy instructors and physiotherapists develop an individual rehabilitation treatment plan.
Stroke is getting younger, but we are not
Khripun: Rehabilitation is expensive, but for Russians it is free
“It is traditionally believed that the risk of stroke increases with age, and this is true,” explains Professor, Director of the Research Institute of Cerebrovascular Pathology and Stroke of the Russian National Research Medical University named after. N.I. Pirogova Lyudmila Stakhovskaya. “But today this is no longer the “prerogative” of elderly patients; today we are talking about stroke rejuvenation. It ceases to be an age-related problem and occurs in young and apparently absolutely healthy people.”
It would seem that there is nothing complicated: adjust your diet, normalize your work and rest schedule, move more, quit smoking, get regular examinations, take simple tests for cholesterol and blood sugar (glucose) levels, monitor your blood pressure. But, as opinion polls show, Russians are characterized by careless behavior. Most people begin to “monitor” their health when it is already running low. This majority would do well to watch Julian Schnabel's poignant film The Diving Bell and the Butterfly, based on real events. The editor of the French magazine Elle, Jean-Dominique Bobby, is a young, successful, super-rich member of the elite - and suddenly - an unexpected stroke, right while driving. And there was no one nearby who would quickly help. The hero survived, but was completely paralyzed. Only the left eye remained “alive”. It’s hard to believe, but in the last month of his life, Bobby managed to “dictate” a book about how he felt - the assistant slowly named the letters, and when she reached the right one, Bobby closed his only eye. In fact, a film was made based on this book, which won many international awards.
Test
Last year, the American Heart Association and the American College of Cardiology lowered the blood pressure levels at which a patient is diagnosed with hypertension. Now normal pressure is considered to be no higher than 120/80 mm Hg. Art. At 130/80, cardiologists talk about “high” blood pressure. And with numbers above this level, a diagnosis of hypertension is made. Up to a level of 140/90 we are talking about stage I hypertension; if this indicator is exceeded, stage II is diagnosed. If the indicators reach 180/90 (and at least one of the two) - we are talking about a hypertensive crisis. In this case, the recommendations say, you should immediately seek medical help.
How to help before the doctor arrives
Before the ambulance arrives, the person needs to be provided with complete rest, an influx of fresh air, and not given any medications or food. Ask your neighbors to meet the ambulance (there have been cases when the team could not drive up to the house due to a barrier or an incorrectly dictated address). Every moment is precious: answer doctors’ questions clearly and quickly, prepare the patient’s documents and insurance policy in advance.
Infographics "RG": Mikhail Shipov/Leonid Kuleshov/Irina Nevinnaya
Consequences
It is impossible to accurately predict the consequences of a major stroke. It all depends on the volume and location of the damage. The human body is designed in such a way that when one hemisphere loses activity, the other is activated, which allows one to maintain vital functions and increase the chances of survival. With such a severe form of pathology, persistent disorders often develop that are difficult to correct:
- paralysis of limbs;
- muscle hypertonicity;
- inability to self-service;
- mental disorders;
- loss of vision;
- memory disorders;
- loss of learning ability;
- speech impairment, etc.
A major stroke is characterized by an unfavorable course. Untimely treatment can lead to the development of incurable complications. The disease occupies a leading position in the structure of disability. The most common consequences of a major stroke include:
- Movement disorders. Such complications occur in 80% of cases. In this case, the ability to move the upper or lower extremities is impaired or completely lost;
- Speech disorders. Doctors identify several options for speech complications;
- The ability to speak and write independently is lost, but the speech of the interlocutor is perceived adequately;
- There is a loss of perception of one’s own and others’ speech;
- Visual impairment. The image may be completely distorted or partially missing.
- Cerebellar dysfunction. Characterized by dizziness at rest. In this case, causeless and uncontrolled vomiting, increased blood pressure and tachycardia occur.
To help patients with a major stroke, doctors at the Yusupov Hospital begin treatment and rehabilitation immediately after the patient’s admission to the neurology clinic. First, the vital functions of the body are ensured with the help of modern equipment that allows you to control breathing and cardiac activity. Then the type of stroke is clarified and drugs are prescribed that restore the function of brain cells in the stroke area and neurons located around the lesion.
In case of hemorrhagic stroke, patients at partner clinics undergo minimally invasive neurosurgical operations to reduce compression of the brain. This is the only effective treatment for hemorrhagic stroke and helps patients recover and regain lost functions.
In the presence of extensive ischemic stroke, pathogenetic therapy is carried out, aimed at improving the passage of blood through brain tissue, and treatment with neuroprotectors that protect brain cells from damage. Treatment begins within three hours of the onset of the stroke. The severity of the positive dynamics depends on the speed of dissolution of the blood clot: neurological functions are better restored with rapid, almost instantaneous lysis of the blood clot. The most rapid and complete dissolution occurs in cardioembolic major stroke. Slow restoration of blood flow occurs with atherothrombotic damage to the artery.
It is not accompanied by a significant improvement in clinical dynamics. For most blockages of medium- and large-sized arteries, thrombolysis is the treatment of choice. It provides early restoration of blood flow in 30-40% of cases. At the Yusupov Hospital, doctors use the most effective drug for thrombolysis - recombinant tissue plasminogen activator. It is administered intravenously to patients.
One of the promising directions for restoring blood flow through a thrombosed artery is surgical removal of the thrombus - endovascular extraction or excision. The operation is performed in partner clinics. After surgery, blood supply to the brain is restored in 81% of patients within the first 24 hours. In the first days of atherothrombotic stroke and with confirmed cardiogenic stroke, patients are administered heparin. In the presence of atrial fibrillation, after heart valve replacement or concomitant myocardial infarction, patients are prescribed warfarin.
Drugs with complex vascular-metabolic action, of which Cavinton is a representative, have a positive effect on the state of blood supply to the brain. In cases of extensive stroke, drugs that have a nootropic effect, as well as neuroprotectors, are prescribed. Rehabilitation of patients with a major stroke after restoration of consciousness is carried out in a rehabilitation clinic. The hospital is equipped with modern equipment, and a multidisciplinary team of specialists takes an individual approach to the treatment of each patient. If you have symptoms of a major stroke, call an ambulance and call.
When the patient arrives at the Yusupov Hospital, doctors will be ready to immediately begin providing specialized medical care that promotes recovery after a stroke. You can increase your chances of survival and reduce the consequences of a major stroke using rehabilitation techniques. You can get diagnosed and treated for a major stroke at the Yusupov Hospital. The clinic has modern medical equipment and a professional team of doctors. This allows for timely and high-quality treatment of cerebrovascular accidents.
Each patient is provided with an individual approach. Rehabilitation is carried out by experienced exercise therapy instructors. You can sign up for a consultation and ask any questions you may have by phone.
Introduction to induced coma
The message that a medical coma has been performed often frightens the patient's relatives. But an artificial coma during a stroke is necessary to reduce the load on brain tissue and ensure:
- connection of surviving brain cells with processes to create new neural chains;
- redistribution of brain functions (surviving structures begin the work of dead cells).
The relatives of the stroke patient are explained in detail why they are put into an artificial coma and they are told what consequences the artificially induced comatose process can prevent:
- after a stroke with hemorrhage, the pressure of the hematomas decreases and the risk of re-hemorrhage decreases;
- during an ischemic attack, it is possible to achieve a redistribution of cerebral blood flow and reduce the focus of necrosis.
While the patient is unconscious and does not respond to stimuli, the brain recovers faster from the attack.
Doctors decide individually how many days the artificially induced condition lasts, assessing recovery processes using CT and monitoring the patient’s vital functions. Sometimes treatment takes several weeks, which the person spends in intensive care under the supervision of staff.
The duration of recovery from drug-induced coma depends on the effect of the drugs. After the drugs are no longer administered, the reaction to external stimuli gradually returns, consciousness and the ability to move consciously appear.
Consequences of damage to the cerebral hemispheres
Based on the developing symptoms of a stroke, one can assume the localization of the damage. With a major stroke, the blood supply to one of the hemispheres is often disrupted, which makes it possible to predict possible consequences. The left hemisphere is responsible for analytical and logical functions, verbal communication. After damage to this area of the brain, problems with speech and pronunciation are likely to develop, loss of the ability to analyze events, loss of visual memory, decreased sensitivity of the right half of the body, psycho-emotional disorders, aggression, apathy, and reluctance to live. According to studies, it turned out that damage to the left hemisphere is less life-threatening, and the chances of recovery are quite high if you provide timely assistance and undergo full rehabilitation.
The right hemisphere is responsible for the perception of surrounding information and thinking, therefore, when it is damaged, the following complications develop: memory impairment (up to loss of short-term memory), motor disorders of the left half of the body, mental disorders, aggressiveness, increased excitability, disorders of the perception of space and time. Rehabilitation for such disorders can last several years, and the likelihood of returning even a small proportion of lost functions is low.
Move!
— How to choose the right physical activity after a stroke?
— It is necessary to move regardless of the degree of impairment after a stroke, with any degree of limitation.
If the functions of your legs and arms are not impaired, get up and start moving as quickly as possible! Do physical therapy, take the stairs instead of the elevator, walk down the street, garden, play with your grandchildren. Any activity that you enjoy is fine—just make a commitment to move every day.
If there is weakness in the limbs, but they work, you can walk, including on a treadmill, it is useful to swim, do gymnastics in the pool, yoga, and dancing.
Even if the patient is in bed or in a wheelchair, he can also move - do strength exercises, stretching exercises.
— Can a person always return to normal life after a stroke?
“It depends on the volume of damaged cells, what part of the brain is affected and whether medical assistance was provided on time. With due persistence, patience, and the help of doctors and relatives, lost functions are restored.
In my practice, there were patients who returned to work even after several strokes.
Both the patient and his family need to understand that recovery is a long and complex process; one should not expect instant results and fall into despair when they do not exist. There will be good days when you make huge strides, and bad days when you seem to have slipped back to where you started. Don’t strive to embrace the immensity, don’t rush things, but divide your goals into:
- the nearest ones - which can be tracked and measured. For example, if the patient was lying down in the first days, the immediate goal would be to sit up in bed and eat on his own. Holding a mug, getting up and walking to the door of the room, doing hygiene procedures - all these are also immediate goals.
- distant - what you want to achieve in 6 months or more. Return to work, sports, hobbies - it is better to discuss all these goals with your doctor to understand what degree of functional restoration you can expect.
Prevention
To reduce the risk of developing a recurrent major stroke, you must follow the preventive recommendations:
- Monitor blood pressure levels daily;
- to live an active lifestyle;
- avoid psycho-emotional stress;
- control weight;
- adhere to the principles of rational and balanced nutrition;
- carry out planned surgical correction in the presence of congenital aneurysms.
Recovery
In order for the patient’s recovery to be more effective, it is important to observe regularity when carrying out rehabilitation measures. To regain lost functions, you may need the help of a physical therapist and speech therapist. Therapeutic gymnastics can improve motor skills.
It is important to monitor a person’s mental state. Patients who have had a third stroke are at high risk of developing post-stroke depression. This should not be allowed, since people with depression are less responsive to rehabilitation and have a higher risk of death than patients without mental disorders.
Odds and Predictions
According to statistics, with major strokes the chances of survival are no more than 65-70%. At the same time, the majority of patients (80%) develop persistent irreversible disorders leading to disability; only in 5% of cases is there a possibility of complete recovery. In addition, 15% of patients develop a recurrent attack, worsening any prognosis, often leading to death. The chances of survival after a major stroke depend on many factors. The older the patient, the worse the prognosis, which is associated with the speed of metabolic processes and the presence of concomitant pathology. Bad habits also adversely affect the recovery of patients. Life expectancy and prognosis directly depend on the speed and quality of care.
If you suspect a stroke, you can contact specialists at the Yusupov Hospital. They organize emergency hospitalization of the patient in a specialized department, where the patient will receive emergency care and create an effective rehabilitation program. Rehabilitation after a major stroke includes a set of measures in accordance with age, indications and contraindications. The success of the procedures depends on the attitude of the patients, the active support of family and friends, and the implementation of all medical recommendations. The coordinated work of professionals at the Yusupov Hospital allows us to achieve excellent results that improve the quality and length of life. You can find out more about the treatment and rehabilitation of patients after a stroke by phone.
Make an appointment
Prognosis of patients after a stroke
The prognosis of patients after a stroke depends greatly on the type of condition, location, extent, age and other associated disorders, especially heart and vascular disease. This phenomenon is characterized by repetitions, which are facilitated by the mentioned cardiovascular diseases. These include:
- hypertension;
- narrowing of the arteries (atherosclerosis);
- heart disease (atrial fibrillation);
- other high-risk diseases (diabetes, hyperlipidemia, obesity).
The cause of repeated cerebral infarction may be a congenital vascular anomaly. Smoking also poses a great risk, both in younger and older people.
With a recurrent stroke, the prognosis for life in old age worsens.