Spinal osteochondrosis is a degenerative-dystrophic process that results in damage to the cartilaginous segments of the spine (intervertebral discs) with subsequent involvement of other parts of the spinal segment in the process. Due to greater mobility in the cervical region compared to other parts of the spine and a weak muscular frame, cervical osteochondrosis is observed very often - in more than 25% of cases. And headache is one of the most common manifestations of this disease.
Clinical picture of cervical osteochondrosis
The degree of severity and nature of symptoms in cervical osteochondrosis depends on the stage of the degenerative-dystrophic process, as well as on the location of the lesion. It should be noted that there is no specific clinic for cervical osteochondrosis; the main manifestations of the disease are pain and loss of sensitivity in the neck, back of the head, shoulder girdle, arms and fingers.
Cervical osteochondrosis is almost always accompanied by headaches (cephalgia), cervicalgia (pain in the neck, radiating to the back of the head, shoulder and arms), limited mobility of the upper spine (neck and shoulder girdle), and dizziness. Depending on the damage to a particular spinal segment, headaches may be observed in different localizations, combined with numbness, short-term or long-term loss of sensation in the shoulder and arms, down to the fingers.
Why is cervical osteochondrosis accompanied by headaches and dizziness?
Headaches are a very common complaint with cervical osteochondrosis. It is often accompanied by symptoms such as dizziness, poor coordination, and blurred vision. Let's consider how changes in the spinal column during cervical osteochondrosis lead to similar symptoms.
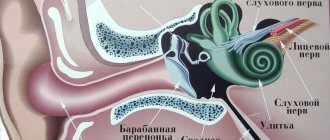
In the transverse processes from the VI to II cervical vertebrae there are canals through which the vertebral arteries pass, supplying blood to many parts of the brain and the so-called “Frank’s nerve”. Due to degenerative changes in the joints of the spine and directly in the vertebrae, the formation of osteophytes (bone growths) occurs, which leads to a narrowing of the spinal canal and compression of elements of the neurovascular system.
Osteophytes directed to the muscles irritate them, this causes a reflex muscle spasm, which leads to compression of the intervertebral discs, aggravating the course of the disease. Osteophytes, irritating the nerve roots at the exit of the spinal column, cause pain and spasms, the localization of which depends on the affected area.
Osteophytes directed to the canal of the transverse processes irritate Frank's sympathetic nerve, which leads to spasm of the vertebral artery, and also mechanically compress this artery, provoking a violation of cerebral circulation.
An acute disturbance of cerebral hemodynamics (brain circulation) leads to the development of an ischemic attack of the brain, which leads to the appearance of symptoms of cervical osteochondrosis such as dizziness, nausea, headache, loss of coordination, and blurred vision.
Another reason for compression of the Frank nerve and the vertebral artery is displacement of the disc in the posterolateral and lateral directions, protrusion of the disc into the intervertebral canal during a hernia or protrusion (protrusion of the disc without violating its integrity).
The cause of compression of the nervous and vascular structures in the cervical spine can also be subluxation of the cervical vertebrae, their confusion relative to their natural position.
In addition, muscle spasm caused by psycho-emotional fatigue, excessive physical exertion or an uncomfortable position during sleep also leads to poor circulation in the cervical region and, as a consequence, headaches and dizziness.
What is a cluster headache?
Headache, or cephalgia, is a common companion in life in both adults and children. It turns out that experts distinguish several types of cephalgia, differing from each other both in the causes of occurrence and in the tactics of getting rid of it. Daria Vasilievna Kunitsyna, a neurologist at Clinic Expert Stavropol, told us about one of them – cluster headaches, the peculiarities of its manifestation, diagnostic methods and treatment methods.
- Daria Vasilievna, what does “cluster headache” mean?
Cluster headache (or, otherwise, cluster headache) is a type of headache of a paroxysmal nature with a pronounced pain syndrome of clear localization. With cluster cephalgia, a person experiences repeated attacks of intense throbbing pain in the eye sockets, periorbital region and temples.
This is a fairly rare pathology, affecting approximately 5% of the entire population.
-What are the causes of cluster headache?
Typically, the cause of this type of headache is a violation of circadian rhythms - cyclical fluctuations in the intensity of various biological processes in the body, which are caused by the change of day and night. A special anatomical structure in the brain - the hypothalamus - is responsible for the continuity of these rhythms.
Pathologies of the hypothalamic-pituitary system, damage to the reticular formation, spasm of cerebral vessels, diseases of the sympathetic nervous system can provoke the development of cluster headaches.
Cluster headaches are more common in men (20 to 50 years of age) than women (5:1 ratio) and in overweight individuals
- Are there risk groups that are more susceptible to this pathology?
Eat. Cluster headaches occur more often in people who:
— are exposed to frequent changes in time zones (due to moving, traveling);
— violate the work and rest schedule;
- abuse alcohol and smoking;
- use certain medications - in particular, nitroglycerin and histamine.
I would like to note the fact that this pathology is more common in men (from 20 to 50 years old) than in women (in a ratio of 5:1), as well as in overweight individuals.
Read materials on the topic:
Isn't it beer that kills people? Alcohol and the brain
What does fat have to do with it or why do people gain weight?
-What characteristic symptoms can be used to recognize a cluster headache?
The peculiarity of this type of cephalgia is its sudden occurrence against the background of complete health, often at night, during sleep. The pain is clearly localized on one side of the head. Patients describe this pain as “unbearable, burning, throbbing.” During attacks, the patient freezes, as the slightest movements cause him severe pain.
Upon examination, you may note redness of the face due to dilated blood vessels, lacrimation, and increased salivation.
- Do children have cluster headaches? If so, how do they manifest themselves?
They happen, but extremely rarely. To differentiate it from other types of cephalgia that develop against the background of increased temperature in various diseases and intoxication of the body, a specialist should pay attention to the sudden onset of headache in the absence of other symptoms, its clear location (orbits, periorbital and temporal areas) and the nature of the sensations. Children describe this pain as “drilling.”
- How is cluster headache diagnosed?
First of all, we clarify the complaints and find out how the disease developed. In this case, attention should be paid to complaints of unilateral damage, characteristic areas of pain, attacks of high intensity pain that occur three to eight times during the day.
After this, a number of laboratory and instrumental research methods are prescribed. Traditional laboratory methods include a general blood test to exclude an inflammatory process, a coagulogram to determine blood clotting and exclude thrombus formation in the vessels of the brain, and a biochemical blood test to assess the concomitant pathology of internal organs.
Read more about blood tests in our articles:
How to properly take a general blood test?
What does a biochemical blood test show?
To visualize brain structures, magnetic resonance or computed tomography may be prescribed to exclude focal lesions, as well as MR angiography or Doppler ultrasound of the cerebral arteries to detect acute cerebrovascular accidents, hemorrhages, or blockage of blood vessels by blood clots.
Read materials on the topic:
If an MRI of the brain showed...
How will MRI of cerebral vessels help a patient?
When is ultrasound of cerebral vessels prescribed?
Consultations with related specialists may also be required - for example, an ophthalmologist who can conduct a fundus examination and measure intraocular pressure. You should consult a therapist to exclude somatic pathology, and a psychotherapist to differentiate cluster headaches from cephalgia in mental pathologies.
- Tell us how to get rid of cluster headaches?
There are two directions in the treatment of cluster headaches. Symptomatic treatment is aimed at eliminating the pain syndrome, and preventive treatment is aimed at reducing the frequency of subsequent exacerbations. Non-drug methods include oxygen inhalation.
As therapy, drugs from the ergotamine group are also prescribed to strengthen the vascular wall. For prolonged periods, hormonal therapy, antipsychotics, tranquilizers, and antidepressants are used. It is important to note that self-medication is inappropriate here, and any medications should be taken under the strict supervision of a doctor.
Unfortunately, it is currently impossible to completely cure this disease, but with supportive treatment, lasting positive results can be achieved.
-What are the dangers of cluster headache attacks?
High intensity of pain leads to asthenia (weakening) of the patient. Attacks and their anticipation can lead to the development of depressive and anxiety disorders. There are known cases of suicide attempts due to unbearable pain. Another danger is long-term use of medications to get rid of cluster cephalgia, which can harm other organs.
- Daria Vasilyevna, is it possible to prevent the development of this pain? If so, how?
Maintaining a healthy lifestyle, giving up bad habits, following a work-rest schedule, playing sports, walking, a balanced diet, reducing the number of stressful situations - these simple rules will help reduce the frequency of cluster headache attacks.
The editors recommend:
Medical horror stories. Myths and truth about migraines
Tension headache: causes, symptoms, diagnosis and treatment
Attack to the head. How to protect yourself from summer meningitis?
When the brain is inflamed: what is encephalitis?
MRI of the brain for prevention
For reference:
Kunitsyna Daria Vasilievna
In 2014 she graduated from Stavropol State Medical University with a degree in General Medicine.
In 2021, she completed her residency training in the specialty “Neurology” at the City Clinical Emergency Hospital of Stavropol.
Neurologist at the Expert Clinic, Stavropol. Receives at the address: st. Dovatortsev, 39A
Features of headaches in cervical osteochondrosis.
Headaches (cephalgia) with cervical osteochondrosis are usually of moderate intensity. Patients characterize the pain as dull, pulling, boring, pressing (feeling of squeezing of the head). Cephalgia with osteochondrosis is usually paroxysmal in nature (from several hours to several days).
Most often, the pain is one-sided, localized in the cervical-occipital region and spreads to the frontal and temporal regions.
Headaches with cervical osteochondrosis are often accompanied by:
- photophobia (intolerance to bright light);
- phonophobia (increased sensitivity to sounds, noise);
- feeling of stuffiness in the ear;
- complaints of blurred vision.
Stiffness in the cervical spine and muscle tension are often noted. Pain and stiffness depend on the position of the neck, and intensify with tension in the muscles of the affected side, or with prolonged stay in an uncomfortable position.
Headaches with cervical osteochondrosis are often combined with pain in the shoulder and arm.
Cephalgia
Cephalgia, also known as headache, is a fairly common nonspecific symptom of various diseases or pathological conditions, which is characterized by pain in the head, base of the neck, or the neck itself.
The brain itself cannot cause pain, since it does not contain pain receptors. Cephalgia occurs in one of the areas of the head: the skull (periosteum), muscles, nerves, arteries or veins, subcutaneous tissue, eyes, nose, mucous membranes. Then the nerve signals are transmitted to the corresponding part of the brain, recognized, and pain is projected from the pathological area to the brain.
The most common headaches encountered in medical practice are primary headaches (occurring on their own without any causative agent). They are of a specific nature, can be localized in a certain part of the head, have different durations, occur with a certain frequency, or arise completely unexpectedly. As a rule, such pain syndrome is well relieved by analgesic drugs and the patient rarely goes to a headache treatment clinic.
Secondary headaches occur against the background of another progressive disease, for example, meningitis, encephalitis, hypertension or hypertension, disorders of the neck muscles. treatment of headaches is always noted during and after skull injuries or concussions, as well as in pathologies and treatment of the cervical spine. These cephalgia have their own characteristics and are accompanied by other symptoms (dizziness, nausea, visual and auditory dysfunction, increased blood pressure, etc.).
Classification of cephalalgia according to pathogenetic characteristics
Doctors offer the following classification of headaches according to the etiology of their occurrence and symptoms:
- Vascular is the most common type of headache, the cause of which is a sharp excessive narrowing or dilatation of arteries and vessels, insufficient tone of the veins, brain hypoxia, and slowing of blood flow. It is observed in patients suffering from vegetative-vascular dystonia, hypertension (constant increase in blood pressure), hypotension (decreased pressure), weakened tone of the muscular walls of the veins, which do not have time to pump out the blood entering the brain.
Vascular cephalgia has a pulsating character, it compresses, there is a feeling of “knocking hammers” in the head, dizziness, and nausea. There are disturbances in coordination of movements, visual function (darkening, flashing of “butterflies” or “circles” before the eyes), pallor of the skin in hypotensive patients and redness in hypertensive patients.
- Vasomotor – associated with overstrain of muscle tissue and disruption of the passage of nerve impulses in neuromuscular clusters. It can occur after severe overwork of the muscles of the neck and head, shoulder girdle (long stay at the computer, eye strain when working with a microscope, etc.), during depression, after stress, overwork, prolonged lack of sleep, hypothermia.
It is characterized by a dull squeezing sensation in the frontal region or throughout the head, aggravated by physical activity, bright light and noise.
- Liquorodynamic pain is associated with an increase or decrease in intracranial pressure, as well as with a pathological change in the location of intracranial arteries (basilar, carotid, cerebral, vertebral arteries, circle of Willis, etc.) against the background of normal pressure inside the skull.
Bursting sensations coming from the depths of the head. They intensify with tension, changes in body position, sudden movements, dizziness, disturbances in gait, vision, and hearing are observed.
- Infectious-toxic - appears when viral microorganisms (influenza, encephalitis, meningitis, tuberculosis, etc.) enter the human body and the immune system begins to work almost immediately. As a result of this struggle, some cells of the body and the harmful pathogen die, begin to decompose, and release toxic substances that are carried through the blood throughout the body.
General intoxication causes severe cephalalgia, usually accompanied by fever, fever, and confusion.
- Neuralgic - provoked by irritation of nerve fibers by pathological processes of an internal or external nature, the formation of foci of pathological activity in the antinociceptive system (part of the nervous system responsible for pain relief). Attacks of pain are sharp, burning, acute, shooting (trigeminal neuralgia - intense shooting pain in the face, congestive processes in the optic nerve head).
If you have other “alarming” symptoms accompanying cephalgia (sleep disturbances, sudden temporary paralysis of the limbs, muscle weakness, blurred vision or loss of vision, pain in the eyeballs or hemorrhage), you should not waste time, but should immediately undergo a full medical examination at a headache center . Pain in the head area may indicate intracranial hemorrhage or stroke, hematoma or brain tumor, dislocation of the lower jaw or thrombosis of the dural sinuses of the brain and other diseases.
Diagnosis and treatment of cephalalgia
In most cases, primary headache is treated with analgesics or antispasmodics; patients do not attach much importance to it and rarely go to the hospital. Secondary cephalgia requires specific treatment, long-term observation of the patient, medical history and clinical trials. To identify foci of pathological activity and exclude neurotic etiology of pain, an electroencephalographic examination or CT scan without the use of a contrast agent is performed.
In almost all chronic, protracted and intense attacks of headache, brain tomography is indicated. If necessary, your doctor may order a lumbar puncture to examine the cerebrospinal fluid.
For frequently recurring pain, the cause of which has not been established, the patient is recommended to keep a diary, which will note the nature of the pain, intensity, accompanying symptoms, factors influencing the relief or aggravation of the condition. Chronic pain is relieved by complex treatment, which consists of medications and manual therapy sessions (acupuncture, acupuncture, relaxation therapy, massage, etc.).
Self-medication of cephalalgia and uncontrolled use of painkillers can lead to the occurrence of so-called medicinal headaches, thus forming a vicious circle in an attempt to cure the disease.
Author: K.M.N., Academician of the Russian Academy of Medical Sciences M.A. Bobyr
What can provoke increased headaches with cervical osteochondrosis
- Prolonged forced positioning of the body, especially while sitting at a computer or desk.
- Uncomfortable head position during sleep;
- Sudden head movements, especially rotational ones.
- Impacts, injuries.
- Incorrectly performed massage and other manual procedures.
- Excess weight puts more stress on the spine.
- Eating spicy and salty foods does not directly worsen the headache, but leads to disruption of metabolic processes, which aggravates the disease.
How to get rid of headaches with cervical osteochondrosis
To relieve headaches, including those with cervical osteochondrosis, analgesics in combination with antispasmodics help well. For severe muscle tension and irritation, nonsteroidal anti-inflammatory drugs (NSAIDs) can be used. However, it must be remembered that these drugs do not treat the underlying disease, providing only symptomatic care, and at the same time they have a number of serious side effects. Thus, analgesics and NSAIDs, including those containing diclofenac, suppress bone marrow function, lower immunity, inhibit gastric secretion, irritating its mucous membrane and provoking the development of gastritis, and reduce blood clotting. In addition, it has been proven that systematic or frequent use of diclofenac increases the risk of heart attack by 40%, and NSAIDs in general lead to the formation of gastropathy, gum ulceration, pancreatitis and aphthous stomatitis. Antispasmodics can cause the opposite effect - increase dizziness, headache, and also cause palpitations and more complex arrhythmias.
Recently, Botox injections have been used to relieve spasms. However, botuloxin is a strong poison; in addition to the unpredictable individual reaction of the body, it can cause headaches, muscle weakness up to paresis of some muscle groups, disruption of the gastrointestinal tract and respiratory system. With each repeated use, the effect of the drug decreases.
Neuroprotectors have a prolonged (long-lasting) effect, improving metabolism in brain tissue and thereby relieving pain. However, such drugs must be taken in long courses, but if used uncontrolled, they can cause dizziness, headaches, anxiety, increased blood pressure and arrhythmia.
It is important to remember that in this case, a headache is only a symptom of the disease. In addition to symptomatic care, it is necessary to direct efforts to fight the disease itself - the spine needs to be treated.
Conservative treatment of osteochondrosis, in addition to the use of painkillers and antispasmodics, should include the use of hydroprotectors, vitamin complexes, as well as exercise therapy and physiotherapy.
Electrophoresis is the most commonly used physiotherapy procedure. Its essence is a local increase in temperature and improvement of blood circulation, which relieves muscle spasms, eliminates pain and speeds up the healing process. In general, any thermal procedures relieve muscle spasms and improve blood circulation.
Magnetotherapy involves the use of low-frequency magnetic field inductors aimed at the problem area, which leads to local dilation of blood vessels, improved oxygenation and metabolism, accelerated elimination of toxins and reduced blood viscosity. Thanks to this, magnetic therapy has an anti-inflammatory, analgesic and anti-edematous effect.
Effective assistance in the treatment of osteochondrosis of the cervical spine can be provided by a modern drug - the therapeutic pain-relieving anti-inflammatory patch NANOPLAST forte.
Migraine - What is it?
This is an attack of severe throbbing (more often) headache. Migraine has a hereditary predisposition. Women suffer from it more often (5:1 with men). Sexual predilection is caused by female hormones – a decrease in progesterone and an increase in estradiol. The mechanism is based on a violation of vascular regulation and a disturbance in the exchange of neurotransmitters.
The pathology occurs in 3 phases:
- Constriction of blood vessels and the appearance of an aura (unpleasant sensations in the body that occur before an attack of pain). An aura does not always happen.
- Dilatation of large and small vessels. The level of serotonin decreases, the level of inflammatory mediators increases. A throbbing headache occurs.
- Swelling around the vessels due to the influx of inflammatory mediators. Decreased serotonin levels.
Migraine is provoked by emotional stress, strong physical exercise, fasting and alcohol, violation of the regime, etc.
How it manifests itself:
- The duration of paroxysmal throbbing pain lasts from 4 to 72 hours, often with loss of ability to work.
- localization of pain - often on one side of the head
- cephalalgia intensifies during physical or other stress;
- one of the symptoms is present: photophobia, nausea, vomiting, sound sensitivity.
A complication of migraine is status migraine. These are attacks of severe throbbing headaches that occur one after another without a pause. Status migraine can be complicated by cerebral infarction.
Migraines don't just happen to the head. Abdominal or abdominal migraine - severe throbbing pain in the abdomen. The pain alternates: first in the stomach, then in the head, then again in the stomach. This cephalalgia occurs in children 5-10 years old. Cephalgia in a teenager is often triggered by fasting or poor nutrition.
Cluster cephalgia
It is characterized by the sudden appearance of severe, cutting and burning pain in the head. Typical localization of pain is the frontal, temporal or zygomatic areas. Even more often, histamine cephalgia is localized around one eye. Sometimes the pain spreads to the entire half of the head or face. Men get sick. The onset of the disease often occurs at the age of 30 years.
Coital cephalalgia
From Latin “coitus” is translated as “sexual intercourse”. Cephalgia occurs during sex. Occurs if intercourse is accompanied by severe emotional shock or severe physical exertion.
Orgasmic cephalalgia
Headache at the time of orgasm is caused by increased blood pressure. The physiological mechanism of orgasmic headache exactly repeats the mechanism of headache of vascular origin due to arterial hypertension.
Vertebrogenic cephalgia
Develops as a result of pathologies of the cervical segment of the spine, especially as a result of osteochondrosis.
Post-traumatic cephalgia
Post-traumatic cephalgia is headaches that appear after physical trauma to the brain or skull. It can be acute or chronic. Acute occurs within 14 days after head injury and lasts no more than 8 weeks. Chronic post-traumatic cephalgia also occurs during the first
14 days after injury, but post-traumatic persistent cephalgia continues for more than 3 months. A type is post-traumatic encephalopathy with cephalgia. It occurs due to damage to brain tissue as a result of trauma, subsequently accompanied by headaches.
Post-puncture cephalgia
Pathology occurs 5 days after dural puncture. Post-puncture cephalgia is accompanied by rigidity of the neck muscles, tinnitus, retching and photophobia.
Cerebral angiodystonia with cephalgia
Occurs against the background of organic or functional disorders of cerebral vessels. The latter arise as a result of infections, injuries or diseases of internal organs.
Cephalgia due to dyscirculatory encephalopathy
DEP with cephalgia occurs due to impaired blood supply to the brain against the background of cerebral atherosclerosis or arterial hypertension.
Cephalgia during pregnancy
Occurs against the background of toxicosis of pregnant women, against the background of eclampsia or preeclampsia. The mechanism of headaches in this case is an increase in blood pressure.
Treatment of cervical osteochondrosis with a therapeutic plaster NANOPLAST forte
When treating cervical osteochondrosis, the NANOPLAST forte therapeutic plaster allows you to relieve pain and inflammation, improve blood circulation in the affected area, and relieve muscle spasms. Depending on the condition and severity of degenerative changes in the spine, the drug can be used both in monotherapy and in complex treatment of osteochondrosis. The use of the NANOPLAST patch in complex treatment allows you to reduce the dose of painkillers and anti-inflammatory drugs, enhance their effect, and speed up recovery processes.
The patch combines two types of physiotherapeutic effects - deep soft heating and magnetotherapeutic properties. Long-term exposure - for 12 hours - provides a high therapeutic effect of the drug.
When treating cervical osteochondrosis, the therapeutic plaster NANOPLAST forte is applied to the disturbing area of the neck, avoiding the anterior surface, especially the area of the carotid arteries and lymph nodes. A course of treatment of 9 days or more is recommended. It is usually recommended to use the patch in the morning for 12 hours, but it can also be used at night.
High efficiency, unique composition, long-term (up to 12 hours!) therapeutic effects, ease of use and affordable price make NANOPLAST forte the drug of choice in the treatment of cervical osteochondrosis.
Read more about NANOPLAST forte